What Happens During An Asthma Episode
During normal breathing, the airways to the lungs are fully open. This allows air to move in and out of the lungs freely. Asthma causes the airways to change in the following ways:
These changes narrow the airways. Breathing becomes difficult and stressful, like trying to breathe through a straw stuffed with cotton.
Also Check: How To Treat Asthma Attack Without Inhaler
Other Health Conditions May Impact Eosinophilic Asthma
Additional testing could also help you feel better. In people who have severe asthma with frequent flares, I do an extensive workup, says Wechsler. Im trying to identify what type of asthma they have, but also I want to know: What are their comorbidities? What else is going on with them in regard to their asthma? Do they have bad reflux disease? Do they have bad sinus disease? Vocal cord dysfunction? Addressing other health issues in parallel with asthma treatment may help you feel better.
Agents Targeting Corticosteroid Resistance
Several mechanisms that may account for corticosteroid-resistant asthma have been reported including activation of p38 mitogen-activated protein kinase and inflammatory genes regulated through transcription factor nuclear factor-B. P38 mitogen-activated protein kinase is important in the activation of GATA3, the master Th2 cytokine transcription factor. Small molecule p38 inhibitors have been demonstrated to attenuate asthmatic features in mice. However, clinical trials in humans for the treatment of inflammatory disease have been associated with substantial systemic side effects. Phosphoinositide 3-kinase also regulates inflammatory pathways, and activation of the isozyme PI3K by oxidative stress may decrease corticosteroid responsiveness through reductions in histone deacetylase 2, an enzyme targeted by theophylline. Other mechanisms for steroid-refractory asthma may include increased expression of the alternatively spliced variant of the glucocorticoid receptor and increased production of macrophage migratory inhibitory factor, which may block the anti-inflammatory effects of corticosteroids.,
Read Also: What Happens If You Smoke Weed With Asthma
Why Should I Get Tested
If you have asthma and are using your rescue inhaler frequently, if you wake up at night due to asthma symptoms, if you take oral steroids like prednisone, and/or if your asthma attacks have required emergency care, then your asthma might be uncontrolled. A blood test, along with speaking to your primary care provider or an asthma specialist, may help determine if you have e-asthma, and if further evaluation of your asthma is necessary. Talking with your physician about the test results may help identify your type of asthma and additional treatment options to help control your asthma.
The Role Of Eosinophilic Immune Dysfunction In Eosinophilic Asthma
