Treatment Plan For Lung Scarring
Removing a scar directly isnt an option. Instead, your doctor will assess the scarring and determine whether any further steps are needed.
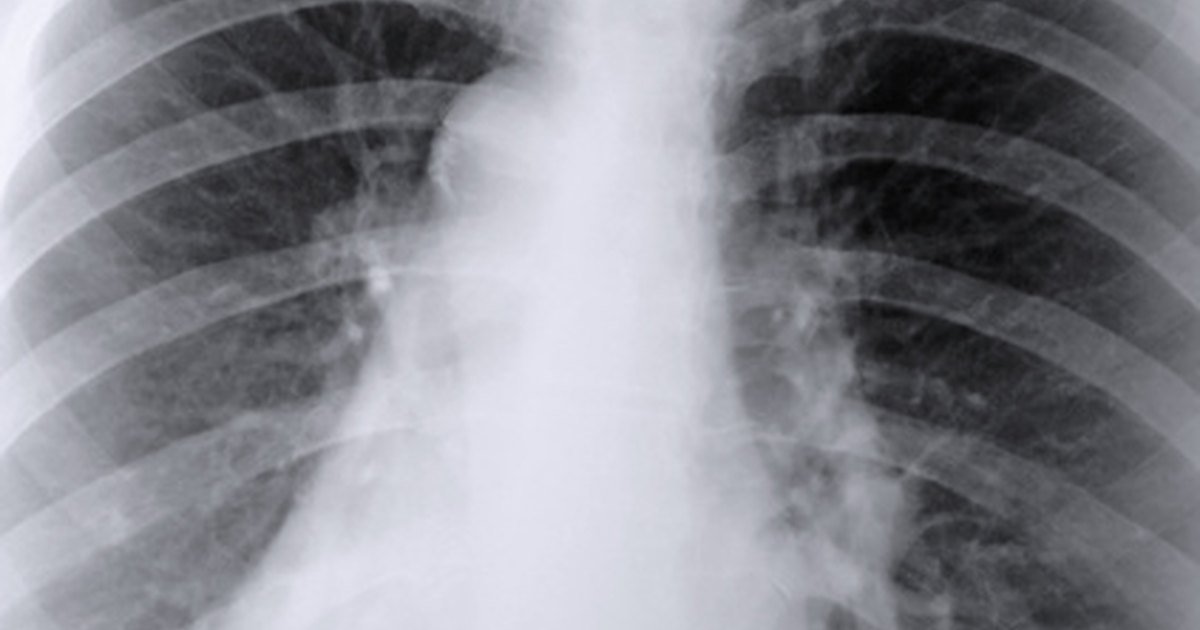
Your doctor will use X-ray images to assess the size and stability of the scarring. Theyll also check to see if the scar is expanding. To do this, theyll compare an older chest X-ray with a new one to see if the areas of scarring have grown. In many cases, you doctor may opt to use a CT scan in addition to X-rays.
If the scar is localized, meaning its only in one area, or has remained the same size over time, its typically harmless. Scars of this nature are generally caused by a previous infection. If the infection that caused this scar has been dealt with, further treatment isnt necessary.
If the scar is growing or is more widespread, this may indicate consistent exposure to things that can cause lung scarring like toxins or medications. Certain medical conditions can cause scarring, too. This can lead to a problem known as interstitial lung disease . ILD refers to a set of diseases that decrease the elasticity of the lungs.
Your doctor may also recommend additional testing, such as a lung biopsy, to gather more information or confirm the diagnosis of a disease. In these cases, your doctor will develop a treatment plan to manage the underlying condition and prevent further scarring.
- fingers or toes that widen and become round at the tip
- aching muscles and joints
- dry cough
What Is The Life Expectancy For People Who Have Pulmonary Fibrosis
Some people live only months after a pulmonary fibrosis diagnosis. Others live several years. Many factors affect your prognosis. Even your provider cant predict some of these factors.
If youve been diagnosed with pulmonary fibrosis, you can take steps to help your body stay in its best possible shape:
- Be proactive to avoid getting sick: Pay close attention to handwashing, and avoid direct contact with anyone you know is sick. Having pulmonary fibrosis means your body cant recover as easily from infections that other people may fight off with little effort.
- Keep up-to-date with vaccines: Lung scarring makes it harder for the body to fight against infections. Get vaccinated for pneumonia and influenza to minimize your risk.
- Practice healthy habits: Stay active and make smart food choices. Get plenty of rest, and quit smoking.
