Are Bronchodilators Safe To Use During Pregnancy Or While Breastfeeding
Beta-adrenergic bronchodilators
- Beta-adrenergic bronchodilators are used for treating children. However, there are no adequate studies of beta-adrenergic bronchodilator use during . Some reports indicate that albuterol sulfate may cause congenital defects when used during pregnancy.
- It’s not known whether beta-adrenergic bronchodilators are excreted in breast milk.
Anticholinergics
- The safety of anticholinergic bronchodilators in women or nursing mothers has not been adequately evaluated.
Xanthine bronchodilators
- Xanthine bronchodilators have not been adequately studied in pregnant women. Theophylline is excreted in breast milk and may cause mild side effects such as irritability in the infant.
- The risks to the fetus or breast-feeding infant versus the risk to the woman should be considered before using bronchodilators in pregnant women; consultation with the patients OB/GYN doctor may be advisable.
When And How Are Types Of Asthma Diagnosed
Asthma is d based on symptoms, a physical examination, and lung function tests.1 Your health care provider will ask about the type and frequency of your asthma symptom and attacks. Tell your provider if you have had eczema, food allergies, hay fever , long-term nasal congestion , heartburn, or reflux in the past.
Inhaled corticosteroids are usually used to treat people with asthma. For some people, these medications do not work well. The first thing to do is to make sure you are taking them . If you still have symptoms, more tests may be needed to know which type of asthma you have.4 The results can help your provider recommend another treatment.
There Are Many Different Types Of Asthma Brought On By Many Different Triggers
If youre struggling with asthma symptoms trouble breathing, a persistent cough or tightness in the chest an allergist can help you take control by providing a diagnosis and identifying the underlying causes.
Learn about the triggers and treatment for allergic asthma and how an allergist can help you manage allergy and asthma symptoms.
What Are The Uses For Bronchodilators
The bronchodilators listed in this article are used for managing bronchospasm due to asthma, reactive airway disease, and exercise-induced asthma.
- Short-acting beta-adrenergic bronchodilators and ipratropium work quickly and are used for acute management of asthma episodes.
- Long-acting beta-adrenergic bronchodilators, tiotropium, and theophylline are used daily and long-term for preventing asthma attacks or reducing the frequency of symptoms.
Severe Asthma Typically Requires A Combination Approach To Treatment
If someone experiences asthma symptoms more than twice a week, their asthma is termed persistent. And among those with persistent asthma, doctors further categorize the condition as mild, intermediate, or severe.
The symptoms of severe asthma are similar to those of mild asthma, theyre just more frequent and more severe, and require more medications to keep them under control, says Emily Pennington, MD, a pulmonologist and asthma specialist at the Cleveland Clinic in Ohio.
Often, if someones symptoms require a combination of asthma medications such as high-dose inhaled corticosteroids as well as longer-acting drugs that persons asthma is termed severe. The same term applies to people who dont respond well to treatment.
We dont entirely understand why some people dont respond as well to medication, Dr. Pennington says. Genetic and underlying molecular factors are likely explanations, she says, but the exact causes of severe asthma are complex and likely vary from one person to the next.
Theres also an informal term, uncontrolled asthma, that refers to people whose asthma symptoms are not well managed. This can happen for a number of reasons:
- Other conditions, such as heart disease, that make asthma hard to manage
- Lifestyle choices, such as the decision to smoke cigarettes, that exacerbate asthma symptoms
- Not following a doctors advice or guidelines when taking medications
About Author
BETTER HEALTH & BEYOND Editorial Team
Learn more at:
Join us on
How Long Asthma Lasts For
Asthma is a long-term condition for many people, particularly if it first develops when you’re an adult.
In children, it sometimes goes away or improves during the teenage years, but can come back later in life.
The symptoms can usually be controlled with treatment. Most people will have normal, active lives, although some people with more severe asthma may have ongoing problems.
