Measures For Indoor Air Pollution
As many people spend most of their time indoors, to reduce the production of indoor pollutants and avoid inhalation are more important. To choose furniture with less chemical emission, check the ventilation system of the house regularly, ventilate the room as opening the door and windows regularly to fresh the air so as to reduce harmful gaseous pollutants from the furniture and construction material, use clean fuels instead of biomass fuels if possible, improve cooking stoves to burn fuel more efficiently and use a chimney woodstove to vent emissions to outside, and similar interventions are feasible and recommended . These measures can significantly reduced indoor air pollution and relieve symptoms consistent with chronic respiratory tract irritation .
During smoke episodes like forest fires, community members should remain indoors and use air cleaners. The air cleaner can effectively reduce PM2.5 exposure during forest fires and residential wood burning . Electrostatic air cleaners can reduce all size particles. The irritation and general symptom indices decreased . In peoples exposed to smoke from wildfire, using of high-efficiency particulate air cleaners could reduce odds of reporting adverse health effects of the lower respiratory tract .
How Is Copd Treated
Treatment of COPD requires a careful and thorough evaluation by a physician.3,13 COPD treatment can alleviate symptoms, decrease the frequency and severity of exacerbations, and increase exercise tolerance. Treatment options that your physician may consider include:
- Quit smoking. For people who smoke, the most important part of treatment is smoking cessation.
- Avoid tobacco smoke and other air pollutants at home and at work.
- Ask your doctor about pulmonary rehabilitation, which is a personalized treatment program that teaches COPD management strategies to improve quality of life. Programs may include plans that teach people how to breathe better and conserve their energy, as well as provide advice on food and exercise.
- Take medication. Symptoms such as coughing or wheezing can be treated with medication.
- Avoid lung infections. Lung infections can cause serious problems in people with COPD. Certain vaccines, such as flu and pneumococcal vaccines, are especially important for people with COPD. Learn more about vaccination recommendations. Respiratory infections should be treated with antibiotics, if appropriate.
- Use supplemental oxygen. Some people may need to use a portable oxygen tank if their blood oxygen levels are low.
To learn more about COPD, visit the Resources page.
Occupational Copd An Underestimated Category
We identified only 20 out of 474 publications that referred to occupational COPD, with most of them implicating inorganic or organic dust or fumes, such as cement dust, construction work and diesel exhaust, as the causative agents.
As an example, the mixed agent cement dust was investigated in 14 studies but only four studies documented cement dust as the causative agent in occupational COPD . The remaining 10 studies described irritant-induced OA cases or identified significant asthma symptoms/ obstructive ventilation patterns without a clear diagnosis . It can be assumed that if it had been considered on the other 10 studies then occupational COPD caused by cement dust would have been frequently observed.
General acceptance of this statement does not exist, although evidence for an association between individual exposure levels and COPD is accumulating in the latest literature.
You May Like: Upper Respiratory Infection And Asthma Exacerbation
When Should I Call My Doctor If I Have Copd And I Might Have An Infection
Avoiding irritants
The lungs of people with COPD are sensitive to certain irritating substances in the air, such as: cigarette smoke, exhaust fumes, strong perfumes, cleaning products, paint/varnish, dust, pollen, pet dander and air pollution. Extreme cold or hot weather conditions can also irritate your lungs.
You can avoid some of these irritants by:
- Asking those around you not to smoke.
- Sitting in non-smoking sections of public places.
- Requesting smoke-free hotel rooms and rental cars.
- Avoiding underground parking garages.
- Avoiding high traffic or industrialized areas.
- Not using perfumes, scented lotions or other highly scented products that may irritate your lungs.
- Using non-aerosol cleaning or painting products in well-ventilated areas and wearing a mask or handkerchief over your mouth when cleaning or working in the yard.
- Reducing exposure to dust by regularly changing filters on heaters and air conditioners and using a dehumidifier.
- Keeping pets out of the house, especially if you wheeze.
- Using an exhaust fan when cooking to remove smoke and odors.
- Staying indoors when the outside air quality is poor and pollen counts are high.
- Following weather reports and avoiding extreme weather. During cold weather, cover your face when going outdoors. During extreme humidity, try to stay in air conditioned areas.
