How Should We Prepare For Spirometry
You can help prepare your child for spirometry by explaining the importance of following the instructions of the person giving the test.
Before the test, your child should avoid cold medicines, caffeine, carbonated beverages, and exposure to tobacco smoke. Your child also shouldn’t eat a big meal before the test.
The doctor might have your child stop taking any regular medicines for a bit before the test. Your child may be asked to practice for the test, such as by pretending to blow out birthday candles or blowing air at a pinwheel.
On the day of the test, make sure that your child doesn’t wear tight clothing that could interfere with being able to breathe in and out deeply.
p1
Restrictive Pattern On Spirometry
With a restrictive spirometry pattern your FVC is less than the predicted value for your age, sex and size. This is caused by various conditions that affect the lung tissue itself, or affect the capacity of the lungs to expand and hold a normal amount of air. Conditions that cause scarring of the lungs give restrictive patterns on spirometry. Some physical deformities that restrict the expansion of the lungs can also cause a restrictive defect. Your FEV1 is also reduced but this is in proportion to the reduced FVC. So, with a restrictive pattern the ratio of FEV1/FVC is normal.
What Are Other Conditions A Doctor Might Test For In Someone With Asthma
There are some medical conditions that might make asthma harder to treat and control. Two of these conditions are and gastroesophageal reflux disease, commonly called GERD and known as heartburn. If you are diagnosed with asthma, your doctor might also test you for these conditions so that they can be treated.
Sinusitis, also called sinus infection, is an inflammation or swelling of the sinuses due to infection. When the sinuses become blocked and filled with fluid, bacteria grow, causing infection and inflammation. Your doctor might order a special X-ray, called a CT scan, to evaluate your sinuses if he or she suspects an infection. Once acute sinusitis is diagnosed, you will be treated with antibiotics for at least 10 to 12 days.
Comorbidities And Risk Factors
Both for adults and children, the detection of potentially modifiable risk factors for exacerbations may be useful in asthma monitoring and includes the exposure to specific allergens, smoking, high SABA use, poor adherence to therapy and incorrect inhaler technique. As already mentioned, GINA guidelines state that a previous sever exacerbation in last 12 months and a history of access into an intensive care or intubation are major independent risk factors for exacerbations .
Moreover, the asthma monitoring cannot be separated from an early identification and management of associated comorbidities .
What Are The Risks
During the test, breathing fast and hard can make you feel tired, dizzy, or light-headed; cause coughing; or lead to chest tightness or pain. Tell the technologist if you have any discomfort.
Tell your provider if you have:
- Had a heart attack within the past month
- Had recent eye, chest, or abdominal surgery
- A collapsed lung
- Tuberculosis
If you had any of these, your provider may wait until you recover before doing the testing.
These Two Graphs Show:
- peak expiratory flow volume loop when breathing in and out
- volume / time.
The table below the graphs shows the normal range of values for
- forced expiratory volume . Thats the volume of air breathed out in one second, measured in litres
- forced vital capacity . Thats the total volume of air breathed out in one breath, measured in litres
- vital capacity . Thats the total volume of air you can breathe out when relaxed, measured in litres
- the percentage of air blown out in the first second. This is calculated by dividing your FEV1 by your VC and multiplying by 100. In normal, healthy lungs, this will be 70% or above.
If your best effort is below the minimum value , your result is below what it is expected it to be. This information and the shape of the loop will help your health care professional understand your results.
