Determine If The Fvc Is Low
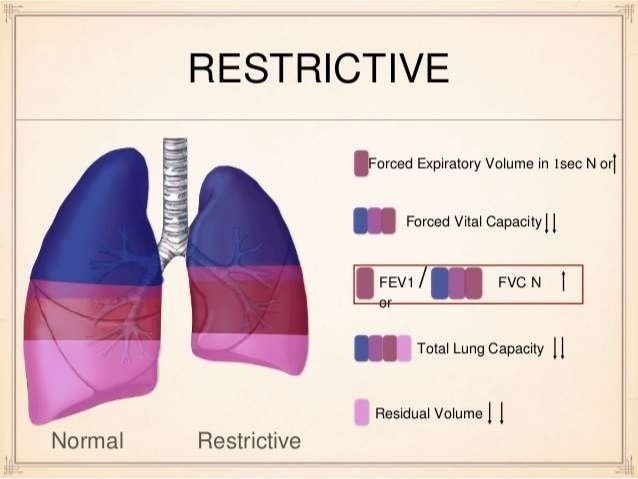
The physician must determine if the FVC is less than the LLN for adults or less than 80% of predicted for those five to 18 years of age, indicating a restrictive pattern.3,10,11 The LLN can be determined using the calculator at . A restrictive pattern can indicate restrictive lung disease, a mixed pattern , or pure obstructive lung disease with air trapping. Table 2 summarizes the first two steps of PFT interpretation.13,10,11
5 to 18 years: 80%
| Test results based on age | Suggested diagnosis | |
|---|---|---|
|
5 to 18 years: 85% |
Normal |
|
|
5 to 18 years: 80% |
5 to 18 years: < 85% |
Obstructive defect |
|
5 to 18 years: < 80% |
5 to 18 years: 85% |
Restrictive pattern |
|
5 to 18 years: < 80% |
5 to 18 years: < 85% |
Mixed pattern |
|
Adults: < LLN |
Adults: < LLN or < 70% |
FEV1 = forced expiratory volume in one second FVC = forced vital capacity LLN = lower limit of normal .
*The 70% criteria should be used only for patients 65 years and older who have respiratory symptoms and are at risk of chronic obstructive pulmonary disease .
Information from references 1 through 3, 10, and 11.
5 to 18 years: 80%
| Test results based on age | Suggested diagnosis | |
|---|---|---|
|
5 to 18 years: 85% |
Normal |
|
|
5 to 18 years: 80% |
5 to 18 years: < 85% |
Obstructive defect |
|
5 to 18 years: < 80% |
5 to 18 years: 85% |
Restrictive pattern |
|
5 to 18 years: < 80% |
5 to 18 years: < 85% |
Mixed pattern |
|
Adults: < LLN |
Adults: < LLN or < 70% |
Information from references 1 through 3, 10, and 11.
Treatments For Obstructive Lung Disease
Obstructive lung disease treatments work by helping to open narrowed airways. Airways may be narrowed by spasms in the smooth muscles that are in the wall of the airways .
Medicines that relax these smooth muscles and improve airflow are called bronchodilators, and are inhaled. These include:
- Combined medications like Combivent Respimat, DuoNeb, Anoro Ellipta, and Advair, which include a bronchodilator
Theophylline is a rarely used bronchodilator taken as an oral tablet.
Inflammation also contributes to airway narrowing in obstructive lung disease. Inflamed airway walls may be swollen and filled with mucus, obstructing airflow. Various medicines help reduce inflammation in obstructive lung disease, including:
- inhaled corticosteroids
- oral corticosteroids
- montelukast
A program of regular exercise will improve symptoms of breathlessness in virtually all people with obstructive lung disease. Oxygen therapy may be necessary for some people.
In severe cases of end-stage, life-threatening obstructive lung disease, lung transplantation can be considered as a treatment option.
Enhancing Healthcare Team Outcomes
The management of restrictive lung diseases can often be complex and challenging due to the many diseases that can result in the condition. For a primary care provider, knowing when to refer a patient to a pulmonologist can be extremely beneficial to the patient. Because of the long list of differential diagnoses and the complications of different conditions, a multidisciplinary approach is always recommended. Besides the primary care provider and pulmonologist, the team would also include nurses who would periodically assess the patients as well as internists and intensivists who would provide care in the inpatient setting according to the severity of the patient’s condition.
Cardiology evaluation should be obtained, especially if pulmonary restriction leads to signs of heart strain as it can potentially result in heart failure. Pharmacists are to be part of the team whenever specialty medications, including the newer anti-fibrotic agents, are used. Nutritionists should also be included in cases of obesity, and Neurologists should be involved in cases of neuromuscular disease. Transplant surgeons ought to assess end-stage patients who are candidates for transplant. Palliative and hospice care specialists should also be involved in cases where there is a terminal disease.
