Risk Factors Of Acute Asthma
In addition to the triggers that can cause an asthma attack, there are a few risk factors that can increase the chances of an attack occurring.
-
Changes in medication Reduction or cessation of certain medications or the use of certain medications in common may increase the possibility of an attack
-
Non-adherence to medication In addition to changes in medication, patients who do not adhere to the medication prescribed to them are at increased risk of exacerbation
-
Smoking The damaging effects of smoking on the lungs also makes smokers more likely to have an asthma attack
-
Coughing at night The risk of an acute asthma attack goes up in relation to the number of nights in a row you experience a troublesome cough
-
Obesity People with a BMI greater than 30 are more likely to have asthma
Know The 4 Steps Of Asthma First Aid
Its important for everyone in the community to know the 4 steps of asthma first aid.
One of the most common reliever medications in Australia is salbutamol, often known as your blue puffer. These are available over the counter from a chemist.
If you are not sure if someone is having an asthma attack, you can still use blue reliever medication because it is unlikely to cause harm.Call triple zero immediately if:
- the person is not breathing
- their asthma suddenly becomes worse or is not improving
- the person is having an asthma attack and theres no reliever medication available
- the person is unsure if it is asthma
- the person is known to have anaphylaxis. If this is the case, ALWAYS GIVE ADRENALINE AUTOINJECTOR FIRST, and then reliever, even if there are no skin symptoms.
What Should I Know About Covid
If you have asthma that is moderate-to-severe, or if your asthma symptoms arent well controlled, youre at greater risk of having to be hospitalized if you get COVID-19. Therefore, you should wear a mask if you go to indoor spaces with other people, get vaccinated and avoid exposure to people who have the virus.
A note from Cleveland Clinic
Many people live fulfilling lives with asthma. Some professional athletes with asthma have set records in their sports. Your healthcare provider can help you find the best way to manage your asthma. Talk to your healthcare provider about how to control your symptoms.
Last reviewed by a Cleveland Clinic medical professional on 01/19/2022.
References
Recommended Reading: How To Beat Asthma Naturally
What Types Of Asthma Are There
Asthma is broken down into types based on the cause and the severity of symptoms. Healthcare providers identify asthma as:
- Intermittent: This type of asthma comes and goes so you can feel normal in between asthma flares.
- Persistent: Persistent asthma means you have symptoms much of the time. Symptoms can be mild, moderate or severe. Healthcare providers base asthma severity on how often you have symptoms. They also consider how well you can do things during an attack.
Asthma has multiple causes:
- Allergic: Some peoples allergies can cause an asthma attack. Allergens include things like molds, pollens and pet dander.
- Non-allergic: Outside factors can cause asthma to flare up. Exercise, stress, illness and weather may cause a flare.
Asthma can also be:
- Adult-onset: This type of asthma starts after the age of 18.
- Pediatric: Also called childhood asthma, this type of asthma often begins before the age of 5, and can occur in infants and toddlers. Children may outgrow asthma. You should make sure that you discuss it with your provider before you decide whether your child needs to have an inhaler available in case they have an asthma attack. Your childs healthcare provider can help you understand the risks.
In addition, there are these types of asthma:
Introduction And Evolution Of Corticosteroids In The Management Of Asthma: Historical Background
Shortly after the discovery of the structure of adrenal steroid hormones, Hench et al. examined using cortisone to treat arthritis in 1949. The effect was remarkable and that work won the Nobel Prize the next year. It also started a series of trials of corticosteroids in various inflammatory conditions. The first use of corticosteroid to treat acute asthma exacerbation was in 1956. Development of corticosteroids that have less mineralocorticoid activity, like prednisone, and later those that have no mineralocorticoid activity, like dexamethasone, made corticosteroids more attractive therapies to use in asthma. In 1972, Clark showed for the 1st time that inhaled beclomethasone was effective in the management of asthma with less adverse effects than systemic steroids. Numerous reports came afterwards describing the efficacy of oral prednisone and prednisolone , IV methylprednisolone and ICS such as triamcinolone, budesonide, and fluticasone in the management of asthma. These effects are mediated through various genomic and nongenomic mechanisms. Table 2 shows some common systemic corticosteroids and their relative potency.
Recommended Reading: How To Strengthen Lungs With Asthma
When Responding To An Asthma Attack When Should You Contact Emergency Services
If you are experiencing an asthma attack, you should contact emergency services immediately. During an asthma attack, the airways narrow and make it difficult to breathe. This can be a life-threatening situation. emergency services can provide you with the treatment you need to help you breathe easier and prevent further complications.