What Are The Symptoms Of Pulmonary Fibrosis
Pulmonary fibrosis doesnt affect everyone in the same way. Many common, easily treatable conditions can cause similar symptoms. Sometimes these symptoms are signs of the common cold or an upper respiratory infection.
Pulmonary fibrosis symptoms include:
- Breathing in short, shallow spurts.
- Dry cough that doesnt go away.
- Fatigue .
- Shortness of breath, especially during or soon after you exercise.
- Weight loss thats not on purpose or easily explained.
As the disease progresses, some people experience:
- Clubbing, fingertips or toes that look different, such as wider or more round.
- Cyanosis, bluish skin or gray or white skin around the mouth or eyes from too little oxygen in the blood.
Don’t Miss: Sickness Induced Asthma
Can You Outgrow Asthma
Some children with asthma stop having symptoms when they mature. By adolescence, 16% to 60% of children diagnosed with asthma seem to be in remission.
However, doctors don’t usually consider asthma “cured” since, even after years of living symptom-free, you could suffer an asthma attack at any time.
The wide range of remission statistics shows that studies have been inconsistent in their design, and more research is needed to fully understand how and why some children seem to “get over” asthma.
In some studies, children who were more likely to go into remission had asthma characterized as:
- Less atopic dermatitis
Male children are also more likely to go into remission.
If your childhood asthma appears to have gone away, it may still be a good idea to avoid triggers, especially allergy triggers, as they could cause symptoms to reappear.
Little to no research has followed adults who appear to have outgrown their childhood asthma, so there’s no clear picture of whether or not this reduces the risk of long-term health effects.
How To Reduce Your Risk Of Complications
In general, working with your doctor can help you find the appropriate treatment to control your asthma symptoms and reduce your risk for these complications. And once you find a treatment that works for you, its important to stick with it.
Most people with asthma know the importance of staying on prescribed treatment, Rosenstreich says. Because if they dont, they know theyll see an increase in their symptoms. But your doctor will remind you that symptoms are only the start. These complications are, in most cases, rare and totally avoidable simply by staying with your treatment.
If you have trouble controlling your symptoms despite following your treatment plan, you may have a more severe form of asthma. Let your doctor know about your struggles so he or she can help find a more appropriate treatment.
With additional reporting by Markham Heid.
Read Also: What Do You Do When You Have An Asthma Attack
When Should I Call My Provider
In some cases, pulmonary fibrosis gets a lot worse, all at once. You should call your provider if you suddenly feel a big difference in symptoms.
For example, call your provider if youre coughing a lot more than usual or have any other symptoms that seem new or alarming. See a provider right away if you experience any difficulty breathing that you cant control.
A note from Cleveland Clinic
If you have pulmonary fibrosis, you will likely see a pulmonologist long-term for regular follow-up visits. Your healthcare provider will work with you to preserve your lung function and maintain the highest possible quality of life. They will help find the right combination of medication, supportive care and clinical trials to treat the ways pulmonary fibrosis affects you. Connecting with a pulmonary fibrosis support group may provide firsthand insights and advice from people who have faced similar challenges.
Last reviewed by a Cleveland Clinic medical professional on 04/05/2021.
References
How Asthma Affects Your Airways
Asthma is a complicated disease, and doctors don’t completely understand its causes. But it has two main components: inflammation and muscle constriction.
Asthma affects the airways, the bronchial tubes that carry air into the lungs. In people with asthma, the lining of these airways becomes inflamed. No one is sure why this first develops. But certain allergy triggers or irritants begin to trigger this swelling.
If you take long-term control medicines — like inhaled corticosteroids — you can reduce this swelling and keep the airways healthy. But if your asthma goes untreated, problems develop. Over time, this constant inflammation can destroy the surface layer of the airways, says Hugh H. Windom, MD, associate clinical professor of immunology at the University of South Florida.
“The surface layer acts as a kind of filter,” Windom says. “But once it’s gone, all of the pollutants and allergens have direct access into the lungs.” So asthma can cause damage to the airways that, in turn, makes the asthma worse.
Asthma also affects the muscles that surround the airways. During an attack, these muscles tighten and further restrict the amount of air getting into the lungs.
Eventually, the constant inflammation and muscle constriction can have irreversible effects.
Also Check: Ketorolac Asthma
How Can The Chance Of Lung Damage From Covid
If you have chronic medical conditions, such as diabetes, COPD or heart disease, it is important to ensure that you are medically optimized. Take your medications as prescribed and monitor your blood sugar, blood pressure and fluid status, and make sure you are breathing appropriately.
