What Can I Expect If I Have Eosinophilia
If you have high eosinophils levels, you may need treatment for the underlying condition causing your high levels. There are many causes, ranging from mild and completely safe to more serious. Talk to your healthcare provider to learn more.
A note from Cleveland Clinic
Eosinophilia happens when your body produces too many eosinophils. Eosinophils are one of several white blood cells that support your immune system. Many times, people learn they have eosinophilia when they have routine blood tests. A high eosinophil count typically isnt a cause for alarm. Your healthcare provider may order additional tests to find out why your eosinophil levels are unusually high.
Tests For Severe Asthma
Along with finding out about your medical history you will also be sent for tests.
To diagnose severe asthma there are a number of tests you can take. Depending on the results, these tests can confirm you have severe asthma and the type of severe asthma it is, or show that there are other reasons for your symptoms.
There are a lot of tests that can be used to help your doctor diagnose severe asthma, but you will probably only need some of them.
High Number Of Eosinophils
Often, people are first tested and treated for more common causes of their symptoms. For example, they might undergo testing for infection and even receive antibiotics even though no infection is found. Because people still have symptoms after treatment, doctors often take a sample of tissue for examination , which will show eosinophils within the organ that is affected.
Treatment of these conditions frequently includes oral corticosteroids.
Read Also: How Do You Know If A Kid Has Asthma
Testing For Severe Asthma
Before you can be tested for severe asthma, you will need a referral from your primary healthcare asthma provider to either an asthma specialist or allergy specialist . The specialist will review your medical history, your current asthma treatment plan and do a physical exam to assess your symptoms. If the specialist thinks you may have severe asthma, they will discuss additional testing with you to determine your specific type. This often starts with testing to identify a biomarker.
Biomarkers help determine what is causing the inflammation in your airways. Taking a blood sample, analyzing a mucus sample or taking a breathing test that measure substances in your breath droplets are all common tests doctors use. These tests are performed in a doctors office or an outpatient clinic setting. Your specialist will recommend one or more of these tests based on your medical history and current symptoms. Once the biomarkers are identified, your doctor can determine the type of severe asthma and the different treatment options that are available to treat that specific type.
When Is Quick Relief For Asthma Not Enough
DO YOU.
- Take your quick relief inhaler more than TWO TIMES A WEEK?
- Awaken at night with asthma more than TWO TIMES A MONTH?
- Do you refill you quick relief inhaler more than TWO TIMES A YEAR?
- Use prednisone TWO or more times a year for flares of asthma?
- Measure changes in peak flow with asthma symptoms of more than TWO TIMES 10 ?
If you answer YES to any of the questions, current guidelines suggest you talk with your physician about adding an inhaled anti-inflammatory to improve your asthma control.
Also Check: How To Calm Asthma Without An Inhaler
Study Design And Data Source
We conducted a retrospective data analysis of patients with asthma diagnosis, extracted from the EMRClaims+ integrated health services database of patients located in the Midwest region of the United States. The database includes administrative insurance claims from approximately 675,000 lives linked to an overlapping healthcare provider database of over 20 million electronic medical records data , including laboratory values, and provider billing files.
How Do Healthcare Providers Treat Eosinophilia
Healthcare providers treat the underlying condition or issue thats causing high eosinophil counts. For example, if you have eosinophilic esophagitis, your healthcare provider may prescribe steroids or other medications. If you have high eosinophil levels because you have allergies or chronic sinusitis, your healthcare provider may recommend allergy testing to find out what causes the allergic reaction that triggered eosinophilia. If a medication is causing eosinophilia, your healthcare provider will usually recommend stopping or avoiding it. If theres an infection, your healthcare provider will treat it. If theres a blood cancer, your healthcare provider will treat it.
Read Also: Are Asthma Inhalers Prescription Only
Two New Medications For Severe Eosinophilic Asthma
Katherine Thompson, PharmD
CHI Health St. Elizabeth Regional Medical CenterLincoln, Nebraska
Lee E. Morrow, MD, MSc, FCCPProfessor of Medicine and Pharmacy PracticeCreighton UniversityDivision of Pulmonary, Critical Care, and Sleep MedicineOmaha, Nebraska
Professor of Pharmacy Practice and MedicineCreighton UniversityOmaha, Nebraska
US Pharm. 2017 42:16-19.
