Accelerated Decline In Lung Function
Since COPD represents incomplete reversibility of airflow obstruction, then any risk factor that leads to accelerated loss of lung function will contribute to the development of COPD. Several risk factors for accelerated decline in include age, smoking, BHR, asthma and exacerbations or lower respiratory infections. Increasing age is associated with decline in lung function, both in asthma and in those without asthma.
Smoking
Loss of lung function is accelerated by smoking by up to 50 ml per year, and there is an established doseâresponse relationship. The loss of lung function with smoking may even be greater in those with asthma, such that smokers with asthma can develop COPD. Importantly, quitting smoking slows the decline in lung function. In the Lung Health Study, the annual decline in FEV1 in people who quit smoking at the beginning of the 11 year study was 30 ml/year for men and 22 ml/year for women. Continued smoking led to a decline in FEV1 of 66 ml/year in men and 52 ml/year in women.
Bronchial hyper-responsiveness
Asthma
The deficits in lung function in asthma seem to arise early in the course of the disease, and may be an effect of incomplete lung growth. In one study, abnormal lung function at age 26 in patients with asthma was related to male sex, BHR at age 9 years, early onset of asthma and reduced lung function by age 9 years.
Exacerbations
How To Distinguish Between Copd And Asthma
Daniel More, MD, is a board-certified allergist and clinical immunologist. He is an assistant clinical professor at the University of California, San Francisco School of Medicine and currently practices at Central Coast Allergy and Asthma in Salinas, California.
Chronic obstructive pulmonary disease and asthma share a variety of common symptoms, which can make it difficult to distinguish between the two, at least initially. Because COPD has a certain stigma in our society that many patients do not like, some patients with COPD are more apt to say they have asthma. As with any condition, it’s important to determine the correct diagnosis to ensure that you’re getting proper treatment.
Molecular Targets In Asthma And Copd
Many external inflammatory signals such as viral and bacterial infections, allergens, cytokines, and growth factors can activate intracellular kinases, following binding to transmembrane receptors on responsive cells. Intracellular kinase pathways play critical roles in a majority of pathobiological events, including transcription, translation, cell migration, apoptosis, and cellular production and secretion of mediators., Studies have focused on the elucidation of these signaling pathways in order to find novel therapeutic targets common to both asthma and COPD. The kinases investigated include mitogen activated protein kinases such as p38, ERK, and JNK inhibitor of B kinase 2/NF-B phosphoinositol-3 kinase and signal-specific Janus kinases and signal transducers and activators of transcription.
You May Like: Can A Humidifier Help With Asthma
Study Population And Validation Studies
The study populations consisted of people who were included in earlier validation studies, and are summarised in and . Questionnaires were sent out to the GPs of possible patients with asthma and patients with COPD with the intent to validate the recording of asthma and COPD in the Clinical Practice Research Datalink . The full selection criteria of both validation studies can be found in their respective articles., Data collection for the asthma validation study was from 1 December 2013 to 30 November 2015. Data collection for the COPD validation study was between 1 January 2004 and 31 December 2012. In the asthma validation study, full data were only available for the patients for whom the GP stated a current asthma diagnosis and only current asthma diagnoses were considered. In the COPD validation study, the population was preselected as current or ex-smokers. The two patient populations included in this study have been thoroughly validated in their respective validation studies using these detailed GP questionnaires and requested supporting information, including outpatient referral letters, other emergency department discharge letters, airflow measurements, and radiography records. In the validation studies, the positive predictive value was 86.5% for COPD and 86.4% for asthma when only using a single diagnostic code for the respective disease.
Selection process of patients with validated COPD. COPD = chronic obstructive pulmonary disease.
How this fits in
Why Is It Important
There are several reasons why the overlap syndrome is important. First, patients with overlapping asthma and COPD are excluded from clinical trials of treatment. This means that for an increasing proportion of older patients with obstructive lung disease, the data on efficacy of treatment may not be relevant. The clearest example of this comes from the studies on the efficacy of inhaled corticosteroids in asthma. These studies typically exclude smokers with asthma because of the difficulty in separating asthma from COPD in smokers with obstructive lung disease. However, up to 30% of people with asthma are smokers, and this means a substantial proportion of the population are excluded from randomised controlled trials. Extrapolation of the efficacy results for corticosteroids in non-smokers to smokers with asthma is flawed. Smokers with asthma have a relative corticosteroid resistance such that corticosteroids are much less efficacious in smokers with asthma than in non-smokers with asthma. This emphasises the need to study drug efficacy in relevant clinical populations, and the necessity to include overlap syndrome in drug evaluation programmes.
Read Also: Do Allergies Cause Asthma
Asthma And Copd: What’s The Difference And Is There A Link
Asthma and chronic obstructive pulmonary disease are lung diseases. Both cause swelling in your airways that makes it hard to breathe.
