Prioritization Of Canadians With Lung Disease In Covid
Joint Statement on Prioritization of Canadians with Lung Disease in COVID-19 Rollout
As part of the Canadian Thoracic Societys COVID-19 Respiratory Roundtable panel representing Canadians living with lung disease, Asthma Canada signed a joint statement titled Prioritization of Canadians with Lung Disease in COVID-19 Vaccination Rollout. Alongside other lung health organizations, Asthma Canada is urging federal, provincial and territorial governments to prioritize people living with lung disease who are at higher risk for more serious COVID-19 complications in the vaccination rollout. From Canadians living with a lung disease such as asthma, chronic obstructive pulmonary disease , cystic fibrosis, lung cancer, pulmonary fibrosis, pulmonary hypertension, and pre- and post-lung transplant, there is widespread concern regarding when in the vaccine rollout in the provinces and territories they will have the opportunity to receive the vaccine.
We will continue to advocate for our community on this subject and will share more information as it becomes available.
Canadians living with pre-existing conditions such as a lung disease and their caregivers have faced heavy burdens throughout the pandemic.
This is why alongside a roundtable of organizations who represent and work closely with Canadians living with these diseases, were urging governments across Canada to prioritize these individuals in COVID-19 vaccination programs.
Read our joint statement below.
Asthma Vs Copd: What’s The Difference
It is no surprise that asthma and chronic obstructive pulmonary disease are often mistaken for one another they are both conditions that affect the lungs and make breathing more difficult. Despite their many similarities, asthma and COPD are not the same. In honor of November being National COPD Awareness Month, it is time to finally clear up the question of whether asthma and COPD are the same thing.
Below, we will look at the definitions of the two diseases, along with the symptoms, causes and treatments for each. We will also discuss when to see a medical professional for lung damage to help raise COPD awareness this month.
Staging And Treatment Of Chronic Obstructive Pulmonary Disease
The stages of COPD are defined primarily by lung function . This emphasises the important clinical message that the diagnosis of COPD requires the measurement of lung function. The stages of COPD suggested in the GOLD Guidelines are as follows. Stage 0: At risk, cough or sputum present but lung function normal. Stage 1: Mild COPD, FEV1/forced vital capacity <70%, with an FEV1 â¥80% predicted, with or without chronic symptoms. Stage 2: Moderate COPD, FEV1/FVC <70% and FEV1 % pred>30% and <80%. Stage 2 is split at an FEV1 of 50% pred since the existing data support the value of inhaled corticosteroids below an FEV1 of 50% pred but not above. Stage 3: Severe COPD, FEV1<30% pred and FEV1/FVC <70%.
In the GOLD guidelines, Stage 0 is a newly defined stage that was included to give a strong public health message that symptoms of chronic cough and sputum production should alert the clinician to the presence ofan ongoing pathophysiological process even when lung function is normal. This may progress to clinically significant COPD in a proportion of those exposed . The analogy that is perhaps most relevant is that mild hypertension in some but not all , with mild elevation of blood pressure will progress to clinically significant hypertension.
The Anatomy Of The Lung
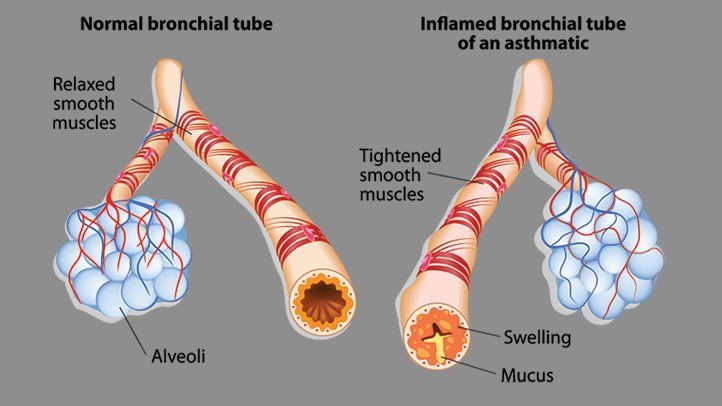
A quick review of lung anatomy may prove helpful here. Inside your chest is a set of lungs. When you take in a breath, air enters in your nose or mouth. The back of your nose or mouth is your pharynx. From there air enters your larynx and passes through your vocal cords. It then enters your bronchial airways.