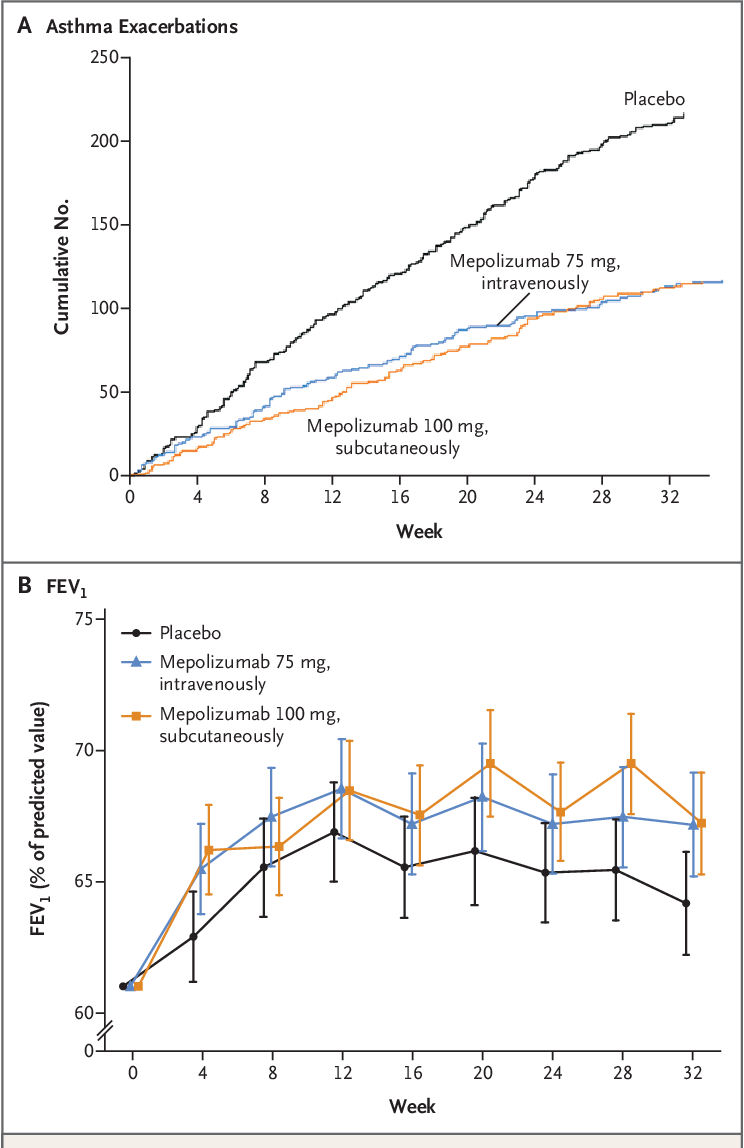
ABSTRACT: Asthma is a common, chronic respiratory disease in which the lungs airways become inflamed and narrowed. While the majority of patients with asthma can be treated effectively with the proper use of maintenance medications, patients with severe asthma are refractory to current standards of treatment, including oral corticosteroids. Eosinophilic asthma is a subset of severe asthma that is characterized by increased eosinophil counts. Because increased eosinophilia correlates with worse disease, mediators of the eosinophil pathway, such as interleukin-5 , are targets for preventing eosinophil-mediated inflammation. Recently, the new IL-5 receptor antagonists reslizumab and mepolizumab were approved by the FDA for use in severe eosinophilic asthma. Used as maintenance therapy, these agents may benefit patients with eosinophilic asthma.
Also Check: Does Ibuprofen Make Asthma Worse
Why Is The Absolute Eosinophil Count Test Done
A doctor could suggest this test to know about abnormal eosinophil levels. Besides, it is also done in combination with a complete blood count test to know the % of different kinds of white blood cells that are present in the blood. This test will say if there is an abnormally low or high white blood cell count. The count of white blood cells varies in some types of diseases.
The other instances where the test is needed include
- An intense allergic reaction
- An infection due to fungus or a parasite
- A response to some medications
Eosinophilic Asthma
- Early phases of Cushings disease
- Eczema
- Leukemia and other types of blood disorders
Recommended Reading: How To Treat Childhood Asthma Naturally
Why Should I Get Tested
If you have asthma and are using your rescue inhaler frequently, if you wake up at night due to asthma symptoms, if you take oral steroids like prednisone, and/or if your asthma attacks have required emergency care, then your asthma might be uncontrolled. A blood test, along with speaking to your primary care provider or an asthma specialist, may help determine if you have e-asthma, and if further evaluation of your asthma is necessary. Talking with your physician about the test results may help identify your type of asthma and additional treatment options to help control your asthma.