What Happens When Allergens Set Off The Immune System
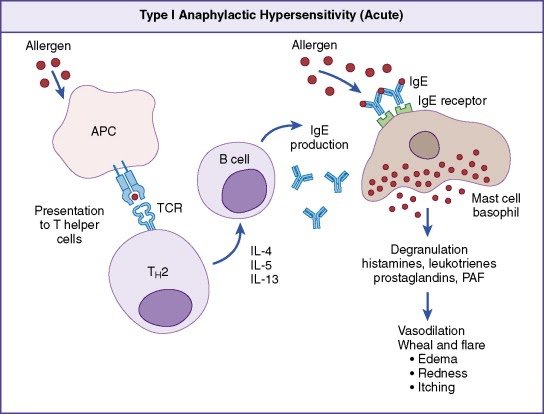
In order to understand your lab results and medications, it is helpful to know what happens during an allergic reaction.
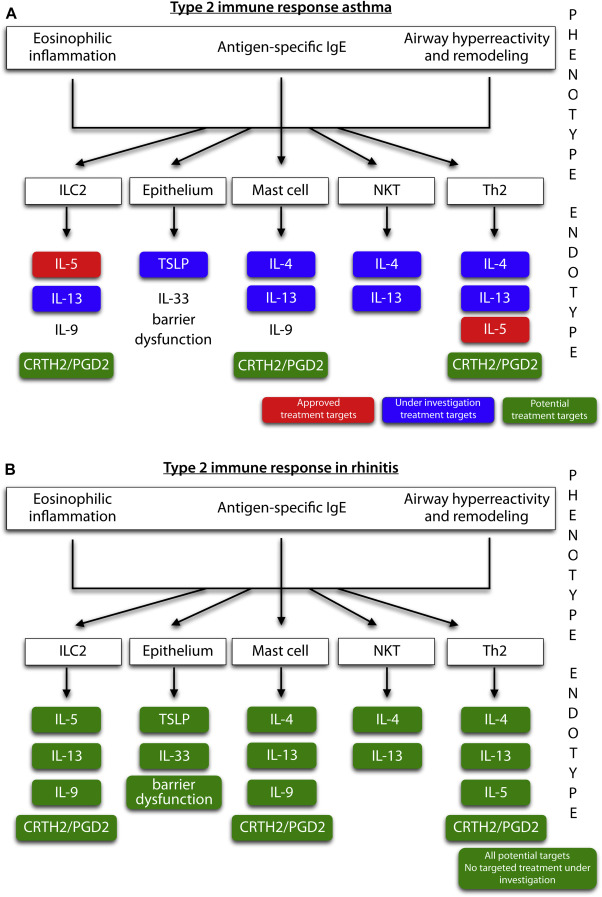
When an allergen triggers the immune system, many different kinds of cells and signaling chemicals get involved. The allergen enters the airway and turns on mast cells and dendritic cells.4 These cells tell type 2 helper cells to send out signaling chemicals called interleukins. There are different kinds of interleukins . Some examples are IL-4, IL-5, or IL-13.
Each interleukin has a different role in allergic asthma:
- IL-4 and IL-13 are signals to make an antibody called IgE . IgE is responsible for many allergy symptoms, such as wheezing, coughing, swelling, itching, and runny nose.5,6
- IL-13 has a role in airway narrowing.4
- IL-5 and IL-13 increase the number of the . Eosinophils are a type of white blood cell. People with asthma often have high levels of eosinophils.
Constant exposure to an allergen leads to ongoing inflammation.2 Ongoing inflammation may cause structural changes in the airways. Overtime, the airways may become more sensitive to allergens and irritants. They may not open as wide, even after treatment with medication.
