Search Methods For Identification Of Studies
Electronic searches
We identified studies from the Cochrane Airways Trials Register, which is maintained by the Information Specialist for the Group. The Cochrane Airways Trials Register contains studies identified from several sources.
Studies contained in the Trials Register are identified through search strategies based on the scope of Cochrane Airways. Details of these strategies, as well as a list of handsearched conference proceedings, are provided in Appendix 1. See Appendix 2 for search terms used to identify studies for this review.
We searched the following trials registries.
We searched the Cochrane Airways Trials Register and additional sources from inception to October 2017, with no restriction on language of publication.
Searching other resources
Management Of Patients Admitted To The Hospital: Wards And Icu Care
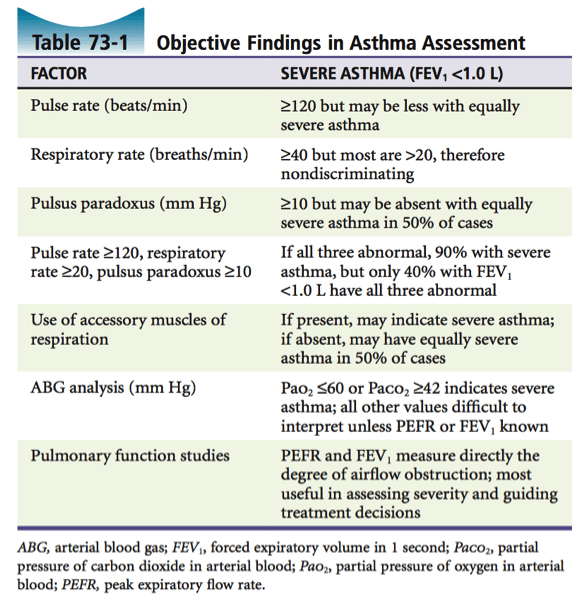
Careful consideration must be given to the level of care required when a patient with an exacerbation of asthma is admitted to the hospital. In general, guidelines suggest that patients should be admitted for observation and further treatment if the pretreatment FEV1 or PEF is < 25% of predicted or of personal best or if the post-treatment values are < 40% after emergency department treatment. Typically, patients who demonstrate a poor response to therapy , persistent or unresponsive hypercapnia, altered mental status, hypotension, or have significant comorbid conditions should be admitted to the ICU.
Although many patients maintain good oxygen saturations despite severe airway obstruction, some patients develop small airway mucus plugging even after the PEF/FEV1 normalize. Guidelines suggest that oxygen should be administered via nasal cannula or oronasal mask to maintain an arterial oxygen saturation of 9395% in adults and 9498% in children. In severe exacerbations, low-flow oxygen therapy by titrating the saturation to 9395% was associated with better physiological outcomes than with high-flow 100% oxygen therapy.
Introduction And Evolution Of Corticosteroids In The Management Of Asthma: Historical Background
Shortly after the discovery of the structure of adrenal steroid hormones, Hench et al. examined using cortisone to treat arthritis in 1949. The effect was remarkable and that work won the Nobel Prize the next year. It also started a series of trials of corticosteroids in various inflammatory conditions. The first use of corticosteroid to treat acute asthma exacerbation was in 1956. Development of corticosteroids that have less mineralocorticoid activity, like prednisone, and later those that have no mineralocorticoid activity, like dexamethasone, made corticosteroids more attractive therapies to use in asthma. In 1972, Clark showed for the 1st time that inhaled beclomethasone was effective in the management of asthma with less adverse effects than systemic steroids. Numerous reports came afterwards describing the efficacy of oral prednisone and prednisolone , IV methylprednisolone and ICS such as triamcinolone, budesonide, and fluticasone in the management of asthma. These effects are mediated through various genomic and nongenomic mechanisms. Table 2 shows some common systemic corticosteroids and their relative potency.
Don’t Miss: How To Know You Have Asthma
Definition Epidemiology And Background
Asthma is a common, chronic inflammatory disorder of the airways characterized by paroxysmal or persistent symptoms and is associated with airflow limitation and airway hyper-responsiveness . Canadian experts have proposed that asthma can be diagnosed in children as early as 1 year of age, if presenting with frequent asthma-like symptoms or recurrent exacerbations reversible with salbutamol with no other alternative diagnosis . Asthma is the most common chronic disease in young people. The general prevalence of asthma in Canada has been estimated at 10%, but is higher in children and youth, including their Indigenous peers -. Asthma exacerbations are a frequent cause of emergency department visits and hospitalizations in children , and asthma is the leading cause of absenteeism from school . Preschool age children with asthma represent more than 50% of consultations in the ED . In one Alberta study, nearly 10% of paediatric ED visits resulted in admission, with one death for every 25,000 ED visits .