With asthma, the swelling is often triggered by something youâre allergic to, like pollen or mold, or by physical activity. COPD is the name given to a group of lung diseases that include emphysema and chronic bronchitis.
Emphysema happens when the tiny sacs in your lungs are damaged. Chronic bronchitis is when the tubes that carry air to your lungs get inflamed. Smoking is the most common cause of those conditions .
Asthma gets better. Symptoms can come and go, and you may be symptom-free for a long time. With COPD, symptoms are constant and get worse over time, even with treatment.
Comparison With Existing Literature
In primary care, most consultations on respiratory diseases start with a provisional diagnosis made on clinical grounds from the patientsâ symptoms, in addition to previous specialistsâ correspondence if available.â Spirometry is needed to accurately differentiate the diagnosis of asthma and COPD, but is not always used in a primary care setting.â
Also Check: Does Qvar Cause Weight Gain
How Is Asthma Related To Chronic Obstructive Pulmonary Disease
- Date:
- University of Nottingham
- Summary:
- Two new studies exploring the causes and treatment of asthma and chronic obstructive pulmonary disease could lead to the development of drugs to battle these debilitating conditions.
Two University of Nottingham studies exploring the causes and treatment of asthma and Chronic Obstructive Pulmonary Disease could lead to the development of drugs to battle these debilitating conditions.
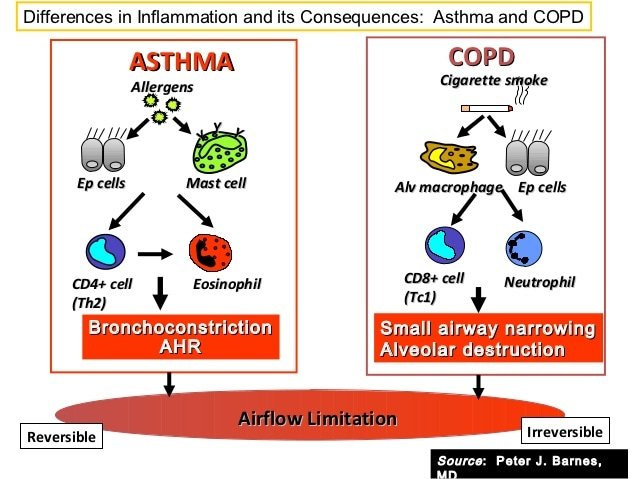
Though they are different diseases, asthma and COPD affect the human body in a similar way. In asthma, allergens irritate the lungs, in COPD, this is done by cigarette smoke. This irritation inflames the sufferer’s airways, which the muscles then close, creating a narrowing effect.
Research done at the University over the past 15 years has found that the muscle layer in the airway is more complex than has traditionally been thought. As well as going into spasm during asthma and COPD attacks the muscle layer produces a wide range of mediators and cytokines proteins that act as chemical signallers when it comes into contact with allergens or cigarette smoke. In asthma and COPD sufferers, these proteins are produced by stimulation of airway muscle cell walls in the lungs, releasing intracellular signalling proteins called ‘transcription factors’ which alter the DNA of the cell and activate messenger RNA. It is these ‘transcription factors’ which activate the inflammation by causing release of mediators and cytokines.
Story Source:
Chronic Respiratory Disease Feasibility Studies
The recommendation to expand the CCDSS to include asthma and COPD was developed in collaboration with six provinces through two rounds of feasibility studies conducted in 2009 and 2010. The studies demonstrated the feasibility of using provincial administrative health data to generate comparable estimates of asthma and COPD across provinces. These results were used to support the inclusion of the case definitions for asthma and COPD, developed during the feasibility studies, into the CCDSS.
Diagnostic fields: In the feasibility studies, variations in the case definitions were tested to determine which would yield the best results. One such study occurred in Nova Scotia where the researchers compared the use of the first diagnostic field only versus three fields when searching for the diagnostic code in the physician billing claims database. The results showed that searching beyond the first diagnostic field to identify cases made a negligible difference in the asthma and COPD prevalence estimates.
Diagnostic codes excluded: ICD-9 490 and ICD-10-CA J40 were excluded from the COPD case definition in the CCDSS. Including this code resulted in prevalence estimates double those where it was excluded and this code is not used in Ontario. It was decided by the CCDSS Chronic Respiratory Disease Working Group that this code could result in too many false positives .