Development And Pathophysiology Of Asthma
Asthma is characterized by airway hyper-responsiveness, chronic inflammation, mucus production, and structural airway remodeling that is largely allergic in nature. It is a complex syndrome and not a singular disease. Clinical and scientific evidence indicates that multiple sub-types of asthma exist in adulthood, though this is less true in early childhood. Asthma usually develops at a young age, and it remains difficult to diagnose before age 3. Upper respiratory viral illnesses, particularly rhinovirus and respiratory syncytial virus, and environmental allergens combine to trigger an upper and lower airway inflammatory response in susceptible individuals. Several theories try to describe this phenomenon, such as the atopic march that states that allergic inflammation of the airways naturally follows eczema or atopic dermatitis in young children. The hygiene hypothesis suggests that allergic inflammation results from changes in the patterns of exposure less infections, more contact with indoor allergens like house dust mite that children experience at a very young age.
Ilkay Zihni Chirali MBAcC RCHM, in, 2014
Long Acting Inhaled 2agonists
In view of the marked fluctuations in PEF and the efficacy of subcutaneous 2 agonist infusions, it might be expected that long acting inhaled 2 agonists would be effective in stabilising the airways. However, in our experience salmeterol has proved to be disappointing in these patients for reasons that are not yet clear. Whether formoterol, which is a full agonist, may be more useful than salmeterol, a partial agonist, remains to be determined. There is an anecdotal report of a patient showing symptomatic and lung function improvement with formoterol, but not to salmeterol.
Type I And Iii Interferon Responses In The Lung
While type I IFNs have been known since 1957 as cell-secreted antiviral factors , and were the first cytokines discovered, type III IFNs were only first described in 2003. Their simultaneous discovery by two different groups led to their many names, with Paul Sheppards group calling them interleukins -29 and IL-28A/B , while Sergei Kotenkos group referred to them as IFN lambda . While IFN1 is only found in humans, both mice and humans express IFN2 and IFN3. Though structurally dissimilar, type I and III IFNs converge at the beginning of their signal cascades to induce the transcription of a highly overlapping complement of interferon-stimulated genes . However, the localization of the type III interferon-specific receptor IFNR1 to mucosal tissues and immune cells restricts its actions . Type I and III IFNs also differ in their kinetics and ability to activate STAT1, leading to differences in IFN response factor expression and subsequent induction of pro-inflammatory chemokines . Moreover, more recent work shows that these differences may be independent of receptor abundance and instead intrinsic to their signaling pathways . While new research will continue to reveal differences between type I and III IFN signaling, these pathways have many redundancies and are highly overlapping throughout the respiratory tract .
Mechanisms Underlying Paucigranulocytic Asthma
Paucigranulocytic asthma encompasses patients with absence of airway inflammation with persistent symptoms and evidence of AHR. Underlying mechanisms for this endotype may be due to changes in ASM or airway inflammation not reflected in the lumen or detected by sputum cytometry.
Although PGA is typically regarded as absence of both eosinophilic and neutrophilic inflammation, Demarche et al demonstrated evidence of inflammation, where PGA had higher sputum eosinophil counts, blood leukocytes and blood eosinophils than healthy subjects. Further, mast cell infiltration in ASM has been postulated to play a role in the pathogenesis of this asthma phenotype, where secretion of mast cell mediators could lead to bronchial obstruction, airway remodeling and AHR. Mast cells may migrate toward Th2-stimulated smooth muscle bundles in asthmatic patients and may get activated by a number of factors including IL-33 that directly promotes mast cell activation and indirectly promotes ASM contraction via upregulation of mast cell-derived IL-13.
Who Is More Likely To Have This Type
The largest number of people with asthma have mild asthma. Mild intermittent and mild persistent are the most common types of asthma. Mild asthma is more likely than other types to be untreated since the symptoms are so mild.