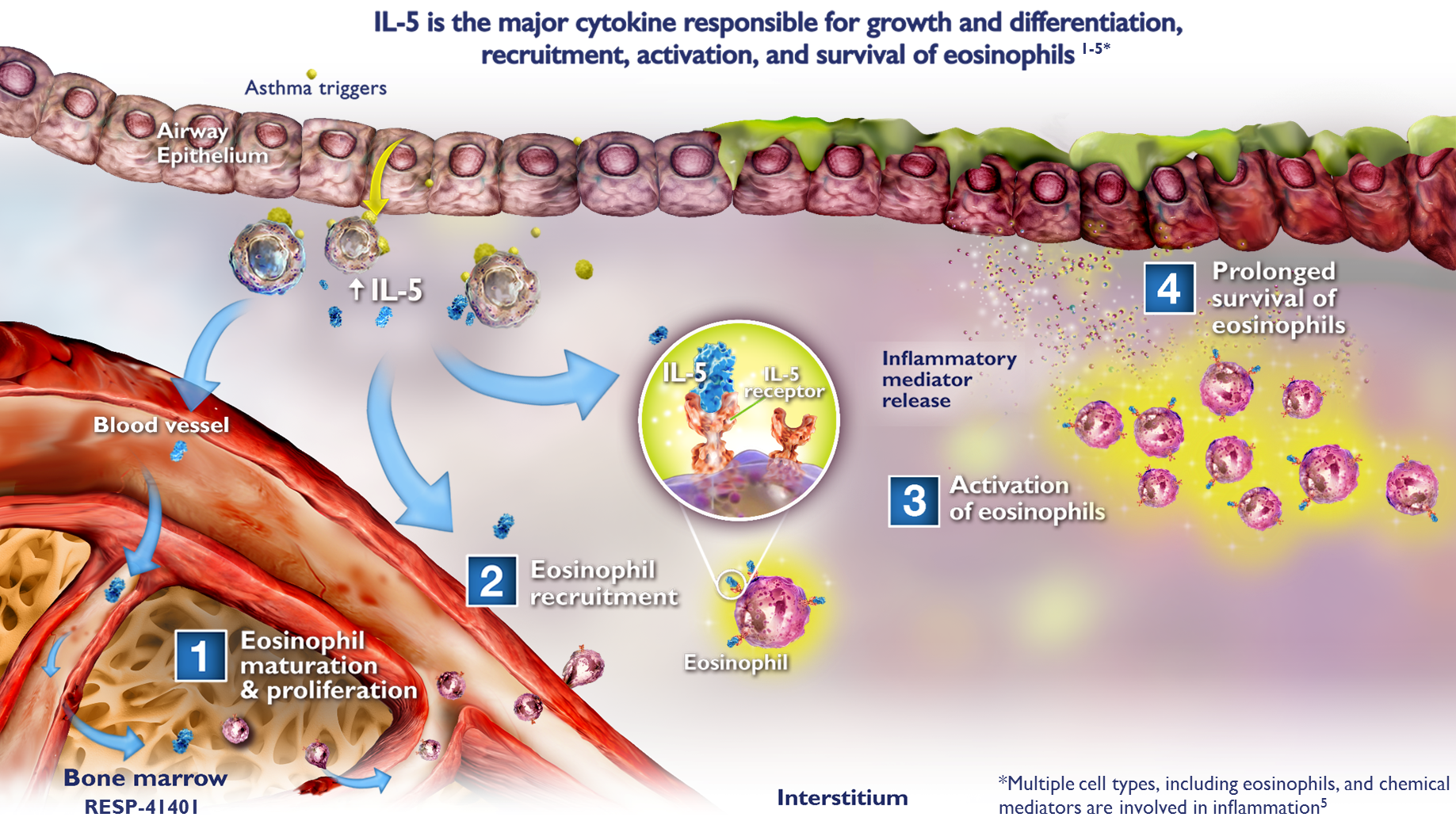
Eosinophils are key effector cells in eosinophilic asthma, where immune system dysfunction leads to eosinophilic inflammation in the airway tissue.6,7
Increasing eosinophil levels in the airway are associated with increasing severity of asthma.8
Eosinophilic asthma patients are at risk of more frequent exacerbations, poorer asthma control, and lower lung function.9-11
Eosinophilic inflammation in the airway tissue12-14
In eosinophilic asthma, immune cells catalyzed by allergic or nonallergic triggers can lead to the production of various cytokines. The cytokines produced by these cells can contribute to the recruitment, activation, and survival of eosinophils.10,15-17
Also Check: What Can Cause Asthma Exacerbation
It Can Take Time To Get A Severe Asthma Diagnosis
Many people with severe asthma have already had asthma for some time and have tried different combinations of drugs. Just as theres no one-off test to diagnose asthma instantly, theres no single test to find out if the type of asthma you have is severe asthma. This means it can take time to get a diagnosis. The process and length of time will vary from person to person.
You can call our Helpline and speak to one of our respiratory nurse specialists on 0300 222 5800 or message them via WhatsApp on 07378 606 728 to ask any questions you have about your new diagnosis.
Next review due June 2022
What Are The Different Lung Function Tests For Asthma
There are several lung function tests for asthma. The most common include:
Recommended Reading: How To Calm Down Asthma Symptoms
New Biologic Agents For Severe Asthma
Nucala
Nucala is an injectable monoclonal antibody which reduces eosinophils in the blood resulting in decreased airway inflammation thus preventing or reducing the severity of asthma attacks. Nucala injections are administered once a month as an add-on treatment to asthma patients standard therapy.
Benefits of Nucala can include:
- Significant reduction in hospitalizations and ER visits due to asthma attacks
- Reduction in occurrences and/or prevention of severe asthma attacks
- Increased quality of life
Nucala injections should be given every 4 weeks even when the patient is feeling better, as biologic agents treat the source of asthma attacks rather than the symptoms. Nucala is not a treatment for sudden breathing problems.
Fasenra
Fasenra is an add-on injectable maintenance treatment for severe eosinophilic asthma patients. As a respiratory biologic agent, Fasenra reduces eosinophils in the blood that trigger airway inflammation resulting in severe asthma attacks. Fasenra is administered once every 4 weeks for the first 3 months, then continued once every 8 weeks thereafter. Because Fasenra is only injected every 8 weeks, it is important to keep your scheduled appointments to maintain treatment success.