Many health care centres, along with national and international associations, have developed practice guidelines for the assessment and management of acute asthma exacerbations -. This statement specifically addresses the management of acute asthma exacerbations in paediatric patients with a known diagnosis of asthma, including preschoolers whose pattern of symptoms suggests likelihood for asthma or suspected asthma .
Asthma Lifestyle Home Remedies
In addition to following your treatment plan, you can try:
- Breathing exercises. These can lower the amount of medication you need to control your symptoms.
- Herbal and natural remedies. Things that may help improve asthma symptoms include:
- Black seed oil . Some studies have shown that it can help open airways.
- Caffeine. Itâs a mild bronchodilator, meaning it can open your airways, but it doesnât work as fast as medications. Avoid caffeine for several hours before any medical appointment that might include a lung function test.
- Choline. This helps your body work the way it should. You can get it in meat, liver, eggs, poultry, fish, shellfish, peanuts, and cauliflower, or from a supplement.
- Pycnogenol. You can get this pine bark extract as a supplement.
Don’t Miss: How To Tell If Your Newborn Has Asthma
Home Management Of Asthma Exacerbations
An asthma exacerbation that causes minimal problems for the mother may have severe sequelae for the fetus. Patients should be instructed on rescue management and should be educated to recognize signs and symptoms of early asthma exacerbations such as coughing, chest tightness, dyspnea, or wheezing or by a 20% decrease in their PEFR. This is important so that prompt home rescue treatment may be instituted to avoid maternal and fetal hypoxia. In general, patients should use inhaled albuterol, 2 to 4 puffs every 20 minutes for up to 1 hour . The response is considered good if symptoms are resolved or if they become subjectively mild, normal activities can be resumed, and the PEFR is more than 80% of the personal best. For asthma exacerbations that can be managed at home, a course of oral prednisone is recommended, 40 to 60mg per day in a single dose or in two divided doses for 3 to 10 days.64 The patient should seek further medical attention if the response is incomplete or if fetal activity is decreased.
Leonard B. Bacharier, Robert C. Strunk, in, 2010
How Do You Take Asthma Medications
Asthma inhalers
Asthma inhalers are the most common and effective way to deliver asthma medicine to your lungs. Theyâre available in several types that work in different ways. Some deliver one medication. Others contain two medications. Your doctor might give you:
- A metered-dose inhaler, which uses a small aerosol canister to push out a short burst of medication through a plastic mouthpiece
- A dry powder inhaler, which releases the medicine only when you take a deep breath
Asthma nebulizer
If youâre having trouble using small inhalers, your doctor may recommend a nebulizer. This machine changes asthma medications from a liquid to a mist so itâs easier to get the medicine into your lungs. It also has a mouthpiece or mask that makes it a good option for infants, small children, older adults, or anyone who has trouble using inhalers with spacers. It takes a few more minutes to use than an inhaler.
Recommended Reading: Is Milk Good For Asthma Patients
Review Criteria And Data Extraction
All original articles were considered, excluding case reports, audits, guidelines, editorials, management/implementation strategies, conference abstracts and study protocols. We excluded animal studies. No limits were set on study design, sample size, location or follow-up. Eligible patient populations included both children and adults using asthma controller therapy: ICS, long-acting 2-agonists or fixed combination therapies of LABA and ICS. Due to incomparability, we excluded studies that looked at leukotriene receptor antagonists or xanthines only.
The first author assessed the eligibility of studies from their titles and abstracts, excluding those that were not relevant. The full texts of eligible papers were assessed independently for eligibility by two authors and data were extracted into a customised data extraction Excel form. Third party adjudication was foreseen in case of disagreement.
In Addition To Ics It Is Recommended To:
| Table 3. Inhaled daily dose of corticosteroids for asthma therapy in children is available as a supplementary file. |
You May Like: Why Asthma Makes It Hard To Breathe
Inhaled Corticosteroids And Long
In patients with poorly controlled asthma and a history of prior asthma exacerbations, the combination of budesonide and formoterol significantly reduces asthma exacerbations compared with ICS alone.50 ICS/LABA have consistently been shown to prevent exacerbations.69, 70, 71 The benefit of ICS/LABA to prevent exacerbations versus ICS alone is primarily seen in patients requiring higher doses of ICS, thus suggesting that combination therapy to prevent exacerbations should be reserved for patients with more severe disease.