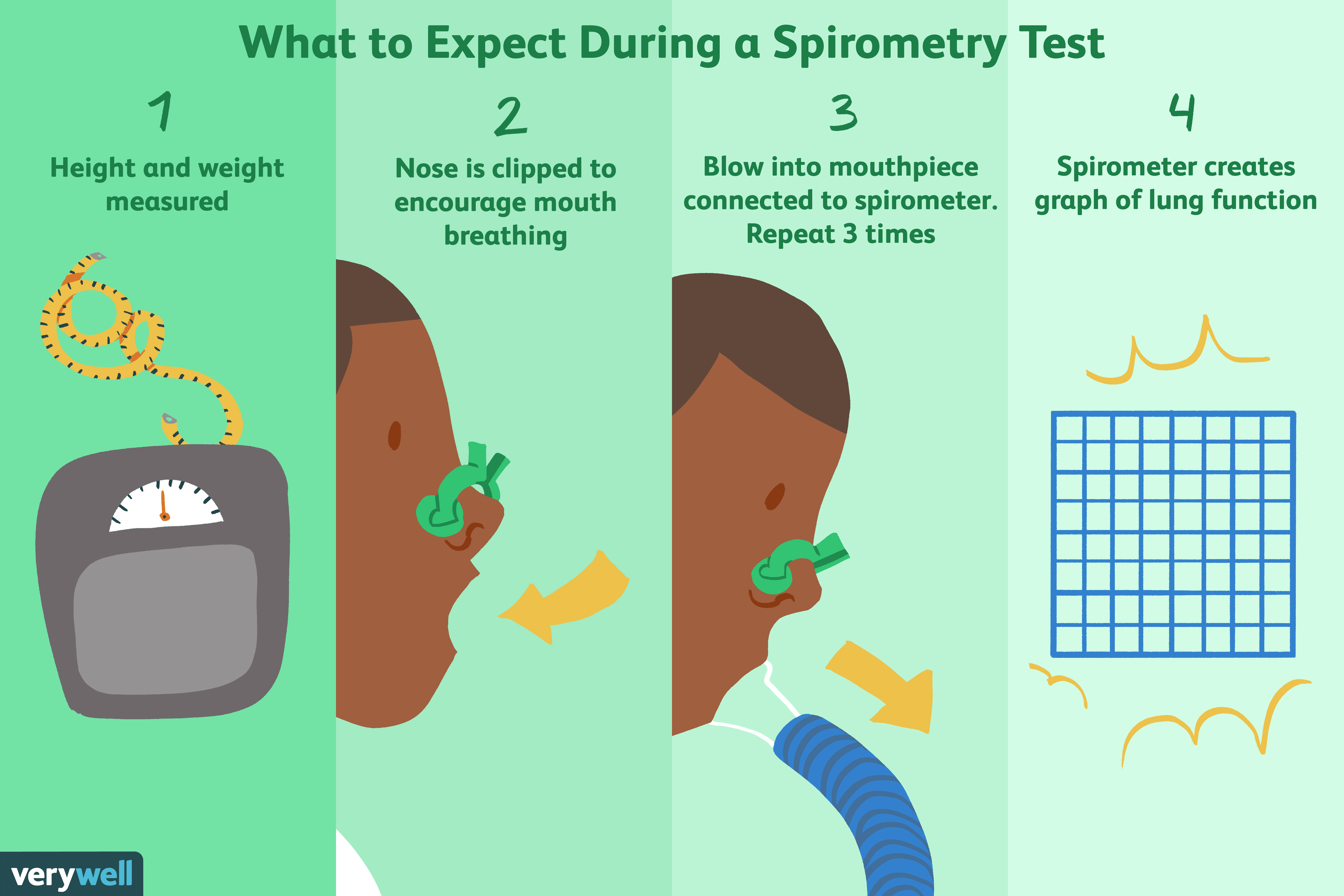
How Is A Spirometry Test Performed
Spirometry only takes about a half hour to 45 minutes to complete. Youll sit upright for the whole test.
First, the technician will place a clip on your nose. This helps you breathe through your mouth.
Then, you will clamp your lips around the mouthpiece connected to the spirometer. Follow the technicians instructions on how to breathe. Youll inhale as deeply as you can then exhale as quickly and forcefully as you can. Use as much energy and effort as possible when you breathe in and out. That gets the most accurate results. Youll repeat this at least three times.
Your technician may give you a medication called a . It opens your airways. About 15 minutes later, you will do the test again to see if there are any changes in your results. Comparing the results before and after you take a will show whether this medicine helps you.
During the test, some people feel lightheaded or dizzy, , or feel chest tightness. If you feel uncomfortable, tell the technician.
After the test is over, you can get back on your regular medication schedule.
Food Drink And Medications
Little preparation is required before having a spirometry test. However, your doctor may advise you to:
- Eat lightly: If your stomach is too full, it may be harder to take deep breaths and you may end up vomiting.
- Avoid alcohol before the test: You may not be able to breathe as well if you have alcohol in your system.
- Check that your medications won’t interfere with the test: Certain drugs can affect breathing, particularly inhaled . Avoid short-acting inhalers six to eight hours before testing unless you really need them .
Is Spirometry The Same As Peak Flow Readings
No. A peak flow meter is a small device that measures the fastest rate of air that you can blow out of your lungs. Like spirometry, it can detect airways narrowing. It is more convenient than spirometry and is commonly used to help diagnose asthma. Many people with asthma also use a peak flow meter to monitor their asthma. For people with COPD, a peak flow reading may be useful to give a rough idea of airways narrowing; however, it can underestimate the severity of COPD. Therefore, spirometry is a more accurate test for diagnosing and monitoring people with COPD.