Health events under surveillance: The health events under surveillance for the feasibility studies were:
Don’t Miss: Are Chihuahuas Good For Asthma
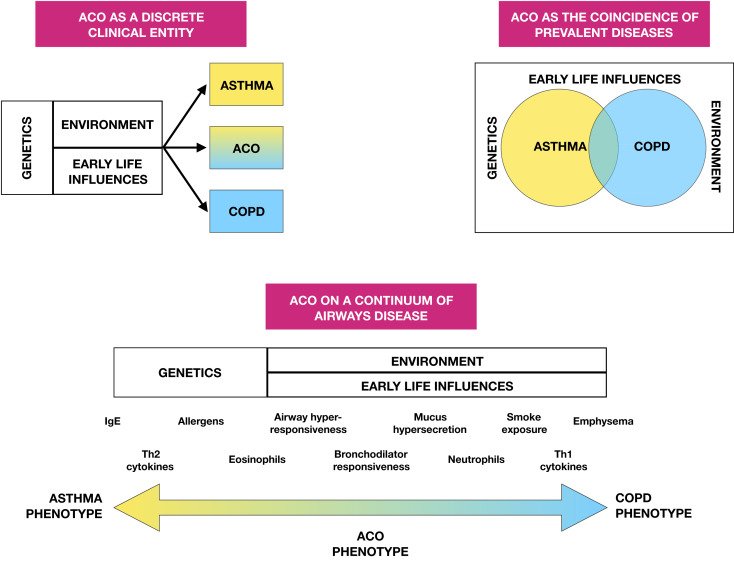
The Differences Between Copd And Asthma
Asthma and chronic obstructive pulmonary disease are both respiratory diseases involving chronic inflammation that leads to airflow obstruction. While they share similar symptoms, their causes and treatments differ. In some cases, asthma and COPD may overlap in what is termed asthma-COPD overlap syndrome, or ACOS.
However, the frequency and predominating symptoms in asthma and COPD are different. With COPD, you are more likely to experience a morning cough, increased amounts of sputum, and persistent symptoms. If you have asthma, you are more likely to experience episodic symptoms during and/or at night.
Another difference between asthma and COPD is the intermittent symptoms seen with asthma versus the chronic, progressive symptoms seen in COPD. Asthma symptoms are likely to occur after exposure to specific triggers, whereas COPD symptoms occur more regularly.
Is It Asthma Or Copd
A spirometry test, or pulmonary function test, can measure how well the lungs work. Individuals blow into the device as hard and as long as they can, providing information about how much air the lungs take in and expel. Many doctors use spirometry tests to measure airway problems associated with COPD and asthma.
Factors doctors look at when weighing a diagnosis with COPD or asthma include:
- A history of smoking: Most people with COPD are or were smokers.
- Age: Asthma often appears in childhood. If breathing difficulties occur after the age of 40, doctors are more likely to diagnose COPD.
- Symptoms: Coughing in the morning, heavy phlegm, and progressively getting worse suggest COPD. Recurring attacks, particularly if accompanied by allergies or eczema, suggest asthma.
- Family history: Asthma is more likely to run in families.
- Symptom triggers: People with COPD may have symptoms when they are active or at rest, without a known trigger. Asthma attacks may be caused by physical activity or something in the environment.
- Onset of symptoms: COPD tends to get worse over time, while asthma attacks come on suddenly.
- Responsiveness to treatment: Asthma tends to respond better to quick acting rescue inhalers than COPD does.
Diagnosis with either condition doesnt rule out developing another breathing disorder, so patients should report all symptoms to their doctor.
You May Like: Chihuahuas Cure Asthma
Definition Of Copd And Asthma
COPD
According to the American Thoracic Society / European Respiratory Society along with the Global Initiative for Obstructive Lung Disease , chronic obstructive pulmonary disease is a preventable and treatable disease with some significant extrapulmonary effects that may contribute to the severity in individual patients. Its pulmonary component is characterized by airflow limitation that is not fully reversible. The airflow limitation is usually progressive and associated with abnormal inflammatory response of the lung to noxious particles or gasses.
Asthma
Asthma is similarly characterized by airflow obstruction however, according to the National Asthma Education and Prevention Program and the Global Initiative for Asthma, asthma is additionally typified by variable and recurring symptoms, bronchial hyperresponsiveness and underlying inflammation of the airways.
What Is The Prognosis And Life Expectancy For A Person Copd Vs Asthma
The prognosis for COPD ranges from fair to poor and depends on how rapidly COPD advances over time. In general, individuals with COPD have a decrease in their lifespan according to research.
If you have asthma, the prognosis for most people ranges from fair to excellent, depending upon how well you can identify what triggers your attacks, and your response to medication.
Don’t Miss: Asthmatic Bronchitis Definition
Comorbid Diseases Or Conditions
Comorbidity is the simultaneous existence of two or more diseases or conditions in an individual. Comorbidity for the purpose of respiratory disease in the CCDSS was defined as the co-existence in an individual of one of either asthma or COPD with diabetes, hypertension, mood and/or anxiety disorders, asthma or COPD .