Also Check: How To Improve Your Lungs With Asthma
Inflammatory Cells In Copd
Neutrophils are present in sputum of smokers but increased in COPD and related to disease severity. They may be important in mucus hypersecretion and through release of proteases. Macrophages: big numbers are in airway lumen, lung parenchyma, and bronchoalveolar lavage fluid. They produce increased inflammatory mediators and proteases and may show defective phagocytosis. T lymphocytes: both CD4+ and CD8+ cells are increased in the airway wall and lung parenchyma, with big CD8+/CD4+ ratio. Increased is the number of CD8+ T cells and Th1 cells which secrete interferon- and express the chemokine receptor CXCR3. CD8+ cells may be cytotoxic to alveolar cells. B lymphocytes: are increased in peripheral airways and within lymphoid follicles, possibly as a response to colonization and infection. Eosinophils: increased eosinophil proteins in sputum and eosinophils in airway wall during exacerbations. Epithelial cells: May be activated by cigarette smoke to produce inflammatory mediators .
Treatment Options For Restrictive Lung Disease
Many forms of restrictive lung diseases are progressive which means they’ll become worse over time. However, there are available treatments based on the individual needs of the patient.
Some treatment options include:
1. Medications
A couple of FDA-approved medicines used for treating idiopathic pulmonary fibrosis are Ofev and Esbriet. Pulmonary fibrosis is a form of restrictive lung disease. There are other types of medications for reducing inflammation and suppressing the immune system.
These are:
Many patients use oxygen therapy to maintain their blood oxygen levels.
3. Cellular Therapy
For patients with certain restrictive lung disease types, like pulmonary fibrosis, pneumoconiosis, idiopathic pulmonary fibrosis or interstitial lung disease, cellular therapy is an option. It works by promoting healing within the patient’s lungs, possibly enhancing the function of their lungs and improving quality of life.
Under physician supervision, some patients have been able to decrease their use of oxygen therapy following treatment.
Recommended Reading: Sickness Induced Asthma
Diagnosis Of Obstructive Lung Disease And Restrictive Lung Disease
Most commonly, people with obstructive or restrictive lung disease seek a doctor because they feel short of breath.
Restrictive and obstructive lung diseases are identified using pulmonary function tests. In pulmonary function testing, a person blows air forcefully through a mouthpiece. As the person performs various breathing maneuvers, a machine records the volume and flow of air through the lungs. Pulmonary function testing can identify the presence of obstructive lung disease or restrictive lung disease, as well as their severity.
A doctor’s interview , physical exam, and lab tests may provide additional clues to the cause of obstructive lung disease or restrictive lung disease.
Imaging tests are almost always part of the diagnosis of restrictive and obstructive lung disease. These may include:
- Chest X-ray film
- Computed tomography of the chest
In some people, a bronchoscopy may be recommended to diagnose the lung condition causing obstructive or restrictive lung disease. In a bronchoscopy, a doctor uses an endoscope to look inside the airways and take samples of lung tissue .
Defining Obstructive Vs Restrictive
Obstructive lung disease is a condition where the airflow into and out of the lungs is impeded.1 This occurs when inflammation causes the airways to swell, making them narrower. Because of that, breathing well becomes harder and air often gets trapped in the lungs. This results in something known as hyperinflation of the lungs. Exhaling becomes slower and shallower than in a person with a healthy respiratory system.1
Examples of obstructive lung disease include:1
Restrictive lung disease is a condition where the lungs don’t function effectively. People with this cannot take a full, deep breath and fill their lungs with air. This can be due to problems within the lungs themselves or due to some kind of damage from external forces .1
With intrinsic disorders, the lungs’ restriction is related to weak muscles, stiffness in the chest wall or damaged nerves.1 Examples of these diseases include:1
- Interstitial lung disease
- Sarcoidosis
- Pneumoconiosis
With extrinsic disorders, other non-respiratory diseases end up causing problems with the function of the airways and lungs. These can include:1
- Obesity
Also, both obstructive and restrictive disease will be diagnosed by using a careful medical history and a variety of pulmonary function tests. The results of those tests and your history will help a doctor determine which type of lung disease you might have.1
Also Check: Forced Expiratory Wheeze
Determine If The Fev1/fvc Ratio Is Low
The first step when interpreting PFT results is to determine if the forced expiratory volume in one second/forced vital capacity ratio is low, indicating an obstructive defect. Physicians have two options to determine if this ratio is low.