The most common long-term disease in children is asthma, which affects the lungs. Severe asthma attacks and asthma attacks usually cause coughing, shortness of breath, chest tightness, and a shortness of breath. A variety of environmental factors can be used to cause asthma attacks. There is no cure for asthma, and the only cure is an attack response. Difficulty breathing can be extremely frightening, and sufferers can be extremely distressed. Make sure the person has a comfortable breathing position and is comfortable with their temperature. An asthma attack may be the result of a rare attack, which may not have previously been diagnosed with asthma.
Definition And Importance Of Asthma Exacerbations
The long-term goals for management of asthma are to achieve good control of symptoms, maintain normal activity, and minimize the risk of asthma exacerbation. However, even with optimal care, approximately 10% of patients with asthma will experience a major exacerbation that requires oral corticosteroids, an emergency department visit, or hospitalization once a year.
Exacerbations of asthma are defined as a progressive increase in symptoms of shortness of breath, cough, or wheezing sufficient to require a change in therapy. Usually exacerbations occur in patients with preexisting asthma but can be the first presentation of asthma. Most often, asthma flares or asthma attacks occur as the result of a viral upper respiratory infection, exposure to an allergy, or the result of poor adherence to controller medications.
Also Check: Is Allergy Induced Asthma Dangerous
Allergy And Defective Anti
Allergic sensitization is a risk factor for wheezing with RV infection, particularly in children. Whether allergic inflammation often found with sensitization increases the susceptibility for viral infections or enhances their ability to provoke further inflammation is not entirely clear.16 Type I interferons are important innate antiviral responses to respiratory viruses.14, 17 There is evidence that virus-induced interferon generation from peripheral blood mononuclear cells,18, 19, 20 plasmacytoid dendritic cells,21 and bronchial epithelial cells22, 23 is reduced in some patients with allergic asthma . It has been show that IgE occupancy of their membrane receptors inhibits antiviral generation of IFN- from plasmacytoid dendritic cells and may increase susceptibility to RV-induced wheezing and asthma exacerbations . Deficient immune responses to viral infections may be present in type 2 inflammatory conditions with interferon production being inversely correlated with increasing airway eosinophilia, IL-4 levels, and total serum IgE.23 Finally, the use of inhaled IFN- at the time of an upper respiratory infection reduces the airway viral load and improves clinical symptoms in patients with asthma.24
Impaired plasmacytoid dendritic cell IFN- response in patients with allergic asthma. pDCs from patients with physician-diagnosed asthma and allergic sensitization secreted less IFN- on exposure to viruses compared with patients without asthma.
What To Take With You When Going To Hospital With Asthma
If youre at home when you have an asthma emergency and need to go to hospital, it would ideally help if you could take a few things with you. These include:
- Your asthma inhalers
- Your spacer, if you use one
- Any other medications you currently take, for your asthma and other conditions
- A copy of your asthma action plan this will help medics see your asthma triggers, your peak flow and other relevant
Taking these items with you will help the medics to treat you. However, they are not essential, so dont worry if youre not able to take them with you.
Read Also: Do Inhalers Make Asthma Worse
Asthma Symptoms In A Severe Allergic Reaction
People having a severe allergic reaction can also have asthma-like symptoms. If the person has an anaphylaxis action plan, follow the instructions.
Always give adrenaline injector first, then asthma reliever if someone with known asthma and allergy to food, insects or medication has sudden breathing difficulty even if there are no skin symptoms. In case of an emergency, call triple zero and ask for an ambulance.
Patients At Risk For Severe Asthma Exacerbations
Careful consideration should be carried out in patients with risk factors for severe asthma exacerbations. Patients with exacerbations that led to endotracheal intubation, previous admissions to the ICU, a history of multiple hospitalizations in the past year or multiple emergency department visits in the past month, the need of chronic oral corticosteroids use, poor access to health care, and frequent use of rescue inhalers are considered to have increased risk of severe asthma exacerbations and death. Patients with asthma and with these characteristics should be evaluated promptly and treated expeditiously. In addition, a minority of patients with asthma may experience a significant decline in lung function without a change in symptoms. These under-perceivers are at higher risk for near-fatal exacerbations. This article focuses on the approach to manage exacerbations of asthma.