Your Eosinophilic Test Results: What To Expect Next
If youre diagnosed with eosinophilic asthma, your doctor might prescribe one of three treatments designed to target eosinophils, says Chupp. These medications, called biologics, can help lower the levels of eosinophils and resulting inflammation in the lungs, which can reduce asthma attacks. Given as injections or infusions you receive every few weeks at your doctors office, these therapies work by targeting specific molecules involved in the action of eosinophils. Mepolizumab and reslizumab are antibodies against interleukin 5 molecules, while benralizumab is an antibody against the IL-5-receptor-alpha-chain. Studies suggest that these drugs are safe and effective in most people with eosinophilic asthma, says Chupp.
If you have severe or hard-to-treat asthma, talk to your doctor about whether you should be tested for eosinophilia. If you do have eosinophilic asthma, it can affect the type of treatment youll need.
Read Also: Is Phoenix Bad For Asthma
How Do Changes In Eosinophils Affect Health And Wellbeing
Allergies such as asthma can affect your everyday life, particularly at certain times of the year. For example, if you are allergic to grass pollen, your symptoms may be more prevalent during June and July. Eosinophil numbers increase during a parasitic infection or allergy.
If an increased eosinophil count is because of a parasitic or worm infection, then the symptoms can make you feel quite unwell. Plus, an infection can cause a reduction in energy levels, making you feel weak and tired.
If you are worried about your immune system or just want to check where you fall on the range, you can test your eosinophils level with a simple at-home blood test.
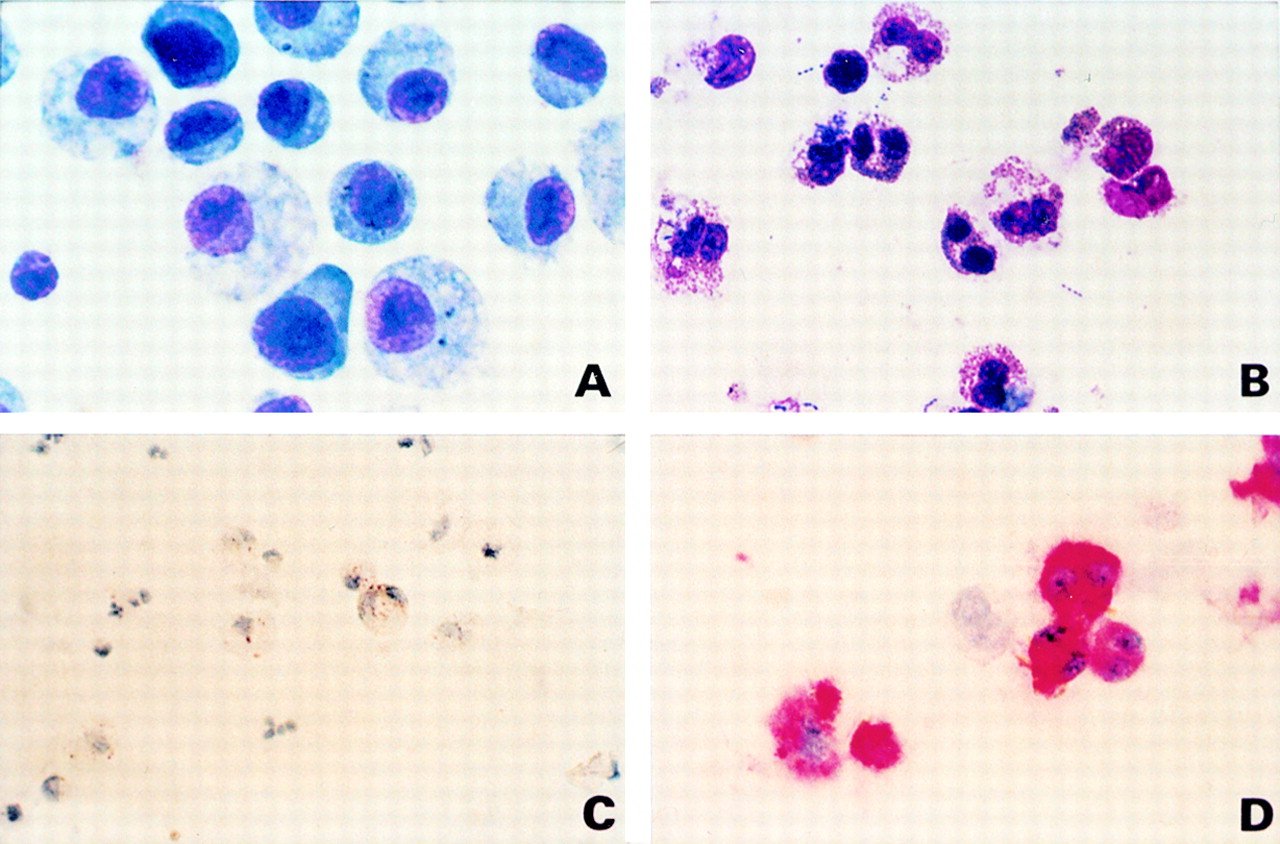
Role Of Innate Immune Activation
The common pathophysiological features of non-eosinophilic asthma involve an IL-8 mediated neutrophil influx and the subsequent neutrophil activation is a potent stimulus to increased airway hyperresponsiveness. Although the stimuli that trigger this response are diverse , the common features are consistent with activation of innate immune mechanisms rather than IgE mediated activation of acquired immunity. Recent data indicate a role for Toll-like receptors and CD14 in this process. TLRs can recognise a large variety of chemically diverse stimuli which then trigger proinflammatory responses involving NF-úB activation and chemokine production characteristic of non-eosinophilic asthma .
