How Many People Die From Asthma
- On average, ten Americans die from asthma each day. In 2019, 3,524 people died from asthma. Many of these deaths are avoidable with proper treatment and care.7
- Adults are five times more likely to die from asthma than children.7
- Women are more likely to die from asthma than men, and boys are more likely than girls.7
- Black Americans are nearly three times more likely to die from asthma than white Americans.7
What Are The Symptoms
Asthma can be different for everyone. Asthma symptoms can also vary over time, with few or no symptoms when asthma is well controlled. The common signs and symptoms of poorly controlled asthma include:
- Shortness of breath
- Trouble sleeping because of breathing difficulty
- Being unable to take part in physical activities without breathing difficulty
These symptoms can occur slowly over hours or days, or they can come on as sudden, recurring attacks after which the symptoms can persist for some time before disappearing. If left untreated, asthma can cause permanent structural changes in your airways called airway remodelling, which is why it is important to get your asthma under control and keep treating it over the long term.
Severe Difficult To Control Asthma Steroid
Children that do not seem to respond to standard treatment are referred to as severe or difficult to control asthma, and these children experience substantial morbidity from asthma symptoms. To classify a child into this phenotype, the first step is to exclude an incorrect diagnosis, poor adherence to treatment, or incorrect technique with an inhaler and spacer . Supervised asthma therapy programs can be extremely useful in managing asthma symptoms and reducing healthcare utilization for children with poor medication adherence and inhaler and spacer technique . It is important to differentiate between severe therapy-resistant asthma and difficult-to-treat asthma due to comorbidities Difficult to treat asthma is a much more common reason for persistent symptoms and exacerbations and can be managed if comorbidities, such as allergic rhinitis and chronic exposure to asthma triggers, are directly targeted. Home visiting programs and assessment of the school environment are important features of the evaluation for children with concern for chronic exposure to asthma triggers . Children with persistent symptoms and exacerbations despite correct inhaler technique and good medical adherence to standard asthma therapy should be referred to an asthma specialist to consider more potent biologic therapies such as anti-IgE, anti-IL-5, or anti-IL-13 therapies and further evaluation .
Recommended Reading: How To Calm Down Asthma Symptoms
Can You Get Asthma When You Get Older
As you know from the stats above, more adults than children have asthma. Of course, that poses the question: When in life did they start showing symptoms? Have they had asthma all their lives? Can asthma develop in older individuals?
The answer is yes, it can. If youre 20 or older, you can have what is known as adult-onset asthma. This can affect people at any age, including their 30s through their 60s and even older. That means its always important to prioritize your health, because even if youve had a life free of asthma so far, that can change.
If you have pet allergies , other air borne allergies, youre obese, youve recently had the flu or a cold, or youre a woman with fluctuating hormone levels, such as a recent pregnancy or menopause, you could get adult-onset asthma.
Theres also whats known as occupational asthma. This is when the environmental factors at your place of work lead to the development of asthma. These factors may include breathing in excessive perfume, feather beds, dust, mold, tobacco smoke and other smoke.
The symptoms of adult-onset asthma and occupational asthma are often the same as those outlined above.
Introduction To Childhood Asthma
Childhood asthma is not a singular disease, but rather a uniquely diverse disorder with variable presentation throughout childhood. Asthma affects 8.3% of children in the United States and is the most common chronic disease of childhood . Childhood asthma is responsible for 50 billion dollars in annual healthcare expenditures and is a major cause of emergency room visits, hospital admissions, school absences, and loss of parental workdays .
Asthma is characterized by inflammation leading to bronchoconstriction, edema, and increased mucous production in the airways. Interestingly, the disorder is more prevalent in boys in the first decade of life. However, after puberty and in the second decade of life, it appears that asthma is more prevalent in young women . Asthma disproportionately affects minority and low-income children with African American and Hispanic children having the highest prevalence rates, morbidity and mortality due to asthma .
Asthma is considered a chronic disease of childhood however there are periods of time during which disease can go into remission or resolve altogether. Important risk factors for the development of childhood asthma have been identified. The phenotypes of childhood asthma and varied presentations are best defined through the periods of the pediatric life course and are described herein.