Patients using Fasenra have shown:
- Significant improvement in pulmonary function
- Reduced need for oral steroids
- Glaucoma/cataracts
- High blood pressure
- Bone fractures
Box 4 Key Messages For The Diagnosis Of Asthma In Adults
-
The diagnosis of asthma should be suspected in patients with recurrent cough, wheeze and dyspnea in whom no alternative diagnosis can be found and should be confirmed by an objective measurement of lung function or, if normal, by tests for bronchial hyperresponsiveness .
-
A clinical diagnosis of asthma should be prompted by symptoms such as episodic breathlessness, wheezing, cough, sputum and chest tightness .
-
Measurements of lung function by spirometry or peak expiratory flow provide an assessment of the severity of airflow limitation, its reversibility and its variability, and can be used to confirm the diagnosis of asthma .
-
Measurements of allergic status can help to identify risk factors that cause asthma symptoms in individual patients .
-
Because the obstruction observed in asthma is variable, it is possible for the spirometry results to be normal for a patient who has asthma. Options to confirm asthma include bronchial challenge tests, serial peak flow monitoring and measurements of inflammation .
-
For patients with symptoms consistent with asthma who have normal lung function, measurement of airway responsiveness may help to establish the diagnosis .
-
Challenge testing is potentially useful in patients with typical symptoms but normal spirometry results or atypical symptoms or possible occupational asthma .
Read Also: What Happens If You Have Asthma And Smoke Weed
Read Also: How Can You Tell If You Have Asthma
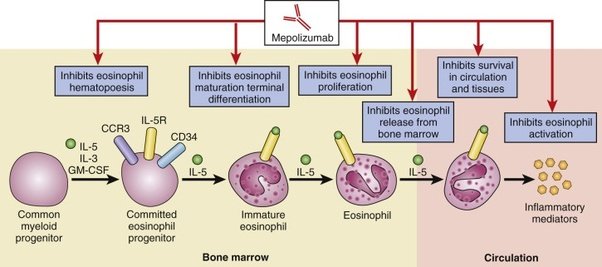
New Medications Are Available To Treat Eosinophilic Asthma
Standard treatments for asthma include long-term controller medications and rescue medications that you use when your symptoms flare up. If these medications arent enough to control your asthma, your doctor may prescribe newer medications called biologics, which target specific molecules involved in the action of eosinophils to help lower eosinophil levels and reduce inflammation. Mepolizumab and reslizumab are antibodies against interleukin 5 molecules benralizumab is an antibody against the IL-5-receptor-alpha-chain. These drugs are delivered by injection or infusion at your doctor’s office. This treatment doesnt necessarily eliminate attacks or exacerbations, but in some people it does, and in other people it reduces them dramatically, says Wechsler.
Talk to your doctor about the treatment plan that’s right for you.
Breathe Easier Baptist Health Is Here To Help
If you suspect that you have eosinophilic asthma, see your Baptist Health primary care physician or allergy specialist. He or she can determine the true nature and extent of your condition, and make recommendations for dealing with it. If your symptoms are severe, call 911 or seek emergency medical care.
You May Like: What Does A Nebulizer Do For Asthma
Asthma Uk Community Forum
My consultant at the Royal Brompton wants me to have a blood test to check for eosinophils when I have an asthma flare up and before starting pred. He is also happy for me to stay on a low dose if I need to, Im currently on a very slow taper. Was just wondering if a low dose of pred 5 or 10mg would affect the results. Has anyone had the blood test while on pred? my cons is hoping I might become candidate for biologicals.
I had a blood test while on 50mg pred a few years back and my eosinophils came back at 0.01, despite my non-pred levels being 1.5-1.7 ish. So I would say a high dose of pred definitely affects eosinophils.
My cons wanted a baseline eosinophil level too a while ago, and he asked me to taper all the way down and be completely off pred for 2-3 weeks before having the bloods, so the levels would be accurate. I have to say it was a bit of a challenge trying to come completely off mid-winter inbetween multiple chest infections! It might be that eosinophils while on 5mg/10mg pred might be closer to your normal, but theyll probably still be lower than they would be off pred completely. The most accurate test would be while off pred , but obviously thats quite a while to go without pred.