Basis And Quality Of Data
Irritant-induced obstructive airways diseases cannot usually be diagnosed in one clinical visit and, instead, follow-up and/or detailed clinical investigations are necessary. The diagnostic gold standard for OA is SIC using a specific occupational agent in an exposure chamber. SIC is particularly indicated in the clinical setting where new causative substances with still unknown adverse respiratory sensitization potential are suspected. This gold standard is not applicable for large studies so, it was used mainly in case series or reports.The evidence levels to confirm irritant-induced work-relaated asthma or occupational COPD for the listed irritant agents, professions or worksites are frequently low with the major reasons being that high quality studies were missing and the quality of the available studies was low. Nevertheless, this knowledge is the best available and may help physicians to identify a suspected irritant agent as causative in irritant-induced work-related asthma and / or occupational COPD. As also recently stressed by Quint et al., implementing an evidence-based identification and regulatory process for OA will help to ensure primary prevention of OA. In cases of low evidence level of an agent that does not exclude a causative role, caution should be exercised and a more detailed diagnostic testing of relevant exposure should be performed.
You May Like: How To Get Rid Of Asthma Without Inhaler
Recommended Reading: What’s An Asthma Attack Feel Like
Chronic Respiratory Disease Feasibility Studies
The recommendation to expand the CCDSS to include asthma and COPD was developed in collaboration with six provinces through two rounds of feasibility studies conducted in 2009 and 2010. The studies demonstrated the feasibility of using provincial administrative health data to generate comparable estimates of asthma and COPD across provinces. These results were used to support the inclusion of the case definitions for asthma and COPD, developed during the feasibility studies, into the CCDSS.
Diagnostic fields: In the feasibility studies, variations in the case definitions were tested to determine which would yield the best results. One such study occurred in Nova Scotia where the researchers compared the use of the first diagnostic field only versus three fields when searching for the diagnostic code in the physician billing claims database. The results showed that searching beyond the first diagnostic field to identify cases made a negligible difference in the asthma and COPD prevalence estimates.
Diagnostic codes excluded: ICD-9 490 and ICD-10-CA J40 were excluded from the COPD case definition in the CCDSS. Including this code resulted in prevalence estimates double those where it was excluded and this code is not used in Ontario. It was decided by the CCDSS Chronic Respiratory Disease Working Group that this code could result in too many false positives .
Health events under surveillance: The health events under surveillance for the feasibility studies were:
What Are Warning Signs Of An Infection Especially If I Have Copd
Warning signs of infection
While most infections can be successfully treated, you must be able to recognize an infection’s immediate symptoms for proper and effective care.
- Increased shortness of breath, difficulty breathing or wheezing
- Coughing up increased amounts of mucus
- Yellow- or green-colored mucus
- Fever or chills
- Increased fatigue or weakness
- Sore throat, scratchy throat or pain when swallowing
- Unusual sinus drainage, nasal congestion, headaches or tenderness along upper cheekbones
If you have any of these symptoms, contact your physician right away, even if you do not feel sick.
Read Also: Chihuahua Takes Away Asthma
Whos Likely To Have Asthma Copd Or Aco
People who smoke or breathe in pollution or chemicals at work for many years have higher chances of having COPD. That’s why the condition often starts in middle age or later in life.
Asthma is sometimes caused by gene changes that are passed down through families. If one of your parents has the disease, you’re more likely to have it.
Symptoms of asthma often start in childhood, and the condition is one of the most widespread long-term illnesses in kids. It affects about 1 in 10 children.
Besides a family history of the condition, a few things can raise your chances of asthma:
- Smoking
- Being around chemicals or other irritants in the air
People who get ACO tend to be over 40 but younger than people with just COPD, and they have allergies .