The first option is to follow the GOLD criteria, which use a cutoff of less than 70%.2 For patients five to 18 years of age, the National Asthma Education and Prevention Program guideline says that a ratio of less than 85% is consistent with an obstructive defect as long as the patient has symptoms consistent with obstructive lung disease.1
The second option is to follow the ATS criteria, which use the lower limit of normal as the cutoff for adults.3 The LLN is a measurement less than the fifth percentile of spirometry data obtained from the Third National Health and Nutrition Examination Survey . Most modern PFT software can calculate the LLN. Alternatively, the calculator at can be used for adults up to 75 years of age. Although the U.S. Food and Drug Administration has not approved this calculator for clinical use, it appears to be accurate and valid.
Chronic Obstructive Pulmonary Disease
Chronic obstructive pulmonary disease , previously known as chronic obstructive airways disease or chronic airflow limitation , is a group of illnesses characterised by airflow limitation that is not fully reversible. The flow of air into and out of the lungs is impaired. This can be measured with breathing devices such as a peak flow meter or by spirometry. Most people with COPD have characteristics of emphysema and chronic bronchitis to varying degrees. Asthma being a reversible obstruction of airways is often considered separately, but many COPD patients also have some degree of reversibility in their airways.
In COPD, there is an increase in airway resistance, shown by a decrease in the forced expiratory volume in 1 second measured by spirometry. COPD is defined as a forced expiratory volume in 1 second divided by the forced vital capacity that is less than 0.7 . The residual volume, the volume of air left in the lungs following full expiration, is often increased in COPD, as is the total lung capacity, while the vital capacity remains relatively normal. The increased total lung capacity can result in the clinical feature of a barrel chest a chest with a large front-to-back diameter that occurs in some individuals with emphysematous COPD. Hyperinflation can also be seen on a chest x-ray as a flattening of the diaphragm.
Also Check: Can A Humidifier Help With Asthma
Is Copd Restrictive Or Obstructive
In cases of obstructive lung diseases, such as asthma, bronchiectasis, COPD, and emphysema, the lungs are unable to expel air properly during exhalation. Restrictive lung diseases, on the other hand, mean the lungs are unable to fully expand, so they limit the amount of oxygen taken in during inhalation.
Furthermore, what is the difference between restrictive and obstructive lung disease?
While both types can cause shortness of breath, obstructive lung diseases cause more difficulty with exhaling air, while restrictive lung diseases can cause problems by restricting a person’s ability to inhale air.
Beside above, how serious is restrictive lung disease? In some cases, treating an underlying cause of lung restriction, such as obesity or scoliosis, can slow or reverse the progression of the disease. When restrictive lung disease is caused by a lung condition, however, it is usually difficult to treat and eventually fatal.
Herein, what is a restrictive lung disease?
Restrictive lung diseases are a category of extrapulmonary, pleural, or parenchymal respiratory diseases that restrict lung expansion, resulting in a decreased lung volume, an increased work of breathing, and inadequate ventilation and/or oxygenation.
What causes restrictive airway disease?
Some conditions causing restrictive lung disease are:
You May Like Also
What Are Obstructive Diseases
Say you swallow a hotdog. But, it doesnt travel down your esophagus to your stomach. Instead, it goes down your airway. At some point it will get stuck. So, its the most basic form of obstruction. This hotdog may completely block your airway making you unable to breathe.
But, if it gets lodged just right, you may still be able to breathe. Air can get in past this hotdog obstruction, but it will have a hard time getting out. So, when you have an obstruction, air can get in but has a hard time getting back out.
When you exhale, the obstruction resists the flow of air. So, it causes increased resistance to the flow of air. So, it may seem you can exhale forever and never get all your air out. Air is therefore slowed when you exhale. A medical term for this is airflow limitation. It is this that makes you feel short of breath.
There are diseases that may obstruct airways. Chronic bronchitis fits into this category. Asthma also fits into it. They both cause inflammation and increased sputum that make airways narrow. So, they both obstruct airways. They are obstructive diseases.1-5
Obstructive Sleep Apnea causes your upper airway to collapse while your sleeping. So, it obstructs the flow of air. Croup causes inflammation of your upper airways. So, its certainly an obstructive disease. Rhinitis causes inflammation in your nasal passages. So, it also qualifies. 5
Cystic fibrosis, emphysema, and bronchiectasis also qualify.5
You May Like: Side Effects Of Short Acting Beta Agonists
How Are These Conditions Treated
Obstructive lung conditions like asthma are generally treated with medications that open your airways and reduce inflammation.