Bronchial airways get smaller and smaller the further down you go. They continue getting smaller all the way to the terminal bronchioles. Air then passes to your respiratory bronchioles. These are surrounded by balloon-like sacs called alveoli. Alveoli are grouped together in grape-like clusters.
Respiratory bronchioles and alveoli are interconnected with small blood vessels. These are called capillary blood vessels. So, its here where gas exchange occurs. When you exhale air goes back all the way up and leaves your mouth or nose.
Clinical Recognition And Inflammatory Features Of The Overlap Syndrome: What Is It
The clinical recognition of both asthma and COPD requires assessment of symptoms and physiological abnormalities . Symptoms can indicate the presence of a disease process; however, their sensitivity and specificity for asthma or COPD may be limited. At a physiological level, patients with overlap syndrome have evidence of incompletely reversible airflow obstruction that can be detected by a reduced postbronchodilator FEV1 . In addition, they have increased variability of airflow, which can be determined by increased bronchodilator responsiveness or BHR. The presence of airflow obstruction can confound the assessment of BHR in COPD. For recognition of the overlap syndrome, it may be preferable to use an indirect acting stimulus to assess BHR. Such agents do not directly cause airway smooth muscle contraction, and include hypertonic saline, adenosine and mannitol.
Informative data can be obtained from studies of discrete patient groups who have features of asthma and COPD. These groups include patients with asthma who smoke, those with asthma who develop incompletely reversible airflow obstruction and non-smokers who develop COPD. Smokers with asthma have features resembling COPD, since they are less responsive to corticosteroids and are less likely to have eosinophilic inflammation and more likely to have increased airway neutrophilia.
What Are The Different Types Of Copd
The two most common conditions of COPD are chronic bronchitis and emphysema. Some physicians agree that asthma should be classified as a chronic obstructive pulmonary disease, while others do not. A brief description of asthma, is included below:
| 1
What is chronic bronchitis?Chronic bronchitis is a long-term inflammation of the bronchi , which results in increased production of mucus, as well as other changes. These changes may result in breathing problems, frequent infections, cough, and disability. |
1
What is pulmonary emphysema?Emphysema is a chronic lung condition in which alveoli may be:
This can cause a decrease in respiratory function and breathlessness. Damage to the air sacs is irreversible and results in permanent “holes” in the lung tissue. |
1
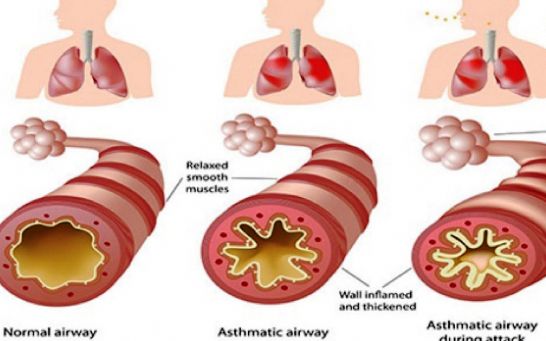
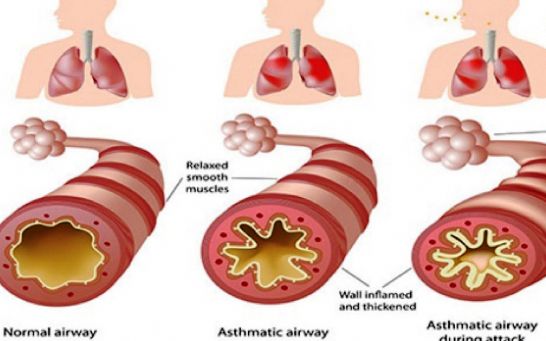
What is asthma?Asthma is a chronic, inflammatory lung disease involving recurrent breathing problems. The characteristics of asthma include the following:
|
Exacerbation/infection: Changes In Inflammatory Features And Cytokine Profiles
Exacerbations of asthma and COPD are clinically significant events. They are frequently triggered by viral infections of the airways and are associated with a decline in lung function and symptomatic aggravation. During exacerbation, airway inflammation becomes more exaggerated than in the mild and stable disease states, and the inflammation pattern changes. Neutrophil recruitment is a prominent feature of acute exacerbation of chronic asthma, probably owing to respiratory tract infection by viruses., Furthermore, neutrophilic inflammation in the absence of eosinophils is largely present in sudden-onset fatal asthma, and neutrophil numbers are highly elevated in status asthmaticus., Thus, severe