How The Test Is Performed
Spirometry measures airflow. By measuring how much air you exhale, and how quickly you exhale, spirometry can evaluate a broad range of lung diseases. In a spirometry test, while you are sitting, you breathe into a mouthpiece that is connected to an instrument called a spirometer. The spirometer records the amount and the rate of air that you breathe in and out over a period of time. When standing, some numbers might be slightly different.
For some of the test measurements, you can breathe normally and quietly. Other tests require forced inhalation or exhalation after a deep breath. Sometimes, you will be asked to inhale a different gas or a medicine to see how it changes your test results.
Lung volume measurement can be done in two ways:
- The most accurate way is called body plethysmography. You sit in a clear airtight box that looks like a phone booth. The technologist asks you to breathe in and out of a mouthpiece. Changes in pressure inside the box help determine the lung volume.
- Lung volume can also be measured when you breathe nitrogen or helium gas through a tube for a certain period of time. The concentration of the gas in a chamber attached to the tube is measured to estimate the lung volume.
How The Test Will Feel
Since the test involves some forced breathing and rapid breathing, you may have some temporary shortness of breath or lightheadedness. You also might have some coughing. You breathe through a tight-fitting mouthpiece and you will have nose clips. If you are claustrophobic, the part of the test in the closed booth may feel uncomfortable.
Follow instructions for using the mouthpiece of the spirometer. A poor seal around the mouthpiece may cause results that aren’t accurate.
Fractional Exhaled Nitric Oxide
As already mentioned, the detection of different asthma phenotypes guided the scientific community searching for specific biomarkers that could guide and improve the disease monitoring and the therapeutic approach. The monitoring of asthma should also include the determination of minimally invasive inflammatory markers.
Fractional exhaled nitric oxide measurement correlates with eosinophilic airway inflammation and therefore with the most common asthma endotype, independently of gender, and age. FeNO levels are higher in asthmatic children compared to non-asthmatic children and in one study values rose further during exacerbations and rapid decline after oral steroid treatment . British guidelines recognize that a FeNO <20 ppb in children under 12 years may have a role in identifying patients who can step down corticosteroid treatment . This relationship is lost in adults smokers .
Two recent Cochrane reviews, including both pediatric and adulthood studies, showed that tailoring asthma medications based on FeNO levels decreased the frequency of asthma exacerbations but did not impact on day-to-day clinical symptoms or inhaled corticosteroid dose .
In conclusion, FeNO role in asthma management has not been concretely proven due to incomplete evidence therefore it is not routinely recommended in all patients, at least in monitoring, even though it may be useful in subjects who respond poorly to inhaled corticosteroids .
What Happens During The Test

You will be asked some questions before you start, to check you are medically fit to do the test. It is important to put as much effort into the test as you can, so the results are accurate.
Youll be asked to sit comfortably and may have a clip put on your nose to make sure all the air goes into the mouthpiece. You will be shown how to blow into the spirometer before starting. You may be asked to blow 3 or more times into the spirometer, to check the readings are similar each time.
Normally, you will first be asked to breathe in deeply and out gently. Once your health care professional is happy with the results, you will move on to the next part of the test. You will have to breathe in again deeply, this time quite fast, and then breathe out as fast and as hard as you can until your lungs are empty.
Your health care professional may ask you to use your inhaler or other medication, wait 1520 minutes and then repeat the test. For some drugs the wait may be 45 minutes between tests. This is called a bronchodilator responsiveness test or reversibility test and its done to see if the medication improves your breathing. If you use inhalers, you should bring them to your appointment.
Occasionally, people feel a little light-headed and dizzy following the test. This usually lasts only a few moments. Let the person performing the test know, to make sure that you have time to recover.
What Happens During A Spirometry Test
You’ll be seated during the test and a soft clip will be placed on your nose to stop air escaping from it.
The tester will explain what you need to do, and you may be asked to have a few practise attempts first.
When you’re ready for the test, you’ll be asked to:
- inhale fully, so your lungs are completely filled with air
- close your lips tightly around the mouthpiece
- exhale as quickly and forcefully as you can, making sure you empty your lungs fully
This will normally need to be repeated at least 3 times to ensure a reliable result.
Sometimes, the test may need to be repeated around 15 minutes after taking some inhaled bronchodilator medicine.
This can show if you have a lung condition that responds to these medicines.
Overall, your appointment should last around 30 to 90 minutes. You’ll be able to go home soon after the tests have finished and return to your normal activities.
How Is Spirometry For Asthma Done
The test may be performed standing or sitting. You may be asked to wear nose clips or pinch your nose shut.2 You will be asked to breathe into a mouthpiece that is attached to a device called the spirometer.