A number of factors increase your risk for any type of asthma. These include:
- having a family history of asthma
- smoking or exposure to secondhand smoke
- having allergies
- development of mucus in the airways
- chest tightness or pain
T1d Versus Allergic Asthma
Epidemiological studies have shown positive associations between the occurrence of T1D and asthma suggesting a common etiology,, as well as inverse relationships between the two diseases suggesting distinction in disease etiology with Th1- or Th2-dominated immune responses, , as a plausible explanation. A possible reason for the discrepancies may be the existence of common genetic dispositions in the immune system occurring before CD4 differentiation, thereby influencing both T1D and allergic asthma development, as well as different or opposite genetic effects operating later in the immune-mediated cascade directly affecting Th1Th2 differentiation. As such, the joint association between the TLR2 and T1D and allergic asthma may represent a common susceptibility pathway before CD4 differentiation, or a pathway involving the regulatory T cells. This is of interest in light of the fact that for both diseases, the prevalence is increasing,, warranting studies exploring possible common factors influencing disease susceptibility.
In conclusion, the present study demonstrates a common association between a TLR2 polymorphisms and T1D and allergic asthma. This suggests that TLR2 is a susceptibility locus common for the two diseases. More studies are needed to elucidate how genetic variation in TLR2 might affect the pathogenesis of these diseases.
What Causes Allergic Asthma
Allergic asthma tends to run in families.1 This means that probably play a role in whether you have asthma and allergies.
The symptoms of asthma are wheezing, coughing, shortness of breath, and chest tightness.3 In a person with allergic asthma, these symptoms start after inhaling an allergen. Allergens are substances that are usually harmless, such as pet dander, pollen, and dust mites. In people with allergies, these allergens set off the immune system.
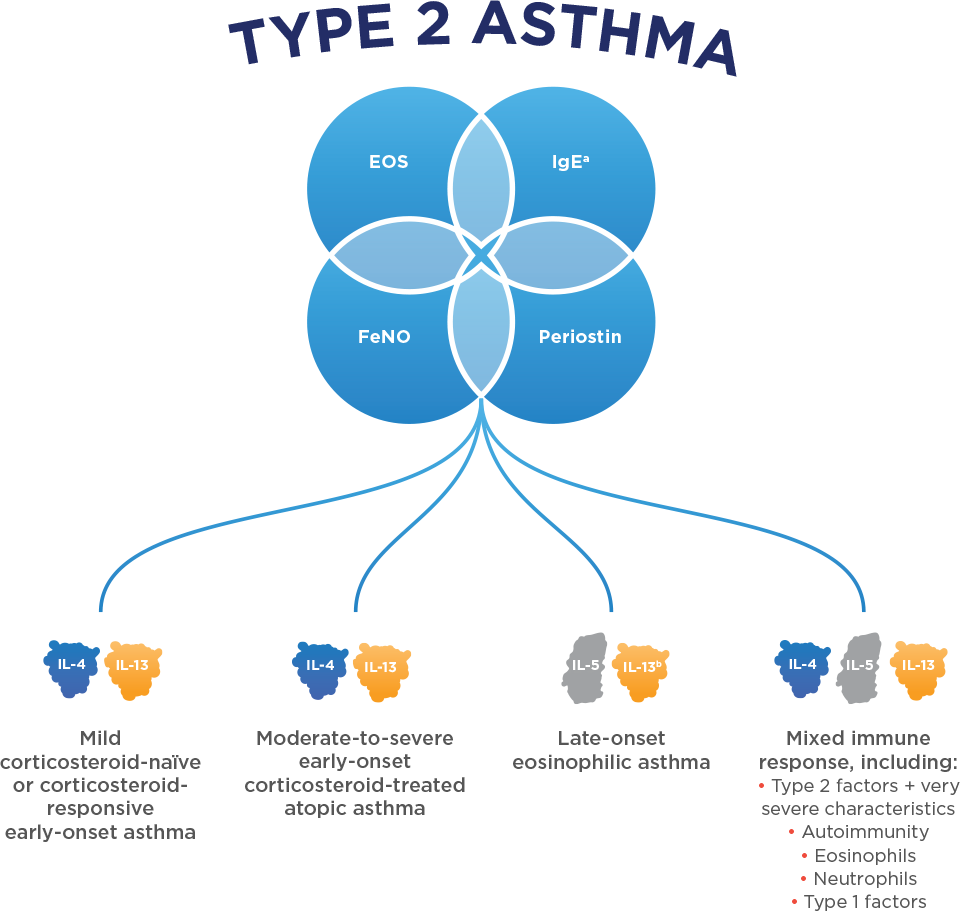
What Is Type 2 Inflammation In Asthma
As many as 50-70 percent of asthma patients have a form of asthma characterized by Type 2 inflammation. Type 2 inflammation is a type of systemic allergic response that can result in increased asthma exacerbations and decreased lung function.