Your exact treatments will depend on the severity of your asthma or other obstructive lung disease and on how well you respond to initial treatments.
Since most obstructive lung diseases are chronic, treatments will not cure your condition, but they will help you better manage your symptoms.
Causes Of Obstructive Lung Disease
The primary risk factor for this condition, according to the National Heart, Lung and Blood Institute, is smoking. More than 75% of individuals with COPD either currently smoke or they used to.
Exposure to environmental lung irritants can also lead to obstructive lung disease.
Some types of lung irritants are:
- Dust
- Chemicals
- Excessive secondhand smoke exposure
There’s also a genetic element to this condition. Individuals could develop all forms of obstructive lung disease without having substantial environmental irritant exposure or without ever having smoked.
Scientists have also found genetics can play a role in developing the condition.
For instance, some individuals have an alpha-1 antitrypsin deficiency which is a common genetic emphysema risk.
Read Also: How To Calm Down Asthma Symptoms
Treatment Options For Obstructive Vs Restrictive Lung Disease
Treatment options will be somewhat different for these two types of respiratory illness.1 With obstructive lung disease, the goal is to reduce inflammation and relax the airways. So, treatments might include bronchodilators and/or inhaled steroids. Some medications are long-acting and some are shorter-acting.1
In addition, with COPD, supplemental oxygen therapy might be helpful. This is not generally prescribed in people who have asthma. Changes in lifestyle may also be helpful. For example, with asthma, learning to avoid your triggers can help keep your asthma under control.1
With restrictive lung disease, the treatment options are often more limited. They may also vary greatly, depending on the specific type of restrictive disease. Steroids and bronchodilators are sometimes used. Medications that suppress the immune system may also be helpful.1 Other options might include supportive oxygen therapy and even lung transplants.1
Compare Current And Prior Pft Results
If a patient’s prior PFT results are available, they should be compared with the current results to determine the course of the disease or effects of treatment.
Data Sources: We conducted literature searches using Ovid, PubMed, the Cochrane database, and Essential Evidence Plus, focusing on the keywords spirometry and pulmonary function test, with an emphasis on the diagnosis and/or interpretation of results. The section on DLCO was reviewed in UpToDate in October 2011 to identify additional primary literature regarding this test. Search dates: September to October 2011, May 2012, and August 2013.
Read the full article.
- Get immediate access, anytime, anywhere.
- Choose a single article, issue, or full-access subscription.
- Earn up to 6 CME credits per issue.
Also Check: Naproxen Asthma
Symptoms Of Restrictive Lung Disease
There are a few common symptoms with the most common being shortness of breath. In the early stages, a patient might experience shortness of breath only with exertion. As the condition progresses, the patient might begin to experience breathlessness or shortness of breath even during rest or minimal activity.
Chronic cough is another common symptom. Often the cough is dry, but it could also create white sputum. Fatigue and weight loss are also common symptoms. Many individuals find it difficult to have sufficient energy to function well and maintain a healthy weight.
Some individuals with this condition may experience symptoms of anxiety and depression. These symptoms are more common when the condition has progressed sufficiently to cause substantial limitations.
Causes Of Restrictive Lung Disease
This condition often results from disorders that cause lung stiffness. In other cases, weak muscles, stiffness of the chest wall or damaged nerves could be causing the lung expansion restriction.
You can categorize restrictive lung diseases as intrinsic or extrinsic.
Intrinsic disorders come from an issue within the lungs themselves. They might include:
- Pulmonary fibrosis
- Pleural Effusion
Recommended Reading: Asthma Lung X Ray
What Are Restrictive Diseases
These are diseases that occur outside your airways. The best example I can think of here is pregnancy. Its not a disease, but it certainly does restrict your airways. You have a baby inside you. It grows larger and larger. At some point, it begins to push up on your diaphragm.
It acts to squeeze or restrict your lungs. This makes it so your lungs are less compliant. This means they are unable to fully expand because of the baby taking up space. So, thats the most basic form of a restriction.
Obstructive diseases make it hard to exhale. Restrictive diseases make it hard to inhale. They cause less lung compliance. Another good example is kyphoscoliosis. People with this have deformed chest walls. This acts to limit the ability of the lungs to expand. Rheumatoid arthritis may also qualify.1,4,5
Neuromuscular diseases like ALS may impact inspiratory muscles. So, this can make it hard to inhale. Drug overdoses qualify here. They relax you so you weaken your drive to inhale.1,3
Pneumonia is inflammation of your alveoli. So, it takes up space making it hard to inhale. Obesity certainly may cause less room for lungs to expand, so it qualifies. Lung cancer takes up space outside airways, so it qualifies. 5