There are three phases of the test: taking the deepest breath possible, followed by blasting air out of the lungs as rapidly as possible, and then continuing to breathe out for as long as possible.2,3 You will be asked to do this at least three times to get a valid test. The attempt does not count if you cough, if there is a delay in exhaling, or if you stop breathing too early. It could take up to eight attempts to get a valid test.2
A valid test requires a lot of effort from you! The technician will encourage you and provide instructions throughout the test. The test can be tiring and uncomfortable. You may feel light headed or dizzy.1 You can take a break between attempts. Giving it your best effort is important so that the results lead to the right .
The test may be repeated after you take a medication that opens your airways, called a bronchodilator. Albuterol is the medication typically used. Fifteen to 30 minutes after taking the medication, you will be asked to do spirometry again.4 This step is done to see if the airway blockage is reversible.
Are There Any Risks From Spirometry
Spirometry is considered a safe procedure with little risk. Because the test requires kids to breathe quickly and deeply, some may have temporary shortness of breath or lightheadedness. This test shouldn’t be done on kids who have chest pain, a recent history of eye or abdominal surgery, or serious heart disease.
What Is Spirometry
Spirometry is the most important test to diagnose and monitor COPD.
COPD causes narrowing of the bronchial tubes , resulting in shortness of breath. The greater the narrowing, the more difficult breathing becomes. Spirometry is a test which measures exactly how much the bronchial tubes have narrowed. The spirometer measures the speed your lungs can be filled and emptied of air, giving an indication of how well your lungs are performing. This enables your doctor to make decisions about your lung condition and to plan the best treatment for you. Further spirometry tests later on can help decide whether treatments should be continued, changed, or are no longer needed.
What Is A Chest X
An X-ray is an image of the body that is created by using low doses of radiation reflected on special film or a fluorescent screen. X-rays can be used to diagnose a wide range of conditions, from to a broken bone. Your doctor might perform an X-ray exam on you in order to see the structures inside your chest, including the heart, lungs, and bones.
The Importance Of Training And Experience
Training and experience are required for interpreting spirometry indices. There are well-established normal values for spirometry based on ethnicity, age, sex, and height. However, airflow obstruction may be underdiagnosed in younger people and overdiagnosed in older people if absolute cut-off values of 70% rather than lower limits of normal for FEV1/FVC are used. Furthermore, normal values are much higher in children than in adults. A lack of skill in interpretation of results, and availability of trained staff and equipment, limits the universal usefulness of spirometry.
For PEF, diagnosis of variable airflow obstruction requires simple arithmetic calculations. The upper 95% confidence limit of diurnal variability from twice-daily readings is 9% in healthy adults, and 12.3% in healthy children. The presence of diurnal variability >10% for adults and >13% for children is regarded as excessive and indicative of asthma. PEF is widely used in case finding and diagnosing occupational asthma.,
Airflow obstruction in asthma is worse during the night and early morning, so lung function indices obtained during office hours may not accurately reflect variability. When spirometry is normal in people with suspected asthma, a pragmatic alternative is to provide a peak flow meter and instructions to record the best of three readings twice a day, when symptoms occur, and if appropriate, in combination with a trial of treatment. This should be followed by a review a few weeks later.
What Happens Next
The test measures a few different variables. Two common tests are the FVC and the FEV. The most important is the FEV which means the forced expiratory volume and the FVC which means the forced vital capacity. For an FVC value in children, anything that is less than 80% should be considered abnormal and get treated right away. In adults, anything less than the lower limit of normal should be a red flag. Doctors look at these numbers together to see essentially how well a patients lungs are functioning as compared to other people with similar ages, weight, gender and other ranges.
The asthma spirometry test will determine the course of action a doctor takes. This will help determine what types of medicine may be necessary to ensure proper lung health treatment and function.
What To Expect

On the day of the test, you may be asked to not use certain inhalers or medications. Wear loose clothing and avoid big meals before testing.These tests are not painful. They are performed by a pulmonary function technician. The tests are repeated several times to make sure the results are accurate. When performing the test, keep the following in mind:
- You should take your daily medications prior to testing unless told otherwise.
- Do not smoke for at least six hours prior to testing.
- If you are taking a short-acting inhaler that is used only as needed, do not use for six to eight hours prior to testing, if possible.
- Your doctor may give you other instructions regarding medications.
During the test, you will be sitting upright. A clip is placed on your nose and you will be given a plastic mouthpiece connected to the spirometry machine. You will place your lips tightly around the mouthpiece and be asked to take in as big and deep a breath as possible and then blow out as hard and fast as you can. This maximal effort is very important, and testing will be repeated at least three times to get the best results.