and fatal asthma may be mediated by neutrophils, which is quite different from the classical Th2-driven eosinophilic form of the disease. In COPD patients, an allergic profile of inflammation can occur, particularly during exacerbation. Airway eosinophilia is observed in chronic bronchitic patients with exacerbation and is associated with the upregulation of RANTES in the airway epithelium., Recently, Siva et al. demonstrated that the minimization of eosinophilic airway inflammation was associated with a reduction in severe COPD exacerbation. Taken together, these studies indicate that the inflammatory characteristics of asthma and COPD are interchangeable during exacerbation and infection.
Staging And Treatment Of Asthma
The goals of long-term management of asthma should include the following: 1) achievement and maintenance of control of symptoms; 2) prevention of asthma exacerbations; 3) maintenance of pulmonary function as close to normal levels as possible; 4) maintenance of normal activity levels, including exercise; 5) avoidance of adverse effects from asthma medications; 6) prevention of the development of irreversible airflow limitation; and 7) prevention of asthma mortality.
The recommended GINA treatment algorithm, together with the clinical features and staging of severity of asthma, are available on the GINA website . It is important to note that the forced expiratory volume in one second levels are before treatment, i.e. in the unmedicated state.
Until the advent of anti-inflammatory drugs, asthma was treated on an as-needed basis and treated as an acute disease rather than a chronic disease. With the recognition that asthma is a chronic inflammatory disease, there has been a gradual move towards treating it more aggressively and earlier in the hope that this may change the natural history of asthma and prevent some of the remodelling that sometimes occurs.
What Are Obstructive Diseases
Say you swallow a hotdog. But, it doesnt travel down your esophagus to your stomach. Instead, it goes down your airway. At some point it will get stuck. So, its the most basic form of obstruction. This hotdog may completely block your airway making you unable to breathe.
But, if it gets lodged just right, you may still be able to breathe. Air can get in past this hotdog obstruction, but it will have a hard time getting out. So, when you have an obstruction, air can get in but has a hard time getting back out.
When you exhale, the obstruction resists the flow of air. So, it causes increased resistance to the flow of air. So, it may seem you can exhale forever and never get all your air out. Air is therefore slowed when you exhale. A medical term for this is airflow limitation. It is this that makes you feel short of breath.
There are diseases that may obstruct airways. Chronic bronchitis fits into this category. Asthma also fits into it. They both cause inflammation and increased sputum that make airways narrow. So, they both obstruct airways. They are obstructive diseases.1-5
Obstructive Sleep Apnea causes your upper airway to collapse while your sleeping. So, it obstructs the flow of air. Croup causes inflammation of your upper airways. So, its certainly an obstructive disease. Rhinitis causes inflammation in your nasal passages. So, it also qualifies. 5
Cystic fibrosis, emphysema, and bronchiectasis also qualify.5
Is Asthma A Lung Disease And Is It A Risk Factors For Coronavirus
- Five million in the UK suffer from asthma
- Asthma is a risk factor for coronavirus infection
- Here’s what you can do if you are asthmatic
The confirmed cases of coronavirus infections keep increasing with each passing day. In the UK, the recorded number of infections stands at 1,950, of which 71 has already died with another 20 in serious or critical condition.