Symptoms And Signs: 6 Similarities Between Copd Vs Asthma
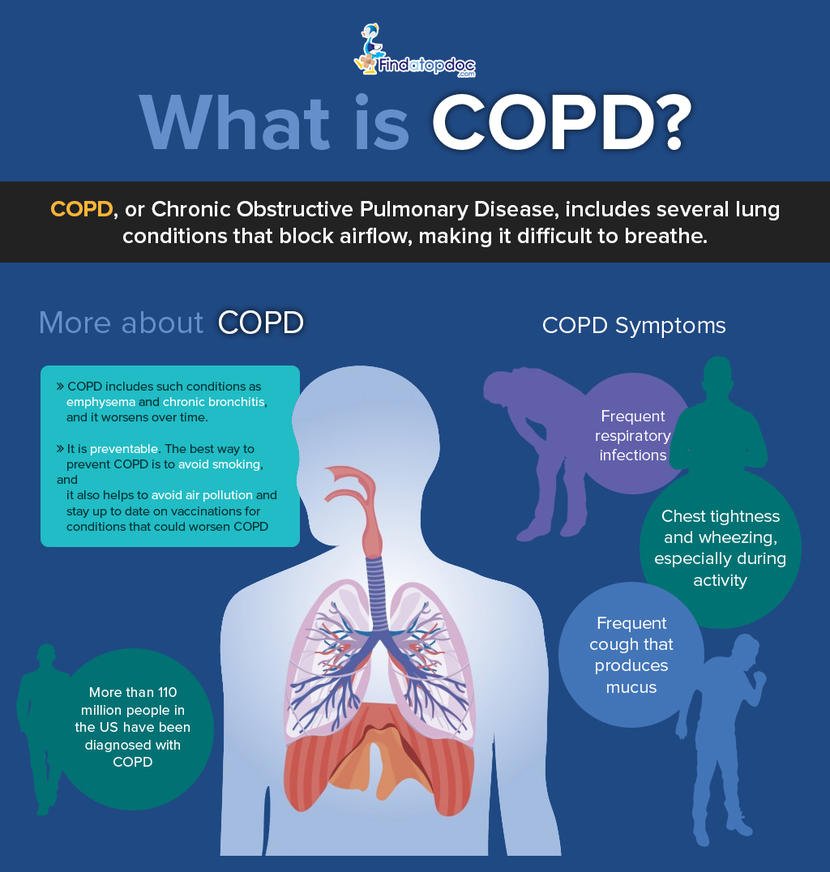
COPD is caused by long-term exposure to lung irritants that damage lung cells. The main cause of COPD in the United States is cigarette smoke followed by other tobacco smoke . Other possible causes of COPD include chemical or toxic fumes, and inherited factors, like alpha-1 antitrypsin deficiency, but these causes are far less common than cigarette smoking.
Although cigarette smoke may trigger asthma in some patients, asthma triggers are different from person to person, and most commonly include airborne substances such as pollen, dust, mites, mold spores, pet dander, and/or many other substances. Inflammatory immune reactions to asthma triggers in the airways is the main cause of asthma.
You May Like: Asthma Ct Scan
Are There Rehabilitation Programs For Copd
The goals of COPD rehabilitation programs include helping the patientreturn to the highest level of function and independence possible, whileimproving the overall quality of the persons physical, emotional, andsocial life. Attaining these goals help people with COPD live morecomfortably by improving endurance, providing relief of symptoms, andpreventing progression of the disease with minimal side effects.
In order to reach these goals, COPD rehabilitation programs may include thefollowing:
-
Medication management
-
Exercises to decrease respiratory symptoms and improve muscle strength and endurance
-
Respiratory treatments to improve breathing ability
-
Assistance with obtaining respiratory equipment and portable oxygen
-
Methods to increase independence with activities of daily living
-
Exercises for physical conditioning and improved endurance
-
Stress management, relaxation exercises, and emotional support
-
Smoking cessation programs
Dont Miss: Asthma And Humidifier Use
Treatment Of Exacerbations Of Copd And Asthma
The treatment of asthma exacerbations is reasonably standardised with inhaled 2 agonists and systemic glucocorticoids as the cornerstone of pharmacological treatment with oxygen when required. This approach is based on several studies reported in the literature and recently reviewed,,,,, and is consistently recommended by national and international guidelines.,,, By contrast, the treatment of COPD exacerbations is much less established, probably because of the limited number of properly conducted studies., In fact, the treatment of asthma and COPD exacerbations is similar and is based on the administration of oxygen, short acting bronchodilators, and systemic glucocorticoids.,,