The technician may give you a medicine to help open your airways and then repeat the test to see if your breathing improves with the medicine. The testing takes about 30 to 45 minutes.
How Is It Done
The image below is of a portable spirometer.
A clip may be put on to your nose to make sure that no air escapes from your nose. The measurements may be repeated two or three times to check that the readings are much the same each time you blow into the machine. Sometimes the tests are performed with you in a separate glass cubicle – this can help to obtain more detailed and precise results.
Spirometry
- 2min
When Should You Have A Spirometry Test
Children older than age five, and adults of any age, who have asthma-like symptoms should have a spirometry test. The healthcare provider should also do a physical exam and a full medical history. If the test shows that you have asthma, your doctor should prescribe asthma medicine. Then you should be retested four to six weeks later. If your test results improve, your treatment is working. You may even be able to take less medicine. If your symptoms get worse, you should have another spirometry test. If your symptoms are controlled, you should have a test at least once every year or two.
This report is for you to use when talking with your healthcare provider. It is not a substitute for medical advice and treatment. Use of this report is at your own risk.
© 2016 Consumer Reports. Developed in cooperation with the American Academy of Allergy, Asthma & Immunology.
02/2014
What Do Spirometry Results Say About Your Asthma
Read our privacy policyThe information provided on our website is not intended to replace professional medical or healthcare advice. It is our aim to help make certain health-related information more readily available and useful to you, however, our website cannot and does not guarantee health-related improvements or outcomes. Any information provided to you by, or linked to from, our website, does not constitute medical advice, diagnosis or treatment, nor you should rely on that output as medical advice, diagnosis or treatment. You should always talk to a qualified medical or healthcare professional about any medical conditions. Any decisions you take affecting your health should always be made in consultation with a qualified medical professional. You should not rely on the information set out on our website as your primary tool for making health-related decisions.Asthma UKNOTE– Spirometry results are not often available immediately after a test.
What Preparation Is Needed Before Having Spirometry
You should receive instructions from the doctor, nurse, or hospital department that does this test. Always follow these carefully. The instructions may include such things as not to use a bronchodilator inhaler for a set time before the test . Also, not to have alcohol or a heavy meal, or do vigorous exercise for a few hours before the test. Ideally, you should not smoke for 24 hours before the test.
How To Prepare For Your Test
- No smoking one hour before the test
- No alcohol within four hours of test
- Do not eat a large meal within two hours of test
- Wear loose, comfortable clothing
- Avoid vigorous exercise 30 minutes prior to testing
- If you are currently prescribed inhalers/puffers, you may be asked to avoid taking them a few hours before spirometry. Ask your doctor beforehand if this applies to you.
The Test Can Save Money
A spirometry test generally costs less than $100. Not having the test can cost a lot more money. If the test shows that you do not have asthma, this can save you hundreds of dollars a month for asthma medicines. If you do not have the test and you have asthma, an emergency room visit for an asthma attack can cost thousands of dollars.
What Happens In A Spirometry Test
Spirometry is a painless test that can often be done in your doctors office or in a nearby clinic. The entire test usually takes less than 10 minutes, although sometimes it is repeated after taking a puffer medication.
How to prepare for the test:
- Do not smoke for one hour before test
- Do not drink alcohol within four hours of test
- Do not eat a large meal within two hours of test
- Please wear loose clothing
- Do not perform vigorous exercise within 30 minutes of test
- If you are on puffer medications, you may be asked to not take them for a few hours before spirometry. Ask your doctor beforehand if this applies to you.
How Is A Physical Exam Used In The Diagnosis Of Asthma

The doctor will watch the way your chest and stomach muscles move when you breathe and use a stethoscope to listen to air flowing in and out of your lungs.
The doctor will look inside your nose, searching for signs of conditions that often go along with asthma, such as rhinitis , sinusitis and nasal polyps , and examine skin for signs of eczema .
Understanding Spirometry And Narrow Airways
Think of a 5-lane motorway that has been reduced to 3 lanes due to roadworks. The traffic will take longer to travel through that stretch of motorway.
In the same way, if your airway is narrower than normal, it will take you longer to empty your lungs of air.
A spirometer records how much air you can breathe out in one second. That will be less if your airways are narrower than someone of your sex, age, height and ethnicity with healthy airways. It can also compare that result to how much air you breathed out, to measure how much your airways are blocked. In someone with healthy airways, at least 70% of the total air they breathe out would be breathed out in one second.
An example of a spirometry result for a hospital spirometer