Asthma control can vary even in the face of ongoing ICS/LABA treatment. Consequently, the use of ICS/LABA combinations both for maintenance and symptom relief has been investigated and shown to reduce exacerbations.72, 73, 74 These benefits are also seen in children with a prior history of severe asthma exacerbations and poorly controlled moderate-to-severe persistent asthma despite the use of moderate doses of ICS.75 The use of ICS/LABA as maintenance and reliever treatment should be restricted to formoterol because of its quick onset of action,76 safety profile,77 and dose-response effect.78
How Is Acute Asthma Exacerbation Diagnosed
How’s an acute exacerbation of asthma diagnosed?
Recommended Reading: Allergy Induced Asthma Icd 10
Acute Exacerbation Of Asthma
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Heres our process.
What happens during an acute exacerbation of asthma?
Asthma is a chronic lung disease. It causes inflammation and narrowing of your airways. This can affect your airflow.
The symptoms of asthma come and go. When symptoms flare up and get progressively worse, it can be called:
- an exacerbation
Your airways become swollen during an acute exacerbation. Your muscles contract and your bronchial tubes narrow. Breathing normally becomes more and more difficult.
Even if youve had exacerbations before and know what to do, its still a good idea to contact your doctor. An acute exacerbation of asthma is serious and can even become life-threatening. Thats why its important to recognize the symptoms early and to take appropriate action.
Its important to develop an asthma plan for how to treat your symptoms. Work with your doctor to come up with a method for what to do when your symptoms flare up.
Hows An Acute Exacerbation Of Asthma Diagnosed
If youve had an acute exacerbation before, youll probably recognize the symptoms. Your doctor will be able to make a quick diagnosis.
If its your first acute exacerbation, your doctor will need to know your medical history, particularly your history of asthma. To make a proper diagnosis, your doctor will likely perform a physical exam and a test of your lung function.
There are several tests that may be used to see how well your lungs are working:
Also Check: When To Go To Er For Asthma
Acute Asthma Prognosis And Treatment
Most recent update: July 2021Originally Posted: September 2004
Division of Allergy and Immunology,University of South Florida Morsani College of MedicineJames A. Haley Veterans’ HospitalTampa, FL 33612
Professor of Medicine, Pediatrics and Public HealthDirector, Division of Allergy and ImmunologyJoy McCann Culverhouse Chair in Allergy and ImmunologyUniversity of South Florida Morsani College of MedicineJames A. Haley Veterans’ HospitalEmail: rlockey@health.usf.edu
Michael A. Kaliner, MD FAAAAIMedical Director, Institute for Asthma and AllergyChevy Chase and Wheaton, MarylandProfessor of Medicine, George Washington University School of MedicineWashington, DC
Professor of Medicine, Pediatrics and Public HealthDirector of the Division of Allergy and ImmunologyJoy McCann Culverhouse Chair of Allergy and ImmunologyUniversity of South Florida College of Medicine and the James A. Haley Veterans’ HospitalTampa, FL
Abstract
Key words: Asthma flare Acute asthma Asthma attack Wheezing Acute asthma diagnosis Acute asthma management
Abbreviations
EPR-3 – The Expert Panel Report 3EPR-4 The Expert Panel Report 4FeNO Fractional Exhaled Nitric OxideOCS – Oral corticosteroidsCOPD – Chronic obstructive pulmonary diseasePEF – Peak expiratory flowSABA – Short acting beta agonistAE Adverse eventsFVC- Forced vital capacity
Introduction
1. Recognition of patients who are at a greater risk for near-fatal or fatal asthma.
Physical Examination
Differential Diagnosis of Acute Asthma
Complete Blood Cell Count
Cell counts and differentials are commonly requested in the emergency department in the majority of cases of asthma exacerbation. Leukocytosis is common but neutrophilia should be interpreted with caution because beta-agonists and corticosteroids may result in the demargination of white cells and an increase in the peripheral white cell count with a predominant left shift . Recommendations:CBC should not be performed routinely in cases of asthma exacerbation and leukocytosis could be a result of dermargination.