Also Check: Asthma And Marijuana
What Do The Two Types Have In Common
Exact causes of asthma can be difficult to pinpoint. Allergies and triggers in the environment can cause asthma symptoms and an asthma flare-up, and genetics can also play a role. But the exact reasons why people develop asthma remain unclear.
Childhood asthma and adult-onset asthma share many of the same triggers. For all people with asthma, exposure to one of the following triggers may cause an asthma attack, though different people have different triggers:
- smoke
Childhood Asthma Risk Factors
The perinatal period has been implicated in the development of childhood asthma. Several cohort studies have unveiled risk factors for the development of asthma in offspring, with factors that span from genetic and environmental risk factors to features such as child’s sex and presence of atopy.
Genetic Risk Factors
Environmental Risk Factors
Environmental perinatal risk factors are also important to consider for childhood asthma. Maternal tobacco smoking during pregnancy has been shown to increase the risk of childhood asthma . Maternal diet in pregnancy has also been implicated as an asthma risk factor with reports of maternal diets higher in vitamin E, zinc, and polyunsaturated fatty acids as protective against the development of childhood asthma . In contrast, high sugar intake in the maternal diet during pregnancy has been associated with increased risk of asthma in offspring . Other maternal dietary factors have been studied but with less conclusive results including the intake of vitamin D, vitamin C, and a Mediterranean diet. Other perinatal risk factors for childhood asthma that have been reported are neonatal jaundice, maternal preeclampsia, and cesarean section delivery, all which have been associated with higher risk of childhood asthma development .
Ultimately gene-environment interactions are critical for the development of asthma in a child .
Natal Risk Factors
Sex
Family History
Medical History
Medication Exposure
Read Also: What Happens When You Have Asthma
What Are Signs And Symptoms Of Adult Onset Asthma
Regardless of age, asthma symptoms can include:
Dry cough, especially at night or in response to specific triggers
Tightness or pressure in the chest
Wheezing a whistling sound when exhaling
Shortness of breath after exercise or physical exertion
Difficulty breathing
Colds that go to the chest or hang on for 10 days or more
Presentation Of Asthma: Early Childhood
Studies of asthma’s natural history have shown that almost 80% of cases begin during the first 6 years of life . The symptoms of pediatric asthma in this age group are varied and not specific to asthma making the diagnosis challenging. The primary symptoms of asthma in infancy and early childhood include cough, both dry and productive , wheeze, shortness of breath, and work of breathing. Asthma symptoms are a result of airway inflammation, bronchospasm, airway edema, and airway mucous gland hypertrophy. Interestingly, these symptoms can also present with a multitude of other pediatric diseases including respiratory tract infections and congenital airway anomalies posing a diagnostic challenge. It is well-established that asthma in this age group is frequently under-diagnosed and undertreated .
Often in this age group, particularly over 03 years, symptoms are virally triggered rather than allergically triggered. Infants will often have very few symptoms until they experience an upper respiratory infection, which can trigger a significant and severe inflammatory cascade.
Also Check: Can I Join The Coast Guard With Asthma
What Further Information Do We Need About The Burden Of Asthma
Tracking the global burden of asthma dependson the acquisition of new standardised data overtime for relevant parameters including, at least,prevalence, disability and mortality. It is becomingclear that asthma is a heterogeneous disease,with diverse causes, life-courses, outcomes andoptimal treatments . In further work onthe burden of asthma, including both disabilityand premature mortality, it would be useful tolink this burden to avoidable causes and treatabletraits. This would highlight the potential value ofinterventions to prevent asthma and mitigate theconsequences of asthma with effective treatment.