Also Check: What Happens During An Asthma Attack
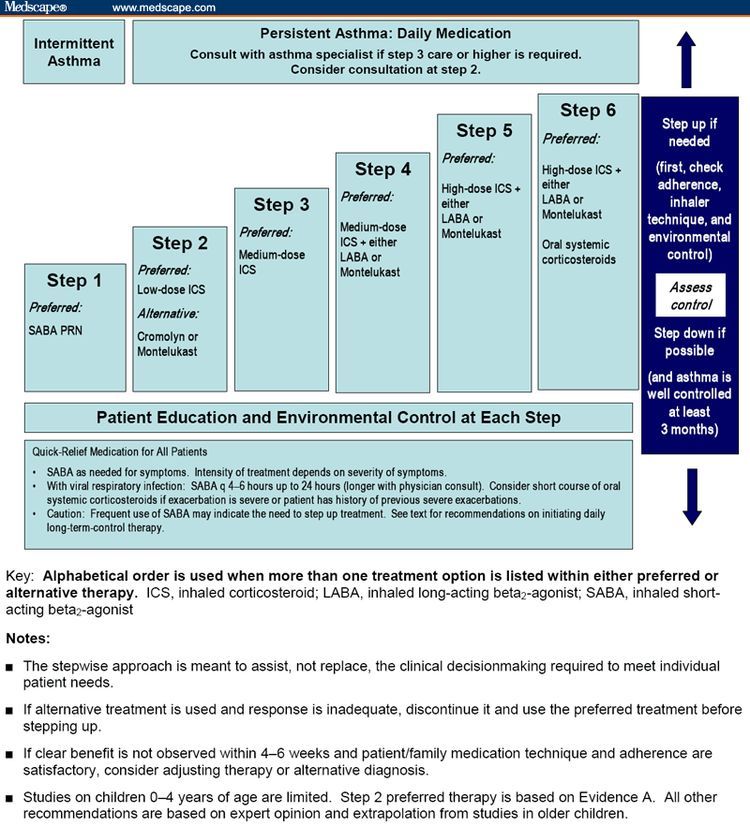
Postdischarge Therapy And Importance Of An Action Plan
Before discharge from the hospital or the emergency department, arrangements for follow-up within 12 weeks should be made for patients. Patients who are hospitalized for their asthma may be especially receptive to information and advice about how to control symptoms and avoid future exacerbations. Health-care providers or an asthma educator should provide detailed education to all patients before discharge. Discussion should assure that the patient understands the cause of his or her exacerbation, modifiable risks factors , the purpose and correct use of medications, and an updated asthma action plan. The action plan should identify each discharge medication, the dose, and frequency. It should also outline how often to take the quick reliever medications if symptoms increase or PEF/FEV1 decreases, when to consider taking oral corticosteroids, and how to reach their primary care provider or obtain emergency care if their asthma does not respond to a step-up in therapy. Patients > 5 y of age usually are discharged with a flow meter, with instructions to keep track of their values until they are seen in follow-up. This is especially important for patients with brittle asthma or for patients identified at risk for near-fatal exacerbations of asthma. Patients should demonstrate the proper use of their inhalers and be discharged with a sufficient quantity of medication to last for at least 12 months.
Why Asthma Can Be Worse In Winter And Steps To Manage Attacks
Asthma is a chronic condition that affects nearly 25 million people in America. Its a respiratory disease that makes breathing difficult and often comes with lung spasms, wheezing, and chest tightness.
Your lungs are made of bronchi that transport air to and from your lungs. If you have asthma, your airways are easily inflamed. Inflamed airways swell, closing your breathing passages and making it hard for air to reach your lungs.
Changes in your environment like weather, dust, and smoke can make your lungs extra sensitive. For many asthmatics, winter weather brings more frequent asthma attacks. The doctors at Wasatch Peak Family Practice can help you find an asthma treatment plan that works with your lifestyle.
One of the best things you can do to prevent and manage asthma attacks in winter is to understand your triggers and know your treatment plan. Let us help you understand your asthma and how to control it.
Dont Miss: How To Control Asthma By Yoga
Also Check: What Are The Symptoms Of Bronchial Asthma
Will My Wheezing Or Coughing Be Worse
Not necessarily. You might be surprised to learn that you may not have more of these than usual during a severe asthma attack. So donât judge how bad your asthma attack is based on how much you wheeze or cough.
In fact, very severe asthma attacks may affect your airways so much that you donât get enough air in and out of your lungs to make a wheezing sound or cough.