Viral study: It well known that viruses are the main trigger of asthma exacerbation .
Recommendations: Screening for viral illness should be limited to moderate or severe exacerbations or admitted cases, and it may aid in the discontinuation of unnecessary antibiotics .
Also Check: How To Reduce Asthma Problem
Inhaled Corticosteroids For Acute Asthma
Multiple trials of different types of inhaled corticosteroids for asthma exacerbations have determined minimal improvements in the respiratory scores. However, no convincing evidence is available regarding their use as an add-on therapy for severe asthma exacerbations , , , , , , ].
Recommendations: High-dose inhaled steroids are not recommended for acute asthma attacks.
Overview Of The Included Studies
The search strategy identified 2319 articles. Upon title and abstract review, 2268 of these were excluded, mainly for the following reasons: lack of information on medication adherence, no severe asthma exacerbation or no evaluation of the relationship between adherence and exacerbation articles on intervention, management or implementation strategies audit/guidelines focus on other diseases animal studies cell biology/immunology not original articles . A total of 23 articles were finally included in the review .
Overview of adult studies publishing odds ratios or relative rate , sorted by quality score, number of participants and year published. Comb: combined ED: emergency department visit for asthma hosp: hospitalisation for asthma MPR: medication possession rate perc: percentile OCS: oral corticosteroids CMA: continuous measure of availability Adh: adherence.
Objective adherence measurements
To assess overall treatment adherence, 17 studies used refill data of these, 11 used MPR measurements and six used number of prescription refills . The remaining studies used either electronic monitoring devices or weighted canisters .
The overall treatment adherence was low in paediatric and adult studies. In children, adherence measured as average MPR was only 2033.9% for ICS . The number of prescription fillings over the course of 1 year ranged from 4.7 to 5.5 times for fluticasone . In adults, MPR for ICS ranged between 15% and 54% .
Don’t Miss: Is Copd Related To Asthma
Data Collection And Analysis
At least two review authors screened the search results for eligible studies. We extracted outcome data, assessed risk of bias in duplicate, and resolved discrepancies by involving another review author. We analysed dichotomous data as odds ratios or risk differences , and continuous data as mean differences , all with a fixedeffect model. We described skewed data narratively. We graded the results and presented evidence in ‘Summary of findings’ tables for each comparison. Primary outcomes were intensive care unit/high dependence unit admission, duration of symptoms/exacerbations, and all adverse events. Seconday outcomes were mortality, length of hospital admission, relapse after index presentation, and peak expiratory flow rate .
Canadian Paediatric Society Acute Care Committee
Members: Carolyn Beck MD,Kevin Chan MD , Laurel Chauvin-Kimoff MD , Kimberly Dow MD , Karen Gripp MD, Kristina Krmptoic MD, Marie-Pier Lirette MD , Kyle C McKenzie MD , Evelyne D. Trottier MDLiaisons: Laurel Chauvin-Kimoff MD, CPS Paediatric Emergency Medicine Section Sidd Thakore MD, CPS Hospital Paediatrics Section
Don’t Miss: Can Asthma Make You Feel Light Headed
Allergy And Defective Anti
Allergic sensitization is a risk factor for wheezing with RV infection, particularly in children. Whether allergic inflammation often found with sensitization increases the susceptibility for viral infections or enhances their ability to provoke further inflammation is not entirely clear.16 Type I interferons are important innate antiviral responses to respiratory viruses.14, 17 There is evidence that virus-induced interferon generation from peripheral blood mononuclear cells,18, 19, 20 plasmacytoid dendritic cells,21 and bronchial epithelial cells22, 23 is reduced in some patients with allergic asthma . It has been show that IgE occupancy of their membrane receptors inhibits antiviral generation of IFN- from plasmacytoid dendritic cells and may increase susceptibility to RV-induced wheezing and asthma exacerbations . Deficient immune responses to viral infections may be present in type 2 inflammatory conditions with interferon production being inversely correlated with increasing airway eosinophilia, IL-4 levels, and total serum IgE.23 Finally, the use of inhaled IFN- at the time of an upper respiratory infection reduces the airway viral load and improves clinical symptoms in patients with asthma.24
Impaired plasmacytoid dendritic cell IFN- response in patients with allergic asthma. pDCs from patients with physician-diagnosed asthma and allergic sensitization secreted less IFN- on exposure to viruses compared with patients without asthma.