Guy Marks, Neil Pearce, David Strachan, Innes Asher, Philippa Ellwood
Canadian Chronic Disease Surveillance System
The CCDSS is a collaborative network of provincial and territorial chronic disease surveillance systems, led by the Public Health Agency of Canada . The CCDSS identifies chronic disease cases from provincial and territorial administrative health databases, including physician billing claims and hospital discharge abstract records, linked to provincial and territorial health insurance registry records using a unique personal identifier. Data on all residents eligible for provincial or territorial health insurance are captured in the health insurance registries thus, the CCDSS coverage is near-universal with the exception of some small populations. Case definitions are applied to these linked databases and data are then aggregated at the provincial and territorial level before being submitted to PHAC for reporting at the provincial, territorial and national levels.
The CCDSS has expanded from its initial mandate of diabetes surveillance to include data on several additional chronic diseases and conditions including: hypertension, mental illness, mood and/or anxiety disorders, heart failure, ischemic heart disease, acute myocardial infarction, stroke, osteoporosis, arthritis and neurological conditions. Asthma and COPD were added to the CCDSS in 2012.
The data presented in this report and subsequent updates can be accessed on the Public Health Agency of Canada’s Public Health Infobase.
Also Check: How Can You Tell If You Have Asthma
Asthma In The Canadian Population
CCDSS Case Definitions
Prevalent Asthma Case Definition
The case definition of diagnosed asthma is: an individual aged one year and older having at least two visits to a physician with a diagnosis of asthma in the first diagnostic field in a two-year period, or at least one hospital separation with a diagnosis of asthma ever in any diagnostic field, coded by the International Classification of Diseases , ninth revision or ICD-9-CM 493 or ICD-10-CA J45-46. This case definition for asthma was validated by two independent studies in Ontario.Footnote 17Footnote 18