Cytokines, which are proteins that signal the bodys cells and begin an immune response, are major contributors to Type 2 inflammation.
Common asthma biomarkers are also present in Type 2 inflammation. These include:
- eosinophils
- Immunoglobulin E
- fractional exhaled nitric oxide
When there are too many eosinophils in the blood, there is an increased risk of severe asthma flares. Learn more about eosinophilic asthma at .
Genetics also appear to play a role in Type 2. Studies show that if one or both parents have Type 2 inflammation related to asthma, their child is four times more likely to have asthma or an allergic disease.
Identifying Type 2 Asthma In Clinical Practice
Professor G. Walter Canonica
Approximately 5070% of asthma patients have Type 2 asthma,37,38 which is characterised by Type 2 inflammation. This group typically includes allergic asthma, exercise-induced asthma, and late-onset eosinophilic asthma. By contrast, non-Type 2 asthma commonly has an older age of onset, is associated with obesity and smoking, and is neutrophilic, smooth muscle-mediated, and paucigranulocytic.31
An understanding of the mechanisms of asthma is important to achieve better disease control. In the clinic, patients are evaluated according to measures of control , quantifiable biomarkers , and patient characteristics . Recently, the need to check for nasal polyps and allergic rhinitis was recognised; an Italian registry39 found that 60% of severe asthma patients had a diagnosis of allergic rhinitis. The registry also found that 62% of patients have taken OCS, and that eosinophil counts were higher than desirable, Prof Canonica said.
When asked whether they use IgE measurements to manage this patient group, Prof Canonica was encouraged that >40% of audience members always relied on IgE measurements; however, 17% said they used it only 25% of the time. On the routine use of eosinophil measurements, around one-third of the audience said they used it either 25% or 50% of the time in this patient group.
Why Would An Association Go In Only One Direction
Children with asthma were more likely to have co-occurring type 1 diabetes, but the reverse was not true, according to a Swedish registry study.
Among more than one million children, those with asthma had a small but significant increased risk of being subsequently diagnosed with type 1 diabetes compared with children who did not have asthma , reported Awad Smew, MD, of the Karolinska Institutet in Stockholm, Sweden, and colleagues.
However, children with type 1 diabetes versus those without did not have a greater risk of going on to develop asthma , the team wrote in JAMA Network Open.
“Our findings could partially be explained by the fact that asthma in our sample occurred at a younger mean age than type 1 diabetes, meaning that children with both asthma and type 1 diabetes in general already had received their asthma diagnosis before they developed type 1 diabetes,” Smew and co-authors wrote.
Prior research has suggested a link between asthma and type 1 diabetes, but this idea was challenged by a 2003 meta-analysis that found a of asthma among kids with type 1 diabetes.
It may seem plausible that some factors, like early exposure to viruses, would play a role in the development of these two diseases, commented Michael Yafi, MD, of the McGovern Medical School at UTHealth in Houston, who was not involved with this research.
-
Elizabeth Hlavinka covers clinical news, features, and investigative pieces for MedPage Today. She also produces episodes for the Anamnesis podcast.