For everyone, its important to maintain adequate nutrition, eat healthy and stay hydrated appropriately. Ensure that youre up to date on your vaccinations, get your flu shot and a pneumonia vaccine if you are in the appropriate age group. Although you may see reports of vitamins, minerals and prophylaxis medications to prevent/reduce the damage, we dont have studies that are supporting it at this time.
What Are The Physiological Changes In Lung Structure And Function That Causes Serious Complications What Causes These Changes Specifically
A major issue with COVID-19 is with gas exchange in the alveolus. Usually, there is a very tight connection between the alveolar epithelium and the capillary. COVID-19 infects AT2 cells, kills them and floods the alveolus. In addition, there is evidence for microthrombosis, which may block the vascular side.
Clinically, this may appear as several conditions: severe bronchopneumonia, acute respiratory distress syndrome or sepsis.
Pneumonia is inflammation and fluid in the lungs, making it difficult to breathe. Patients can experience shortness of breath, fevers and cough, which can be productive. More severe inflammation can lead to ARDS, which can require significant treatment including the use of oxygen therapies, including mechanical ventilation or even extracorporeal membrane oxygenation , which is a lung bypass machine that oxygenates the blood. If a patient develops this severe of a syndrome, this can lead to longer-lasting effects on the lungs, such as fibrosis .
Figure 3 CT chest showing multifocal ground glass opacities with intermixed consolidation from COVID-19 bronchopneumonia.
Figure 4 – CT chest showing multifocal ground glass opacities with intermixed consolidation from COVID-19 bronchopneumonia.
Figure 7 – CT chest showing multifocal ground glass opacities from COVID-19 bronchopneumonia.
Also Check: What To Do Asthma Attack No Inhaler
Are Pulmonary Fibrosis And Copd The Same
No, pulmonary fibrosis and chronic obstructive pulmonary disease are not the same. However, they are similar in some ways. Pulmonary fibrosis and COPD are both lung diseases that get worse over time. Both conditions can make breathing difficult.
But these conditions affect your lungs differently:
- Pulmonary fibrosis: Providers classify pulmonary fibrosis as an interstitial lung disease. The interstitial tissues are cells that make up the space between blood vessels and other structures inside the lungs. Pulmonary fibrosis damages these cells. It is a rare disease.
- COPD: COPD is a more common type of lung disease. Diseases like emphysema and chronic bronchitis are types of COPD. In COPD, lung tissue is damaged, alveoli are destroyed and airways can get irritated and inflamed .
What Should I Know About Egpa
- Almost all EGPA patients have asthma and/or sinus polyps, and a higher-than-normal level of eosinophils.
- Symptoms can range from mild to life-threatening, depending on which organs are involved and the extent of disease. Symptoms may include fever, fatigue, rapid and sudden weight loss, muscle and joint pain, skin rashes, numbness or tingling of the hands or feet, increasing shortness of breath or coughing and abdominal pain.
- EGPA is serious but treatable. Treatment typically includes oral corticosteroids used in combination with medications that suppress the immune system.
- In late 2017, a new medication was added to the treatment toolbox. FDA approved the use of the biologic drug mepolizumab for the treatment of EGPA in adults.
- Even with effective treatment, EGPA is a chronic illness with cycles of relapse and remission that can cause serious health problems, so ongoing medical care is necessary.
Don’t Miss: Asthma Help Without Inhaler
Causes Of Scarring Of The Lungs: Its Treatment And Prognosis
Scarring or fibrosis of the lungs is seen as thickening of the tissue around and in-between the air sacs in the lungs. As a result it becomes difficult for oxygen to pass in to the blood. Scarring may occur due to various factors prolonged exposure to toxins, some diseases and medical conditions, and radiation therapy.
It manifests as a chronic, dry, hacking cough, significant weight loss, rapid heart rate, exhaustion and curving of the fingernails. Symptoms seem negligible at first and then gradually progress with time. But they tend to vary from one individual to another.
How Is Pulmonary Fibrosis Treated

Most pulmonary fibrosis treatments focus on easing symptoms and improving your quality of life.
Your provider may recommend one or more treatments:
- Medication: Two medications pirfenidone and nintedanib may slow down lung scarring. These medications can help preserve lung function.
- Oxygen therapy: Giving your body extra oxygen helps you breathe more easily. It may also increase your energy and strength.
- Pulmonary rehabilitation: Staying active in this special exercise program may improve how much you can do everyday tasks or activities.
- Lung transplant: A lung transplant replaces one or both diseased lungs with a healthy lung from a donor. It offers the potential to improve your health and quality of life. A lung transplant is major surgery, and not everyone is a candidate. Ask your provider if you may be eligible for a lung transplant.