Only the first diagnostic field was used in physician billing claims data as not all provinces and territories had more than one diagnostic field. All fields were included from the hospital separation file as this database allows for the recording of up to 25 diagnoses.
Based on this definition, once a case is detected, it is a prevalent case for life regardless of future contact with health services. Consequently, once someone is identified as a case, they are always included in the database as a case. All jurisdictions identified cases occurring as of 1995, with the exception of Quebec which began in 1996 and Nunavut which began in 2005.
Active Asthma Case Definition
Incident Asthma Case Definition
Denominator Definition
Prevalence
Asthma
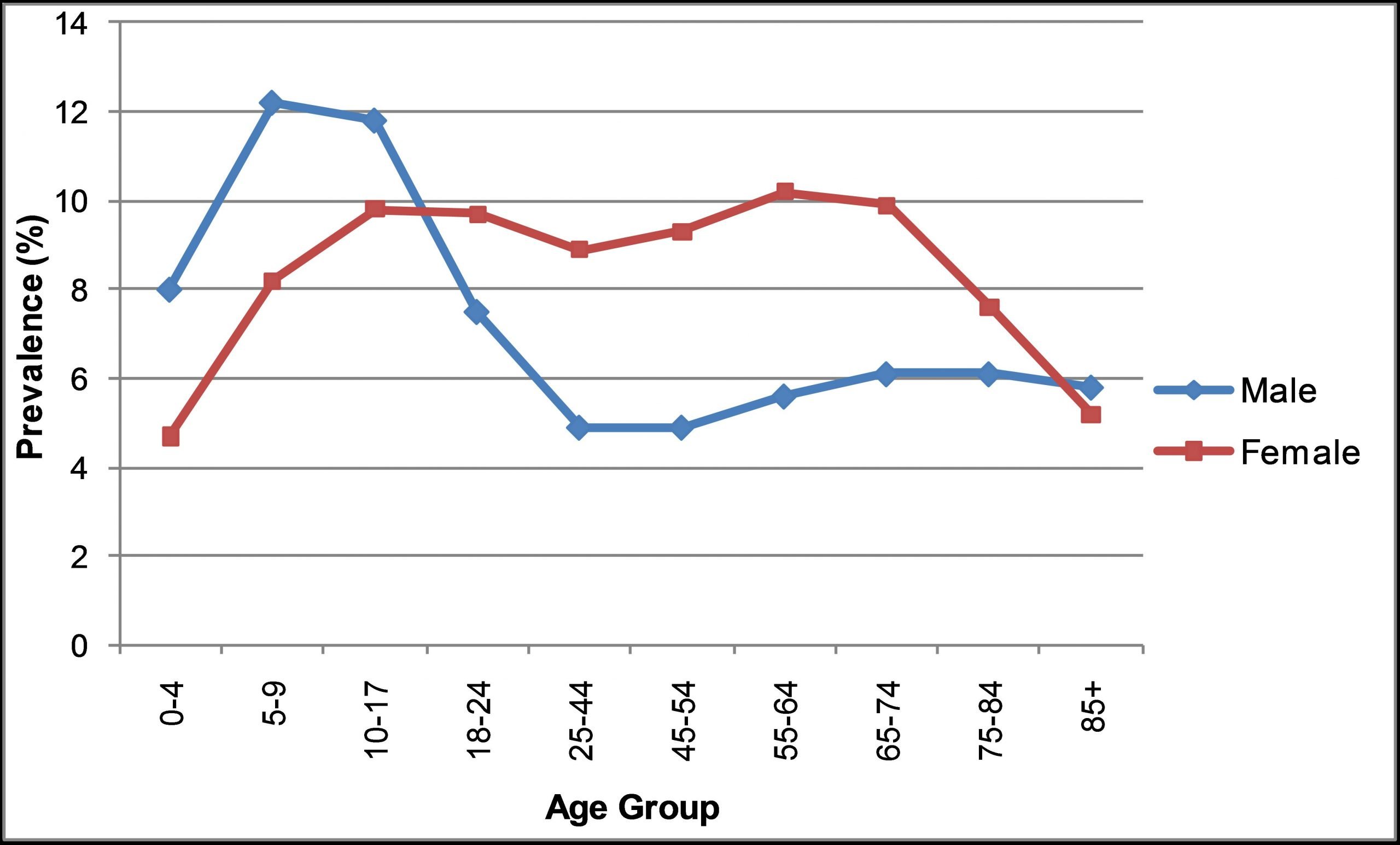
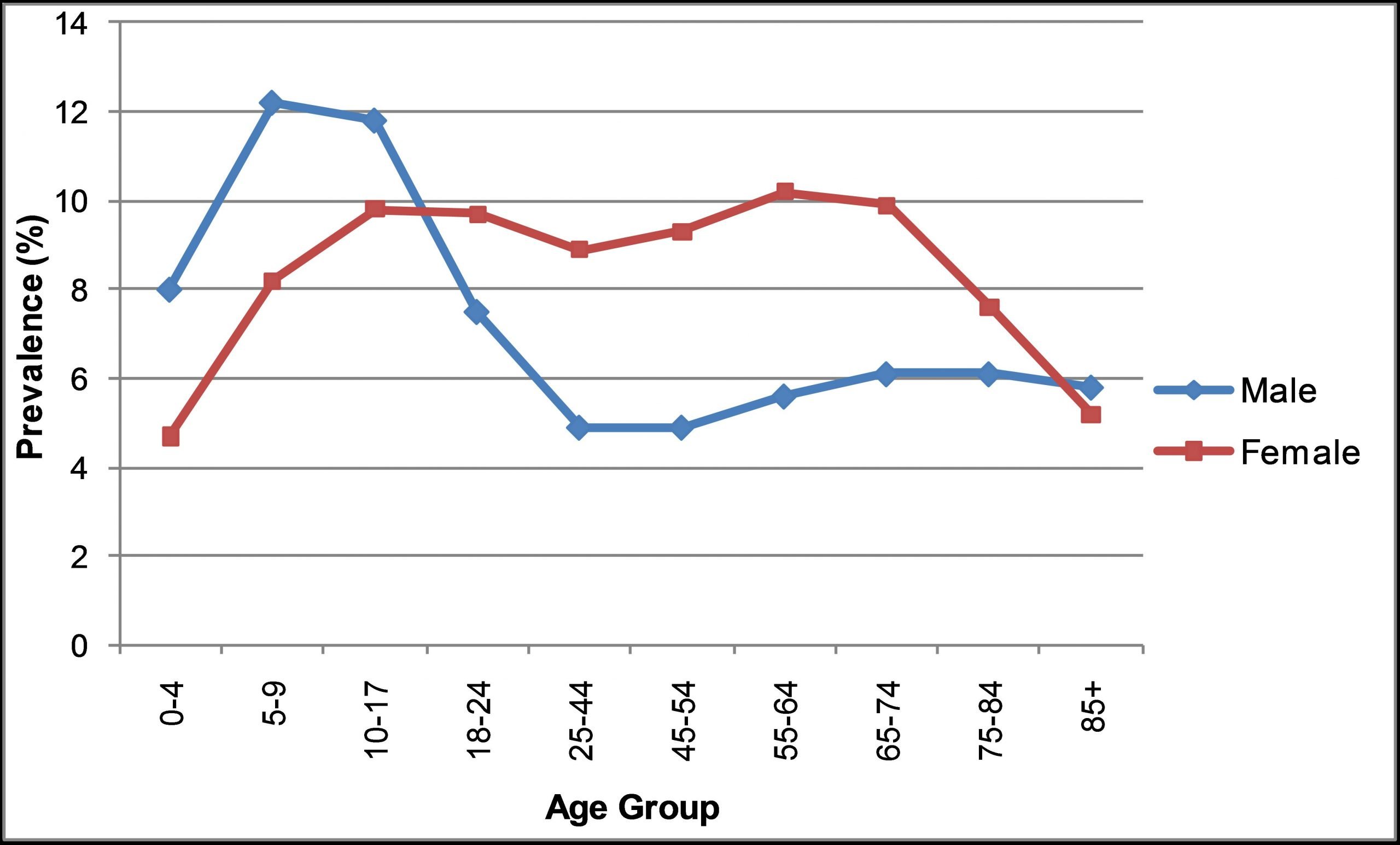
Figure 1.1 Prevalence of diagnosed asthma among Canadians aged one year and older, by age group and sex, Canada, 2011-2012
Active Asthma
Incidence
All-cause Mortality
Comorbidity
How Many People Died From Asthma In Each Uk Region In 200812
England: Death rates for asthma in the West Midlands and the South East were higher than in other parts of the UK. The South West had the lowest asthma mortality rate.
Scotland, Wales and Northern Ireland: Asthma death rates were similar to the UK generally.
Asthma mortality ratios by UK regions, males and females, 200812
Relative risk of death from asthma, by local authority district , 200812
Relative risk is used in medical research to compare risk in different groups of people. In the maps we show the risk of an area relative to the average for Scotland, England and Wales. Here we show whether the group of people living in a particular area have a risk of dying from asthma that is lower or higher than the average. Because of the way relative risk is calculated there must always be some areas above average and some below average.