There is also the potential for combined activation of both innate and allergen specific inflammatory mechanisms to occur in asthma. This could result in a mixed eosinophil/neutrophil response as has been observed in some cases of acute asthma, and may explain the ability of ozone and NO2 to potentiate allergen induced asthmatic responses.
Recommended Reading: How To Get Rid Of Asthma Without Inhaler
Read Also: How Does Aspirin Trigger Asthma
Be Prepared For A Doctors Appointment Beforehand:
Sufferers with a suspected asthma or asthma will be referred to a pulmonologist or an allergist. So, we have prepared a list of tips that may prove helpful to get you prepared for the doctors appointment:
- Dont forget to keep a proper record of the symptoms you are having, even if they are seemingly unrelated.
- Remember to maintain and bring a list of medications you are taking be it vitamins, over the counter medications, or the supplements.
Prepare list of questions that you have in your mind like:
- What tests can be performed For Eosinophilic Asthma?
- How should I use my medications?
- What are the triggers for asthma flare ups?
- Can I do anything to reduce the risk of having an asthma attack?
- Do I need to change my diet?
- Can I restrict the use of inhalers?
- Is there any elimination diet?
- How often do I need follow-up care?
What Can I Do To Lower The Eosinophil Count In The Blood
If there is a mild transient eosinophilia with no symptom, no action is necessary. The count probably will return to normal in the following test.
On the other hand is there is a moderate or severe eosinophilia you should visit your doctor and ask about the medication you are taking. Several drugs may raise the eosinophil count.
If there is an underlying cause, for example a parasitic infestation it is necessary to treat and solve previously this disease.
Corticosteroids reduce the eosinophils in the blood. If your doctor considers it appropriate he may prescribe them to you.
Also Check: How To Get Rid Of Asthma Cough
Why Do I Need An Eosinophil Count
Your doctor may discover abnormal eosinophil levels when a white blood count differential is performed. A white blood count differential test is often done alongside a complete blood count and determines the percentage of each kind of white blood cell present in your blood. This test will show if you have an abnormally high or low count of white blood cells. White blood cell counts can vary in certain diseases.
Your doctor may also order this test if they suspect specific diseases or conditions, such as:
- an extreme allergic reaction
Before the test, be sure to tell your doctor about any current medications or supplements youre taking.
A healthcare provider will take a sample of blood from your arm by following these steps:
What Does High Eos Absolute Blood Test Mean
High Absolute Eosinophils . A high absolute eosinophil count indicates that there is an elevated number of eosinophils a type of white blood cell in tissue or in the blood. Because white blood cells like eosinophils fight infection and cause inflammation, a high absolute eosinophil count may indicate a viral or bacterial infection, parasites,
Recommended Reading: Is Caffeine Bad For Asthma
Treatment: How Do We Treat Patients With Sea
Patients with severe asthma who have an eosinophilic-driven phenotype may benefit from newly developed precision medicines. One group clearly eligible for treatment with biologics is those patients with severe asthma adherent to high-dose inhaled corticosteroids who nevertheless have frequent exacerbations with or without symptoms, and who have persistently elevated levels of circulating blood eosinophils.
There are number of targeted therapies, both licensed and in development, that are appropriate for consideration in this patient population. Three biologic therapies are now licensed for severe asthma: omalizumab ), mepolizumab ) and reslizumab . Four more are currently in the development process: benralizumab has recently reported successful phase 3 results tralokinumab and dupilumab are in phase 3 trials and pitrakinra has completed phase 2 trials . Guidance is needed to understand how best to use these different treatments in practice, tailoring treatment choice to the clinical picture and selecting patients likely to benefit.