This prompted Prime Minister Boris Johnson to ask people to stay at home if they belong to the group considered as high risk. The list included people suffering from asthma. What does this mean for them? asthma coronavirusPhoto: CC Public Domain – pxhere
Asthma Symptoms
The NHS said that symptoms of asthma include having a whistling sound when breathing, feelings of breathlessness, coughing, and feeling your chest getting tighter. During an asthma attack, these symptoms may get worse.
Asthma is classified as a disease of the lung. According to the British Lung Foundation, its symptoms happen when there is inflammation of the airways, which then tightens when something irritates it. The condition can be managed by using inhalers, or in worse cases, a nebulizer machine. Many asthmatics lead normal lives.
The Cause Of Asthma
The exact cause of asthma is still unknown, though it has been observed to often run in families and is common in people with allergies. Childhood asthma is often linked to allergic reactions, particularly dust or pollen.
Asthma And COVID-19
Knowing The Differences Between Copd And Asthma Is Vital To Good Practice
This content was published in 2011. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
The Outcomes strategy for people with chronic obstructive pulmonary disease and asthma was launched in July 2011 by the Department of Health, with the overall aim to drive improvements in outcomes for patients.1 Once implemented, it is expected to help people to avoid lung disease and lead longer and healthier lives. The strategy recognises the role of community pharmacy in supporting the management of people with respiratory disease through medicines use reviews and new pharmacy services.
In addition, the introduction of national target groups for MURs in England, under amendments to the NHS Community Pharmacy Contractual Framework, aims to ensure the service is provided to those who will benefit most. One of the target groups is patients with asthma or COPD.2 Both diseases have a major impact in the UK in terms of mortality and morbidity3 and the aim of MURs with these patients is to support them to take their medicines as intended, increase their engagement with their condition and medicines, and promote healthy lifestyles, in particular stopping smoking.
How Can You Tell If You Have Asthma
It can be hard to tell if someone has asthma, especially in children under age 5. Having a doctor check how well your lungs work and check for allergies can help you find out if you have asthma.
During a checkup, a doctor will ask if you cough a lot, especially at night. He or she will also ask whether your breathing problems are worse after physical activity or at certain times of year. The doctor will then ask about chest tightness, wheezing, and colds lasting more than 10 days. He or she will ask whether anyone in your family has or has had asthma, allergies, or other breathing problems. Finally, the doctor will ask questions about your home and whether you have missed school or work or have trouble doing certain things.
The doctor may also do a breathing test, called spirometry, to find out how well your lungs are working by testing how much air you can breathe out after taking a very deep breath before and after you use asthma medicine.
What Is Autoimmune Disease
Autoimmune disease is a disease where the bodys immune system attacks its own healthy cells and tissues. B cell receptors and T cell receptors of our body recognize bodys healthy tissue as antigen. So our immune system considers own body cell as foreign body and starts to act against it. Ultimately it causes a chronic inflammatory process and disrupts the normal function of the tissue.
Autoimmune disease affects 7 to 10 percent of persons in Europe and North America. The autoimmune disease causes disability and mortality.
What Causes An Asthma Attack
An asthma attack can happen when you are exposed to asthma triggers. Your asthma triggers can be very different from someone elses asthma triggers. Know your triggers and learn how to avoid them. Watch out for an attack when you cant avoid your triggers. Some of the most common triggers are tobacco smoke, dust mites, outdoor air pollution, cockroach allergen, pets, mold, smoke from burning wood or grass, and infections like flu.
How Are Asthma And Bronchiectasis Linked
People with have permanently widened airways. Long-term inflammation of the airways causes bronchiectasis. Some people are born with it, others develop it because of recurring infections.8
About 2% to 3% of people with asthma also have bronchiectasis.9,10 People with both conditions are more likely to have severe asthma and more frequent asthma attacks than people with asthma alone. 9,10 Consequently, they use more and have more visits to the emergency room.