You can find out how these figures were calculated.
Also Check: Asthma Chromosome
What Is The Best Way To Live With Asthma
The key to good living with asthma is developing a strong partnership between patients, caregivers, and physicians. Practical steps include the following:
Make an asthma care management plan with your physician. An asthma management plan helps you understand what to do when specific situations arise. Each time you visit the physician, talk about your plan, and make any necessary changes.
Educate yourself. Stay informed about the latest developments in asthma and allergy care and treatment. Ask your physician about new medications or research findings that may relate to your care.
Get regular medical care. If you have asthma, you should see your physician at least once a year, even if your symptoms are under control. When you become sick, or if you have significant changes in your health, you should also talk with your physician about how your asthma could be affected.
Take your medicine. Your asthma medications will make you feel better and sometimes people think thats the time to stop. Its not! Use your medications as prescribed.
With good management, asthma symptoms can be controlled. Most people who develop adult onset asthma are able to lead normal lives. Expect success!
Is Asthma Embarrassing
Interestingly, feeling less confident does not necessarily mean feeling embarrassed about your asthma. Overall, 10% fewer participants reported feeling embarrassed about their asthma in comparison to feeling less confident. However, embarrassment was also a more commonly experienced feeling among individuals in younger age groups. It appears that as you age, asthma feels less socially distressing.