Phenotypic Variability In Asthma
To complete the topic asthmatic allergic response, the phenotypic heterogeneity has to be taken into consideration. Indeed, apart from allergic asthma, which is the most common form, other types of asthma have been described.9,34 However, as with allergic asthma, the scientific community recognizes that IgE could be implicated in an inflammatory cascade, as well as CD4+ and CD8+ T cells, eosinophils, and mast cells. A second type of asthma is characterized by sensitivity to aspirin. It is estimated that approximately 1020% of adult asthmatics suffer from this particular type.35 Aspirin sensitization is thought to be non-IgE mediated so could be considered as a nonallergic subphenotype of asthma. A dysfunction of the eicosanoid metabolism is responsible for this type of asthma. It is estimated that 915% of all cases of asthma in adults are linked to the workplace and that up to 25% of new cases of adult asthma fall in the occupational asthma category. The two major hypotheses that could explain the induction of asthma after an effort are related to the augmentation of ventilation in the lungs. These two hypotheses are the osmotic hypothesis and the thermal hypothesis .36 These two hypotheses could better explain the phenotype rather than each one separately.
G.U. Schuster, … C.B. Stephensen, in, 2013
What Is Eosinophilic Asthma
Eosinophilic asthma is a subtype of asthma that is often severe. It is commonly seen in people who develop asthma in adulthood, although it may occur in children and young adults.
Asthma is a chronic lung disease in which diseased airways are infiltrated by inflammatory cells and obstructed by fluid and mucous. This causes spasms in the bronchial tubes, making breathing difficult. Asthma may result from allergy or other hypersensitivities; however, many patients who have eosinophilic asthma do not have a history of allergic conditions .
In eosinophilic asthma, the numbers of eosinophils are increased in blood, lung tissue, and mucus coughed up from the respiratory tract . The whole respiratory tract is involved in airflow obstruction from the sinuses to the small or distal airways. Patients with eosinophilic asthma frequently suffer from chronic sinus disease and nasal polyposis.
Research has shown that an elevated number of eosinophils in the blood correlates with future risk and severity of asthma attacks.
Asthma can range in severity and treatment may vary from patient to patient. To help outline the best course of treatment for an asthmatic patient, it is important for a health care provider to determine which subtype of asthma a person might have, because there are now new therapies that target specific subgroups of asthma, like eosinophilic asthma.
Causes And Triggers Of Asthma
Asthma is caused by swelling of the breathing tubes that carry air in and out of the lungs. This makes the tubes highly sensitive, so they temporarily narrow.
It may happen randomly or after exposure to a trigger.
Common asthma triggers include:
- allergies
- smoke, pollution and cold air
- exercise
- infections like colds or flu
Identifying and avoiding your asthma triggers can help you keep your symptoms under control.
What Are The Risk Factors For Brittle Asthma
The causes of severe asthma are not known, but some risk factors have been identified. Many of the risk factors for brittle asthma are the same as those for less severe types of asthma. These include the state of your lung function, how long youve had asthma, and the severity of your allergies.
Being a woman between the ages of 15 and 55 increases your risk for type 1 brittle asthma. Type 2 brittle asthma is seen equally in men and women.
Additional risk factors for brittle asthma include:
- being obese, which is accompanied by sleep apnea
- specific gene mutations, including genetically determined resistance to certain asthma drugs
- environmental exposure to allergens, such as dust mites, cockroaches, mold, cat dander, and horses
- food allergies, including allergies to dairy products, wheat, fish, citrus, egg, potato, soy, peanuts, yeast, and chocolate
- cigarette smoking
- structural changes in airways
- psychosocial factors, including depression
Age can also be a risk factor. In one of 80 people with severe asthma, which includes brittle asthma, researchers found that:
- nearly two-thirds of participants developed asthma before age 12
- one-third developed asthma after age 12
- 98 percent of early-onset participants had positive allergy reactions
- only 76 percent of late-onset participants had positive allergy reactions
- people with early-onset asthma more commonly had a family history of eczema and asthma
- African-Americans are at increased risk for early asthma
How Is It Treated
At this asthma level your doctor may prescribe a low-dose inhaled corticosteroid medication. An inhaled corticosteroid is taken by quickly inhaling it. Its usually taken daily. Your doctor may also prescribe a rescue inhaler to have in case your symptoms still occur from time to time. Your doctor may also prescribe allergy medications if your asthma is triggered by allergies.