Ask The Allergist: Does Chronic Asthma Lead To Copd
Q: Ive had severe asthma all my life. Am I at risk for developing chronic obstructive pulmonary disease, or COPD?
Bradley Chipps, MD: Not every person with asthma develops ; they are two different conditions. However, we are seeing a significant number of patients who have features of both asthma and COPD and distinguishing between the two is not always easy.
Asthma is an inflammatory lung disease often associated with allergies, and symptoms vary over time and in intensity.
COPD is a progressive disease that usually develops after the age of 40. It is characterized by persistent airflow limitation and inflammation, commonly associated with exposure to noxious particles or gases primarily cigarette smoke, either from personal use or secondhand exposure, or environmental pollutants, including biomass fuels from poorly vented gas stoves.
While asthma does not automatically lead to COPD, a person whose lungs have been damaged by frequent flares of poorly controlled asthma is at increased risk of developing COPD or if they are living or working in environments where they are exposed to airborne pollutants.
Some develop Asthma/COPD Overlap , which is now being recognized more widely in the medical community.
Q: Can you stop the progression of COPD if you catch it early enough?
Q: Whats the treatment for ACO?
I also recommend pneumonia and annual flu vaccinations, smoking cessation assistance and pulmonary rehabilitation, or exercise programs.
How Do You Monitor Asthma Symptoms
Monitoring your asthma symptoms is an essential piece of managing the disease. Your healthcare provider may have you use a peak flow meter. This device measures how fast you can blow air out of your lungs. It can help your provider make adjustments to your medication. It also tells you if your symptoms are getting worse.
Understanding The Difference Between Copd And Asthma
When you develop a lung disease or infection such as asthma or chronic obstructive pulmonary disease , you are often required to make significant lifestyle modifications to make breathing easier. After diagnosis, its normal to have questions. For many people, the big question is: How can I breathe easier?
The first step is getting the diagnosis straight. A sufferers prognosis and treatment options are very dependent on the actual condition. When it comes to chronic lung conditions, it can be difficult to tell symptoms apart, and on occasion, it can result in an incorrect diagnosis. For example, asthma and COPD differences are subtle, and theres even a third possibility: asthma-COPD overlap syndrome. Knowing the difference can be difficult but essential to a good treatment plan.
Here are a few major differences between COPD and asthma:
Inflammatory Mediators Involved In Asthma
Chemokines are important in the recruitment of inflammatory cells into the airways and are mainly expressed in airway epithelial cells . Eotaxin is selective for eosinophils, whereas thymus and activationregulated chemokines and macrophage-derived chemokines recruit Th2 cells . Cysteinyl leukotrienes are potent bronchoconstrictors and proinflammatory mediators mainly derived from mast cells and eosinophils . Cytokines orchestrate the inflammatory response in asthma. Key cytokines include IL-1 and TNF, and GM-CSF. Th2-derived cytokines include IL-5, which is required for eosinophil differentiation and survival; IL-4, which is important for Th2 cell differentiation; and IL-13, needed for IgE formation . Histamine is released from mast cells and contributes to bronchoconstriction and inflammation . Nitric oxide , a potent vasodilator, is produced from syntheses in airway epithelial cells . Exhaled NO is increasingly being used to monitor the effectiveness of asthma treatment . Prostaglandin D2 is a bronchoconstrictor derived predominantly from mast cells and is involved in Th2 cell recruitment to the airways .
Airway structural cells involved in the pathogenesis of asthma are: airway epithelial cells, airway smooth muscle cells, endothelial cells, fibroblasts and myofibroblasts and airway nerves .
Symptoms And Signs: 6 Similarities Between Copd Vs Asthma
COPD is caused by long-term exposure to lung irritants that damage lung cells. The main cause of COPD in the United States is smoke followed by other tobacco smoke . Other possible causes of COPD include chemical or toxic fumes, and factors, like alpha-1 antitrypsin deficiency, but these causes are far less common than cigarette smoking.