Don’t Miss: Can You Smoke Weed If You Have Asthma
How Common Is Asthma
- Approximately 25 million Americans have asthma. This equals to about 1 in 13 Americans, including 8 percent of adults and 7 percent of children.1
- About 20 million U.S. adults age 18 and over have asthma. 1
- Asthma is more common in adult women than adult men.1
- It is the leading chronic disease in children. 2 Currently, there are about 5.1 million children under the age of 18 with asthma. 1
- Asthma is more common in boys than girls.1
Asthma In Massachusetts Is Costly
- The total charges for hospitalization due to asthma in Massachusetts increased 82.5% from $57 million in 2002 to $104 million in 2013.
- In 2013, public insurance was the expected payer for 66.61% of hospitalizations due to asthma.
Figure 2. Total Charges for Hospitalizations Due to Asthma, Massachusetts Residents, 2002-2013
Disparities Exist in Hospitalizations, Emergency Department Visits, and Outpatient Observation Stays by age, gender and race/ethnicity.
- Adults ages 65 years and older had the 2nd highest rate of hospitalization due to asthma, but had the lowest rates of emergency department visits and outpatient observation stays due to asthma.
- From 2002 through 2013, Black, non-Hispanics and Hispanics consistently had significantly higher age-adjusted rates of hospitalization due to asthma than White, non-Hispanics. Children ages 0-4 years had the highest rates of emergency department visits, outpatient observation stays, and hospitalization due to asthma
Figure 3 Age-Specific Rates of Emergency Department Visits Due to Asthma, Massachusetts Residents, 2009-2013
For more information about Massachusetts asthma statistics, please contact .
Also Check: How To Deal With Asthma Attack Without An Inhaler
Why Do People Get Asthma
Research has yet to show a definitive cause of asthma. However, researchers have determined several risk factors that can lead to asthma development.
Family History and Genetics
Children of mothers with asthma are three times more likely to suffer from asthma, and 2.5 times more likely if the father has asthma. More than 30 genes have been linked to asthma so far, and gene-gene interactions, gene-environment interactions and epigenetic modifications also play a part. Genetic differences also play a role in differences in response to treatment.
Allergies
People are more likely to have asthma if they have certain types of allergies, such ones which can affect the eyes and nose. However, not everyone who has allergies will get asthma and not everyone who has asthma is affected by allergies. Respiratory allergies and some types of asthma are related to an antibody called immunoglobulin E , which the immune system produces in response to allergens. To protect the body, the IgE causes allergic reactions that can affect the eyes, nose, throat, lungs and skin.
Premature Birth
Children born before 37 weeks are at increased risk of developing asthma later in life.
Lung Infections
Babies or small children may be at risk of developing asthma later in life if they had certain lung infections at a very early age.
Occupational Exposures
Hormones
Women can develop adult-onset asthma during or after menopause.
Environment Air Quality
Obesity
Why The Increase In Asthma
What changes over the last several decades can account for the startling rise in asthma rates? It is unlikely that the dust mite and cockroach populations have changed significantly, nor can genetics explain this increase.
One dramatic change in recent decades is the variety of chemicals to which many children are exposed, especially in the indoor air they breathe. New materials are being used in building construction and maintenance. Energy-efficient buildings often have ventilation patterns that recycle the air which contains allergens and pollutants reducing indoor air quality. Consumer products such as furniture, particle board, and synthetic rugs can emit irritants such as formaldehyde. Some products, such as detergents, cleaning products, and deodorizers, can contain chemicals that irritate the respiratory system. Children from a very young age and in utero are exposed to many of these contaminants in different combinations on a daily basis. Public health experts are now raising questions about the impact of exposure to these pollutants.
Other scientists such as Dr. Peyton Eggelston of the Johns Hopkins University Center for Childrens Environmental Health Research believe that the important exposures occur after birth. This research has looked in particular at infectious bacterial and viral exposures that may contribute to onset of the disease.
You May Like: Does Cold Weather Make Asthma Worse