For those over the age of 5, a round of oral corticosteroids may also be considered.
Viral Exposure In Children
Evidence suggests that rhinovirus illness during infancy is a significant risk factor for the development of wheezing in preschool children and a frequent trigger of wheezing illnesses in children with asthma. Human rhinovirus C is a newly identified genotype of HRV found in patients with respiratory tract infections. A study of children with acute asthma who presented to the emergency department found HRVC present in the majority of patients. The presence of HRVC was also associated with more severe asthma.
Approximately 80-85% of childhood asthma episodes are associated with prior viral exposure. Prior childhood pneumonia due to infection by respiratory syncytial virus, Mycoplasma pneumoniae, and/or Chlamydia species was found in more than 50% of a small sample of children aged 7-9 years who later had asthma. Treatment with antibiotics appropriate for these organisms improves the clinical signs and symptoms of asthma.
Signs Symptoms And Complications
How often signs and symptoms of asthma occur may depend on how severe, or intense, the asthma is and whether you are exposed to allergens. Some people have symptoms every day, while others have symptoms only a few days of the year. For some people, asthma may cause discomfort but does not interfere with daily activities. If you have more severe asthma, however, your asthma may limit what you are able to do.
When asthma is well controlled, a person shows few symptoms. When symptoms worsen, a person can have what is called an asthma attack, or an exacerbation. Over time, uncontrolled asthma can damage the airways in the lungs.
When Asthma Is Not Just Asthma: Type 2 Inflammation
, , Severe Asthma News & Updates
Asthma was once considered a single, though complex, disease. Now its recognized as a spectrum of diseases. Genetic and environmental factors play a role in airway inflammation and hyper-reactivity. This leads to common asthma symptoms: coughing, wheezing and shortness of breath.
Severe asthma is one form of the disease. Its estimated that 5-10 percent of people with asthma have severe asthma.
Severe asthma is the diagnosis when
- symptoms are not well-controlled by high-dose inhaled controller medications
- the patient experiences two or more asthma flares in a 12-month span requiring oral corticosteroids
Recent medical breakthroughs involving severe asthma are transforming how its diagnosed and treated. Airway inflammation is a particular focus.
Asthma Management Strategies To Improve Maternal And Infant Outcomes In Pregnancy
Several studies indicate that the type of asthma management during pregnancy can impact asthma outcomes. A study of 211 pregnant women with asthma found that the provision of education on self-management skills, by a trained asthma educator, even once during pregnancy, improved self-management skills such as medication knowledge and adherence, lung function monitoring and possession of a written asthma action plan . Maternal and neonatal outcomes were not measured in this study, nor was this cohort compared with a group of pregnant women who did not receive asthma education; therefore, interpretation of the findings is difficult. Another study showed that repeat educational sessions were associated with reduced non-adherence and improved self-management skills in pregnant women . A more recent randomized controlled trial of 169 pregnant women with asthma showed that an asthma management service improved asthma control during pregnancy compared to usual antenatal care for persistent uncontrolled asthma . This antenatal asthma management service was led by a respiratory nurse and included asthma self-management education, an individualized asthma action plan, and evaluation of current asthma treatment . A significant difference in neonatal outcomes was not found between the groups, and larger RCTs would be required to determine the cost and clinical effectiveness of providing an ongoing nurse-led service.
Kamyar M. Hedayat, Jean-Claude Lapraz, in, 2019
Are There Differences Between Bronchodilators
Bronchodilators differ in their mechanism of action, how quickly they work, and their duration of action, their uses, side effects, and how they are administered. Beta-adrenergic bronchodilators are supplied as aerosols for , powders for inhalation, solution for nebulization, syrup, and tablets. Anticholinergic bronchodilators are supplied as solutions for inhalation, powder for inhalation, and nebulized solution. Xanthines are supplied as tablets, capsules, elixir, and solution for injection.