For asthma, the prevalence of four comorbid diseases or conditions was calculated among those with and without asthma. For diabetes and mood and/or anxiety disorders, the prevalence was calculated for those age one and older for hypertension, it was calculated for those aged 20 years and older and for COPD, for those aged 35 years and older.
For COPD, the prevalence of COPD was reported among those with and without each of the comorbid conditions. Therefore the prevalence of COPD was calculated among those with and without diabetes, mood and/or anxiety disorders, hypertension and asthma. The prevalence was calculated among those aged 35 years and older among all four comorbid diseases or conditions, corresponding to the reporting age for COPD.
The following case definitions were used for the comorbid diseases and conditions:
Diabetes
Hypertension
Mood and/or Anxiety Disorder
Individuals aged one and older with at least one physician billing claim listing a mood and/or anxiety diagnostic code in the first field, or one hospital discharge abstract listing a mood and/or anxiety diagnostic code in the most responsible diagnosis field in a one-year period.
Canadian Chronic Disease Surveillance System
The CCDSS is a collaborative network of provincial and territorial chronic disease surveillance systems, led by the Public Health Agency of Canada . The CCDSS identifies chronic disease cases from provincial and territorial administrative health databases, including physician billing claims and hospital discharge abstract records, linked to provincial and territorial health insurance registry records using a unique personal identifier. Data on all residents eligible for provincial or territorial health insurance are captured in the health insurance registries thus, the CCDSS coverage is near-universal with the exception of some small populations. Case definitions are applied to these linked databases and data are then aggregated at the provincial and territorial level before being submitted to PHAC for reporting at the provincial, territorial and national levels.
The CCDSS has expanded from its initial mandate of diabetes surveillance to include data on several additional chronic diseases and conditions including: hypertension, mental illness, mood and/or anxiety disorders, heart failure, ischemic heart disease, acute myocardial infarction, stroke, osteoporosis, arthritis and neurological conditions. Asthma and COPD were added to the CCDSS in 2012.
The data presented in this report and subsequent updates can be accessed on the Public Health Agency of Canada’s Public Health Infobase.
Also Check: Does A Chihuahua Take Away Asthma
Why Does Overlap Happen
Having already analyzed all the potentially important common risk factors for overlapping asthma and COPD, such as increasing age, smoking, BHR, inflammation, remodeling and exacerbations, the big question is why does overlap happen. Dutch hypothesis tries to answer the question, stating that asthma and BHR predispose to COPD later in life and that asthma, COPD, chronic bronchitis, and emphysema are different expressions of a single airway disease. Furthermore, the presence of these expressions is influenced by host and environmental factors . Epidemiological studies, on the other hand, proved a correlation between respiratory illnesses during childhood and impaired adult lung function . Knowing that airway growth starts in utero, fetal or childhood exposures may contribute to adult asthma or COPD .
Implications Of Overlapping Asthma And Copd
How-to videos available from the National Asthma Council AustraliaPatients with coexisting asthma and COPD have an increased illness burden1 compared to those with asthma or COPD alone. They have more frequent and severe exacerbations9 and hospitalisations. This is despite having had fewer pack-years of smoking than those with COPD alone.9 Mortality may also be increased.1,10
Asthma may also be a risk factor for developing COPD.1,4,11 In severe asthma, structural changes such as airway remodelling can contribute to fixed airway obstruction and smaller airway size. Single nucleotide polymorphisms have been identified in biologically plausible genes associated with asthmaCOPD overlap but their significance is unclear.9
Read Also: How To Get Rid Of Asthma Without Inhaler
Questions That Will Help Your Doctor Determine If You Have Copd Or Asthma
Answers to the following questions will aid in a proper diagnosis of your condition.
Did I have symptoms of allergy or asthma as a child?
While some patients are diagnosed with asthma in adulthood, most asthmatics are diagnosed in childhood or adolescence. In fact, a number of studies have shown that primary care doctors will often label older patients with asthma when in fact they have COPD. While COPD can be a llong-termcomplication of poorly controlled asthma, COPD is rarely diagnosed before the age of 40.
What makes my symptoms worse?
Asthmatics can often identify what it is that worsens their symptoms. Things such as:
COPD, on the other hand, is often made worse by respiratory tract infections and not any of the asthma triggers mentioned above.
Am I a current or past smoker?
While COPD and asthma may occur together, COPD is more common in current or former smokers and those exposed to environmental tobacco smoke. While COPD can occur in patients that have never smoked, greater than 80% of patients with COPD smoked in the past or are current smokers.
Am I ever symptom-free?
Patients with asthma experience symptoms intermittently, are relatively symptom-free between asthma exacerbations and tend to experience significant periods of time without symptoms when their asthma is under good control. COPD patients, on the other hand, experience progressive symptoms and rarely go a day without symptoms.
Does my lung function return to normal between exacerbations?