Short acting inhaled 2 agonists are usually the preferred bronchodilators used in the treatment of both asthma and COPD exacerbations.,,, If there is no prompt response, the addition of an anticholinergic is recommended, particularly for COPD exacerbations,,, even if supportive evidence for the effectiveness of the combination is rather controversial. Despite the consolidated clinical practice, the role of aminophylline in the treatment of asthma and COPD exacerbations also remains controversial, as most of the studies have shown that aminophylline increases the toxicity but not the efficacy of 2 agonists, particularly in asthma.,,,,
Recommended Reading: Is Asthma A Small Airway Disease
Chronic Obstructive Pulmonary Disease
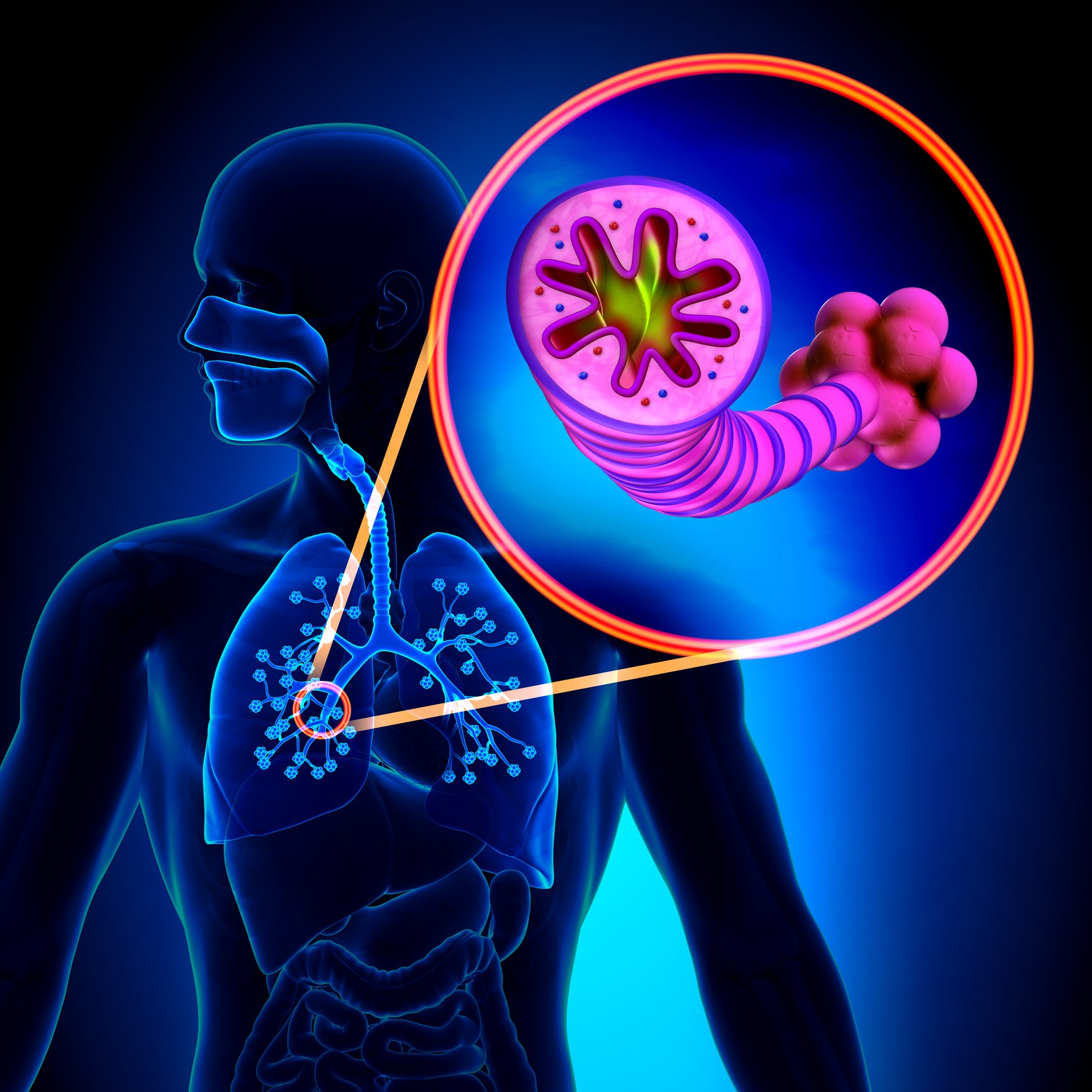
In the recent Global Initiative for Chronic Obstructive Lung Disease Guidelines , COPD is defined as follows: a disease state characterised by airflow limitation that is not fully reversible. The airflow limitation is usually progressive and associated with an abnormal response of the lungs to noxious particles or gases.
Comorbid Diseases Or Conditions
Comorbidity is the simultaneous existence of two or more diseases or conditions in an individual. Comorbidity for the purpose of respiratory disease in the CCDSS was defined as the co-existence in an individual of one of either asthma or COPD with diabetes, hypertension, mood and/or anxiety disorders, asthma or COPD .
For asthma, the prevalence of four comorbid diseases or conditions was calculated among those with and without asthma. For diabetes and mood and/or anxiety disorders, the prevalence was calculated for those age one and older for hypertension, it was calculated for those aged 20 years and older and for COPD, for those aged 35 years and older.
For COPD, the prevalence of COPD was reported among those with and without each of the comorbid conditions. Therefore the prevalence of COPD was calculated among those with and without diabetes, mood and/or anxiety disorders, hypertension and asthma. The prevalence was calculated among those aged 35 years and older among all four comorbid diseases or conditions, corresponding to the reporting age for COPD.
The following case definitions were used for the comorbid diseases and conditions:
Diabetes
Hypertension
Mood and/or Anxiety Disorder
Individuals aged one and older with at least one physician billing claim listing a mood and/or anxiety diagnostic code in the first field, or one hospital discharge abstract listing a mood and/or anxiety diagnostic code in the most responsible diagnosis field in a one-year period.