Inhaler Devices For Asthma Medication
Some people need extra help to take their asthma medication and make it work more effectively.
Work with your doctor to decide which device is best for you.Inhalers are the most common devices for asthma medication. The 3 main types of inhaler devices are:
- Metered-dose inhaler an aerosol canister that produces a fine mist of medication. Always shake the canister before use. It is recommended to always use a spacer with your puffer.
- Breath-activated inhaler a spring-loaded aerosol canister. The medication automatically mists out when you start to breathe in through the mouthpiece. These are good for children and for people who find it hard to coordinate a puffer.
- Dry-powder inhalers contain medication as a dry powder, rather than liquid like aerosol inhalers. Deep breathing is required to release medication to the lungs. Young children and anyone who struggles with shortness of breath may find these difficult to use.
Watch National Asthma Council videos which show you how to use different types of inhalers, including this video on how to use a standard metered-dose inhaler.
Some other types of medication may be used for more severe asthma. Your doctor may prescribe these additional therapies or refer you to a respiratory specialist.
You May Like: Developing Asthma Later In Life
Clinical And Objective Assessment
History should be collected very carefully since it is an extremely important tool to predict the severity of exacerbations and the risk for hospitalization. Symptoms are poorly related to the severity of airway obstruction. Therefore, objective evaluations should be considered . However, the value of pulmonary function parameters in the assessment of patients with respiratory distress is modest . Only three high quality studies are available . One is a systematic review of 60 studies showing that none of the available score are validated in the clinical practice . The other one is an observational prospective study including 101 children, aged > 6 years, demonstrating that the Clinical Asthma Score was not related to the spirometry results . More recently Eggink and collaborators performed a prospective, high quality study, reviewed and validated clinical scores for dyspnoea severity in children, and authors concluded that the commonly used dyspnoea scores have insufficient validity and reliability to allow for clinical use without caution .
Table 1 Management of acute asthma attack in children
Causes Of Acute Asthma
An acute asthma attack can be caused by several triggers. With experience and the help of your doctor, youll be able to identify the triggers that are most likely to affect you. Common triggers include:
-
Respiratory tract infections This includes lower tract infections such as pneumonia, bronchitis, and tuberculosis as well as upper tract infections like pharyngitis, laryngitis, sinusitis, flu, and cold
-
Allergens These include pollen, dander, or other allergens that affect the respiratory system, including household pests, such as dust mites, mice, and cockroaches
-
Exposure to pollution Strong inhaled pollutants such as chemical fumes, strong odors, and smoke can trigger an attack
Read Also: How Long Does Asthma Cough Last
Complications Of Acute Asthma
If asthma is well controlled, it will usually have minimal impact on your lifestyle. However, an asthma attack can interfere with work, school, sleep, and recreational activities. Having poorly controlled asthma makes this worse.
In extreme circumstances, a severe asthma attack can result in death. Thankfully, the number of deaths due to asthma is declining. In 2016, asthma was an underlying cause of death in only 10 people per million. The chances of an asthma attack resulting in death increase with age.
Management Of Status Asthmaticus In The Icu
Patients admitted to the ICU include individuals who require ventilator support or those with severe asthma for whom therapy failed. Most often they have refractory hypercapnia, persisting or worsening hypoxemia, deteriorating PEF/FEV1, drowsiness, confusion, or impending signs of respiratory arrest. Elective intubation by an experienced clinician is always recommended as soon as signs of deterioration are present. Intubation and mechanical ventilation may lead to hypotension and barotrauma secondary to high positive intrathoracic pressures. Care must be taken to assure that intravascular volume is adequate before intubation, and a bolus of intravenous normal saline solution is often recommended before initiation of mechanical ventilation.
Although there are no studies that determined the optimal mode of mechanical ventilation, it seems prudent to use the mode with which one is most familiar. Most researchers have recommended an initial minute ventilation of 90130 mL/kg ideal body weight , with further adjustments based on pH and the plateau airway pressure. Based on studies by Tuxen and Lane and Peters et al, we usually use a tidal volume of 89 mL/kg with a breathing frequency of 1014 breaths/min, a flow of 100 L/s, and 0 PEEP. However, many institutions prefer to use tidal volumes of 68 mL/kg ideal body weight., We adjust the setting to maintain a plateau pressure of 30 cm H2O and judiciously adjust ventilator-applied PEEP based on its ability to lower intrinsic PEEP.
Also Check: What Happens When You Use An Inhaler Without Asthma