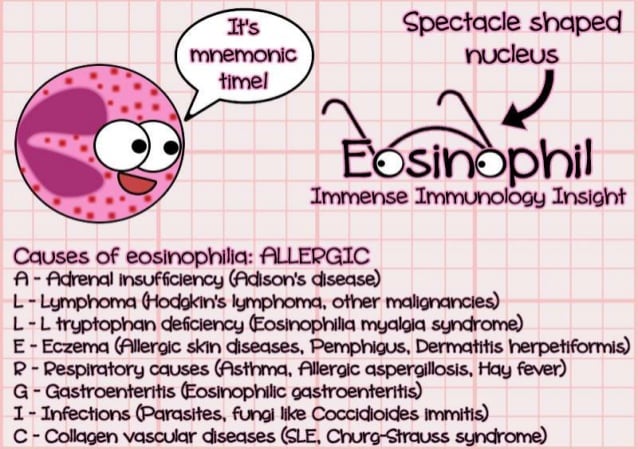
Why Do I Need An Eosinophil Count
Your doctor may discover abnormal eosinophil levels when a white blood count differential is performed. A white blood count differential test is often done alongside a complete blood count and determines the percentage of each kind of white blood cell present in your blood. This test will show if you have an abnormally high or low count of white blood cells. White blood cell counts can vary in certain diseases.
Your doctor may also order this test if they suspect specific diseases or conditions, such as:
- an extreme allergic reaction
Before the test, be sure to tell your doctor about any current medications or supplements youre taking.
A healthcare provider will take a sample of blood from your arm by following these steps:
Don’t Miss: What Can Asthma Do To You
How Is An Asthma Flare
The best thing to do first if your asthma symptoms are getting worse is to use your rescue or quick-relief medicine. Ask your doctor if youre not sure what to use for quick-relief medicine. The usual inhaler dose is two to four puffs every 20 minutes for a total of three doses, or one nebulizer treatment if you have a home nebulizer.
You should be able to tell how serious the flare-up is after you use your quick-relief medicine. If you have a peak flow meter, check your PEF again after you use the quick-relief medicine. If your PEF is still very low, your flare-up is serious.
Your doctor may have given you a written Asthma Action Plan with directions for treating mild, moderate and severe flare-ups. If you dont have an action plan, ask your doctor for written directions about treating asthma flare-ups. If you have the symptoms of a serious flare-up or if your PEF is less than 50 percent of your personal best, call your doctor right away or go directly to the nearest hospital emergency room .
Preparing For A Doctors Appointment
Patients with asthma or suspected asthma will likely be referred to an allergist or a pulmonologist. These tips may help you be more prepared for your appointment:
- Keep a log of symptoms you are having, even if they are seemingly unrelated.
- Bring a list of any prescription or over-the-counter medications you are taking. Dont forget to list vitamins and supplements, too.
- Jot down a list of questions, such as:
- What tests or procedures will be performed?
- How will my asthma be monitored?
- How should I use my medications? How should they be stored?
- What triggers might cause my asthma to flare? Is there anything I can/should do to reduce my risk of having an asthma attack?
- Will I have an asthma action plan?
- How often do I need follow-up care?
Don’t Miss: Does Weight Gain Make Asthma Worse
How Is Asthma Prevented And Treated
There is no cure for asthma. Control symptoms by taking asthma medicines and avoiding your triggers. With proper treatment and an asthma management plan, you can reduce your symptoms and enjoy a better quality of life.
Talk to your health care provider about your asthma symptoms and be sure to discuss any changes in your asthma management or status.
What Are The Signs And Symptoms Of Asthma
Asthma is a lung condition that causes shortness of breath and difficulty breathing. It can be triggered by several things, including airborne allergens and physical exertion. Signs and symptoms of asthma include the following:
- Coughing
- Low tolerance for physical exercise
- Wheezing
Many of these symptoms can be caused by other ailments , but you should consider being tested by a doctor regardless. Allergies often act as asthma triggers, making it a dual problem.
Recommended Reading: Military With Asthma
Also Check: Does Weather Affect Asthma
Your Eosinophilic Test Results: What To Expect Next
If youre diagnosed with eosinophilic asthma, your doctor might prescribe one of three treatments designed to target eosinophils, says Chupp. These medications, called biologics, can help lower the levels of eosinophils and resulting inflammation in the lungs, which can reduce asthma attacks. Given as injections or infusions you receive every few weeks at your doctors office, these therapies work by targeting specific molecules involved in the action of eosinophils. Mepolizumab and reslizumab are antibodies against interleukin 5 molecules, while benralizumab is an antibody against the IL-5-receptor-alpha-chain. Studies suggest that these drugs are safe and effective in most people with eosinophilic asthma, says Chupp.
If you have severe or hard-to-treat asthma, talk to your doctor about whether you should be tested for eosinophilia. If you do have eosinophilic asthma, it can affect the type of treatment youll need.