Don’t Miss: How To Get Rid Of Asthma Without Inhaler
Knowing The Differences Between Copd And Asthma Is Vital To Good Practice
This content was published in 2011. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
The Outcomes strategy for people with chronic obstructive pulmonary disease and asthma was launched in July 2011 by the Department of Health, with the overall aim to drive improvements in outcomes for patients.1 Once implemented, it is expected to help people to avoid lung disease and lead longer and healthier lives. The strategy recognises the role of community pharmacy in supporting the management of people with respiratory disease through medicines use reviews and new pharmacy services.
In addition, the introduction of national target groups for MURs in England, under amendments to the NHS Community Pharmacy Contractual Framework, aims to ensure the service is provided to those who will benefit most. One of the target groups is patients with asthma or COPD.2 Both diseases have a major impact in the UK in terms of mortality and morbidity3 and the aim of MURs with these patients is to support them to take their medicines as intended, increase their engagement with their condition and medicines, and promote healthy lifestyles, in particular stopping smoking.
Figure 1 Symptom Overlap For Asthma And Chronic Obstructive Pulmonary Disease
In fact, the three most common presenting symptoms of COPD are dyspnea, cough, and sputum production. Where the disease symptomology differs is with wheezing and chest tightness, which typically are less common in COPD.20 Commonly, patients will present with symptoms of fatigue, unaware that the underlying cause is dyspnea on exertion. This happens more often in less active patients in whom the dyspnea becomes progressively more severe over time. It also is common for patients to present with a chronic cough productive of green sputum. This cough typically is more intense in the morning and resolves throughout the day. Patients also can present with a constellation of the symptoms mentioned earlier, with dyspnea plus cough plus breathlessness plus wheezing, etc. With or without fever, securing a COPD diagnosis with such a presentation can be difficult, and the differential diagnosis list can be quite long.
Also Check: How To Breathe Better With Asthma Without An Inhaler
What Are The Stages Of Copd
Doctors generally use the Global Initiative for Chronic Obstructive Lung Disease Program to stage COPD. These staging guidelines have been proven to be consistent and accurate by doctors and scientists. Other methods can be used to stage COPD, but they may be influenced by other factors.
There are many treatment options and ways to manage COPD. The newest 2017 guidelines emphasize the use of combined bronchodilators as first-line therapy for COPD. Doctors recommend vaccinations for people with the condition to decrease the risk of lower respiratory tract infections. Alterations in health-related behaviors is emphasized. Spirometry measurements can help determine the extent of obstructive lung disease. As COPD progresses, oxygen therapy, especially if you have obstructive sleep apnea, may help improve your survival.
Like COPD, there are many treatment options and ways to manage asthma. Your primary care doctor and/or an allergist will discuss and suggest the best choice of treatment and management drugs for you. Medications used include corticosteroids, short acting beta agonists , and occasionally anticholinergic medications for severe exacerbations.
Emergency treatment of life-threatening asthma or COPD may involve intravenous corticosteroids, intubation, mechanical ventilation, and oxygen treatment until the crisis is resolved.
How Is Chronic Obstructive Pulmonary Disease Diagnosed
To assess your lungs and overall health, your healthcare provider will take your medical history, perform a physical exam and order some tests, like breathing tests.
Medical history
To diagnose COPD, your provider will ask questions like:
- Do you smoke?
- Have you had long-term exposure to dust or air pollutants?
- Do other members of your family have COPD?
- Do you get short of breath with exercise? When resting?
- Have you been coughing or wheezing for a long time?
- Do you cough up phlegm?
Physical exam
To help with the diagnosis, your provider will do a physical exam that includes:
- Listening to your lungs and heart.
- Checking your blood pressure and pulse.
- Examining your nose and throat.
- Checking your feet and ankles for swelling.
Tests
Providers use a simple test called spirometry to see how well your lungs work. For this test, you blow air into a tube attached to a machine. This lung function test measures how much air you can breathe out and how fast you can do it.
Your provider may also want to run a few other tests, such as:
- Pulse oximetry to measure the oxygen in your blood.
- Arterial blood gases to check your oxygen and carbon dioxide levels.
- Electrocardiogram to check heart function and rule out heart disease as a cause of shortness of breath.
- Chest X-ray or chest CT scan to look for lung changes that are caused by COPD.
- Exercise testing to determine if the oxygen level in your blood drops when you exercise.
You May Like: Does Asthma Shorten Life Expectancy