Although smoke may trigger asthma in some patients, asthma triggers are different from person to person, and most commonly include airborne substances such as , dust, mites, spores, pet dander, and/or many other substances. Inflammatory immune reactions to asthma triggers in the airways is the main cause of asthma.
What Should I Know About Lam
- The most common symptoms are coughing, wheezing, chest tightness and shortness of breath. Other symptoms include blood in urine, enlarged lymph nodes and swelling on the body, usually in the abdomen or feet.
- LAM worsens over time, but its progression is usually slow. There is no cure, however medications are available to help improve lung function and make breathing easier.
- If the level of oxygen in the blood is low, doctors may suggest oxygen therapy given through nasal prongs or a mask. For those with advanced disease, a lung transplant may be considered but again, this is not a cure.
Signs Symptoms And Complications
How often signs and symptoms of asthma occur may depend on how severe, or intense, the asthma is and whether you are exposed to allergens. Some people have symptoms every day, while others have symptoms only a few days of the year. For some people, asthma may cause discomfort but does not interfere with daily activities. If you have more severe asthma, however, your asthma may limit what you are able to do.
When asthma is well controlled, a person shows few symptoms. When symptoms worsen, a person can have what is called an asthma attack, or an exacerbation. Over time, uncontrolled asthma can damage the airways in the lungs.
Medical History And Physical Exam
Your doctor will ask about your risk factors for asthma and your . They may ask also about any known allergies. This includes how often symptoms occur, what seems to trigger your symptoms, when or where symptoms occur, and if your symptoms wake you up at night.
During the physical exam, your doctor may:
- Listen to your breathing and look for of asthma
- Look for allergic skin conditions, such as eczema
Why Autoimmune Disease Occurs
Research suggests that genetic factors play an important role in the development of autoimmune diseases. Based on research, it is thought that autoimmune diseases occur due to genetic risk factor. So genetic factor for autoimmune disease is shared for a range of diseases such as celiac disease, SLE, thyroiditis, Ankylosing spondylitis, type 1 diabetes and many more all these are autoimmune disease by type.
For all these diseases, one thing is common: significant genetic regions are associated with autoimmune disease risk. Many of these genes encode proteins that are established therapeutic targets and have various biological effects.
A genome-wide association study conducted in 2010 identified a region on chromosome 17 that is strongly associated with susceptibility to asthma. Also, the region in chromosome 1 is associated with asthma in African ancestral children. Chromosome 1 contains a gene, DENND1B, that is expressed by natural killer cells which is a critical component of the immune system.
So various study results indicates that genetic role is an important key for development of various autoimmune diseases including asthma.
Research For Your Health
The NHLBI is part of the U.S. Department of Health and Human Services National Institutes of Health the Nations biomedical agency that makes important scientific discovery to improve health and save lives. We are committed to advancing science and translating discoveries into clinical practice to promote the prevention and treatment of heart, lung, blood, and sleep disorders, including asthma. Learn about the current and future NHLBI efforts to improve health through research and scientific discovery.
Speak To Our Team Today
Find out if you qualify for our lung treatments.
Every day the Lung Health Institute is changing peoples lives. Our duty and obligation is to help our patients. We measure our success by our patients satisfaction and their satisfaction with our services and the care they receive from our dedicated staff.
Patient Satisfaction Focused
With over 9,000 procedures performed, each patient is assigned a dedicated Patient Care Specialist for a personalized experience.
CDC Safety and Quality Standards in Place
We have adapted and delivered comprehensive infection prevention, including COVID-19 precautions, safety innovations and processes to safeguard you during your visit.
Pulmonary Rehabilitation
Our patients are provided resources and exercises focused on improving their lifestyle with exercises, nutritional guidance, and counseling to assist in their long-term lung health. After treatment, patients are given access to an online portal with pulmonary therapy support and more.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to suggest diagnosis, treatment, cure or prevention of any disease. Lung Health Institute operates in compliance with CFR Title 21 Part 1271.15 Regulation.