Role Of Eosinophil In Pathogenesis
Eosinophils are granulocytes in blood produced in the bone marrow with other white blood cells making about 13% of white blood cells. Eosinophil plays multiple functions and is an important component of allergic and asthmatic type 2 immune responses. Allergens on exposure starts a group of processes by Th2 cytokine-producing cells, resulting in eosinophils attraction to the airway through the action of IL-5, and eotaxin research reported that Clara cells of the airway epithelium are the main source of eotaxin in the lung .
During asthma attack, eosinophils are stimulated to release proteins from granules including major basic protein, eosinophil peroxidase, eosinophil cationic protein, and eosinophil-derived neurotoxin, all of which are toxic to the epithelial cells of airway. Furthermore, eosinophils secrete plenty of inflammatory mediators like cytokines , platelet-activating factor, growth factors , leukotrienes, thromboxane, and prostaglandins. The secretion of all these mediators results in enhancement of the inflammatory process, airways epithelium cell injury, airway hyperresponsiveness, mucus hypersecretion, and airway remodeling and bronchospasm . Eosinophils control the allergen-dependent Th2 pulmonary immune responses activated by dendritic cells and T cells as well as decrease Th1 responses .
Recommended Reading: Relieving Asthma Without Inhaler
What Is The Outlook For Eosinophilia
Treating the cause of high eosinophil counts affects the outcome. In more serious conditions, outcomes also depend on the extent of target organ and how the person responds to treatment.
Last reviewed by a Cleveland Clinic medical professional on 02/15/2018.
References
- Fulkerson PC, Rothenberg ME. Targeting Eosinophils in Allergy, Inflammation and Beyond. Nature reviews Drug discovery. 2013 12:10.1038/nrd3838. doi:10.1038/nrd3838.
- Common Laboratory Tests. In: LeBlond RF, Brown DD, Suneja M, Szot JF. LeBlond R.F., Brown D.D., Suneja M, Szot J.F. Eds. Richard F. LeBlond, et al.eds. DeGowinâs Diagnostic Examination, 10e New York, NY: McGraw-Hill 2014.
- Merck Manual Professional Version. Accessed 3/2/2018.Eosinophilia.
- American Partnership for Eosinophilic Disorders. Accessed 3/2/2018.What is an eosinophil-associated disease?
- Hsieh, Fred H Eosinophilia and the Hypereosinophilic Syndrome. In: _eLS. John Wiley & Sons, Ltd: _Chichester. doi: 10.1002/9780470015902.a0002155.pub2
- Kovalszki A, Weller PF. Eosinophilia. Primary care. 2016 43:607-617. doi:10.1016/j.pop.2016.07.010.
- Rothenberg ME. Eosinophilia. N Engl J Med. 1998 338:1592-600.
- Butt, N. M., Lambert, J., Ali, S., Beer, P. A., Cross, N. C. P., Duncombe, A., Ewing, J., Harrison, C. N., Knapper, S., McLornan, D., Mead, A. J., Radia, D., Bain, B. J. and the British Committee for Standards in Haematology , Guideline for the investigation and management of eosinophilia. Br J Haematol, 176: 553â572. doi:10.1111/bjh.14488
Will This Diagnosis Change How My Asthma Is Treated
Maybe. Some patients with eosinophilic asthma respond to the traditional methods of treating it, using inhaled corticosteroids to reduce inflammation and bronchodilators like as a quick-acting rescue medication. However, since eosinophilic asthma affects the entire respiratory tract, inhaled steroids are often not enough, and many patients require systemic oral steroids to see symptom improvement.
New treatments are also being developed to reduce the number of eosinophils in the airway. These may be a good option for you if your symptoms dont respond to steroids.
-
Anti-interleukin-5 therapy- Interleukin-5 is a protein that activates eosinophils. Biologic therapies, such as mepolizumab and reslizumab , block IL-5. They are both used in conjunction with other asthma medications.
-
Anti-immunoglobulin E therapy- Immunoglobulin E is an antibody that plays a role in . Therapies, like omalizumab , that block IgE decrease both inflammation and the number of eosinophils in the airway. However, this treatment will only be effective for cases of eosinophilic asthma that are triggered by allergens.
-
Clinical trials- Researchers are studying other treatments that target interleukins, such as anti-IL-4 and anti-IL-13. Early results look favorable for these new therapies.
Don’t Miss: What Is Type 1 Asthma