If Youre Living With Asthma
taking care of yourself starts with understanding the type of asthma you have.
Knowing your asthma type is especially important if you are taking multiple treatments, but symptoms still interfere with your daily activities. If this is you, there may be a treatment option available so you can start getting back to things that matter.
What is asthma?
Asthma is a long-term condition that is caused by inflamed airways.
If youve been living with asthma for a while, you already know the common symptoms. And when symptoms get worse, its called an asthma attack .
An attack can happen after exposure to a trigger something that causes your immune system to react and increases inflammation in your lungs. Triggers are different for everyone. Common triggers include dust, mold, and outdoor air pollution.
Usually, asthma symptoms can be managed with a combination of oral and inhaled medications. But sometimes, thats not enough.
Poorly controlled, severe asthma can be different.
Poorly controlled, severe asthma is hard to manage even with high-dose inhalers and oral steroids.
Here are some signs that your asthma may be severe and poorly controlled:
- Even if youre taking multiple asthma medications, you still have symptoms.
- You sometimes have to take oral steroids for asthma attacks.
- Symptoms wake you up at night.
- You need to go for breathing treatment at your doctors office.
- Youve been to the emergency room or hospital due to asthma symptoms.
Shelby discusses her symptoms.
Also Check: What Can Asthma Lead To If Not Treated
Data Source And Study Design
Data were extracted from the Optimum Patient Care Research Database and the Clinical Practice Research Datalink GOLD database. OPCRD comprises data obtained through the Optimum Patient Care Quality Improvement services, which contains information from both anonymized electronic medical records and patient responses to disease-specific questionnaires. At data extraction, OPCRD contained data for approximately 10 million patients from more than 700 practices in the UK. CPRD GOLD is a primary care database of anonymized medical records that includes data for more than 11 million patients from 674 general practices in the UK.27 Data obtained from CPRD were limited to patients whose records could be linked to Hospital Episode Statistics, a comprehensive source for hospital admission and outpatient HCRU data. Patient-level data from OPCRD and CRPD are de-identified at the source, and patients have the option to opt-out of sharing their health information.
Baseline data represented the 12 months prior to the index date, defined as the most recent BEC measurement for which there were 12 months of subsequent outcomes data . Asthma outcomes and HCRU were evaluated for 12 months after the index date . The year of the index date for patients included in the data sets ranged from 2006 to 2018.
Will This Diagnosis Change How My Asthma Is Treated
Maybe. Some patients with eosinophilic asthma respond to the traditional methods of treating it, using inhaled corticosteroids to reduce inflammation and bronchodilators like as a quick-acting rescue medication. However, since eosinophilic asthma affects the entire respiratory tract, inhaled steroids are often not enough, and many patients require systemic oral steroids to see symptom improvement.
New treatments are also being developed to reduce the number of eosinophils in the airway. These may be a good option for you if your symptoms dont respond to steroids.
-
Anti-interleukin-5 therapy- Interleukin-5 is a protein that activates eosinophils. Biologic therapies, such as mepolizumab and reslizumab , block IL-5. They are both used in conjunction with other asthma medications.
-
Anti-immunoglobulin E therapy- Immunoglobulin E is an antibody that plays a role in . Therapies, like omalizumab , that block IgE decrease both inflammation and the number of eosinophils in the airway. However, this treatment will only be effective for cases of eosinophilic asthma that are triggered by allergens.
-
Clinical trials- Researchers are studying other treatments that target interleukins, such as anti-IL-4 and anti-IL-13. Early results look favorable for these new therapies.
Read Also: What Can Cause Asthma Like Symptoms
Recommended Reading: Allergy And Asthma Center Of Minnesota
Asthma Control During The Outcome Year
A greater percentage of patients with 1 BEC > 300 cells/µL experienced 1 severe asthma exacerbation during the outcome year compared with the never high group . Other measures of asthma control were not appreciably different among blood eosinophil pattern groups. Full asthma control was achieved by 22.3%, 24.3%, and 23.6% of patients in the persistently high, intermittently high, and never high groups, respectively.
|
Table 4 Asthma Control During the Outcome Year by Longitudinal Eosinophil Pattern |
|
Table 5 Association Between Eosinophil Pattern and the Rate of Exacerbations During the Outcome Year |
|
Figure 4 Association between longitudinal eosinophil patterns and exacerbations in the outcome year by smoking status. Abbreviation: CI, confidence interval. |
Read Also: Asthma Inhaler Ingredients