Recommended Reading: Army And Asthma
What Are The Symptoms Of Pulmonary Sarcoidosis
Most people with sarcoidosis do not have symptoms and probably don’t know they have the disease. It can affect many organs, causing a variety of symptoms. Pulmonary sarcoidosis can reduce the amount of air the lungs can hold and cause lung stiffness.
The following are the most common symptoms of pulmonary sarcoidosis. However, each person may experience symptoms differently. Symptoms may include:
- Shortness of breath, which often gets worse with activity
- Dry cough that will not go away
- Chest pain
Sarcoidosis can also cause symptoms not directly related to the lungs, such as:
- Extreme tiredness
- Pain in the joints and bones
- Skin rashes, lumps, and color changes on face, arms, or shins
- Swollen lymph nodes
- Weight loss
The symptoms of pulmonary sarcoidosis may look like other conditions or medical problems. Talk with your healthcare provider for a diagnosis.
What Should I Know About Pneumoconiosis
- Pneumoconiosis can take years to develop. Symptoms are similar to asthma and other respiratory diseases: shortness of breath coughing with phlegm and chest tightness.
- There is no cure for pneumoconiosis treatment focuses on managing the disease. Patients may be prescribed quick-relief and long-acting controller inhalers, as well as undergo oxygen therapy to improve lung function.
- Patients should work with doctors and employers to ensure the workplace has proper health and safety measures in place, including wearing protective clothing and masks. Lifestyle changes such as maintaining a healthy weight, quitting smoking and frequent handwashing may also help.
Also Check: What Is The Blood Test For Eosinophilic Asthma
For Those People Who Are Diagnosed With Covid
According to the World Health Organization, recovery time appears to be around two weeks for mild infection and three to six weeks for severe disease. However, this is variable and depends on a patients pre-existing comorbidities in addition to illness severity.
Several surveys conducted in the U.S. and Italy are showing that only 39% of those who had been hospitalized reported a return to baseline health by 14-21 days after diagnosis.
Similarly, in a study of 143 patients hospitalized for COVID-19, only 13% were symptom-free after a mean of 60 days following disease onset.
The most common symptoms were dyspnea , fatigue , joint pain and chest pain.
However, there have been reports of persistent severe illness with weeks of fevers and pneumonia persisting in immunosuppressed patients.
With milder infection, patients can still have prolonged symptoms. A recent survey showed that only 65% reported a return to baseline health by 14-21 days after diagnosis. Those who did return to baseline health did so a median of seven days after the diagnosis. Symptoms that can persist include cough , fatigue and rarely fevers and chills in those with prior mild infection.
What Is Sarcoidosis
Sarcoidosis occurs when groups of immune cells form lumps on various organs in the body, usually the lungs and lymph nodes in the chest. While no one knows what causes sarcoidosis, it is believed that inflammation and an overactive immune system may play a role.Sarcoidosis can cause breathing problems, reduced lung function and sometimes permanent lung damage . The disease can affect anyone, but people over 20 years of age and women are more likely to develop it. African-Americans are at higher risk for sarcoidosis than Caucasians and may experience more severe symptoms.
Also Check: Stopping Wheezing Without Inhaler
What Are The Long
In the long term, chronic inflammation and bronchospasms from asthma can make structural changes in the airway causing it to become permanently narrowed. The airway tubes become scarred and thickened, and the bronchial muscles get enlarged, leading to reduced lung function and breathing difficulties.
Asthma increases the risk for bronchial infections. Asthma can also affect sleep quality and lead to sleep deprivation. It can affect the ability to take part in exercise and sports, which can in turn, potentially lead to conditions such as diabetes, obesity and high blood pressure.
Severe asthma increases the risk for respiratory failure. Though rare, an acute asthma attack can diminish oxygen supply to the body, cause weakness and fatigue, and can sometimes even lead to death.
What Causes Scarring Of The Lungs
Autoimmune diseases: Cause the bodys immune mechanism to attack itself. Certain autoimmune disease can cause scarring of the lungs, these are:
- Rheumatoid arthritis
- Polymyositis
- Dermatomyositis
Chemical exposure: An exposure to chemicals can also contribute to pulmonary scarring. Chemicals found in cigarette smoke, asbestos fibers, silica dust, grain dust, some gases and radiation can produce scarring and impairment of the lungs.
Drugs: Some medications increase your risk of developing lung fibrosis.
- Heart medications such as amiodarone
- Chemotherapy drugs
- Antibiotics such as sulfasalazine
Idiopathic: sometimes, there may be no identifiable cause.
Genetics: 10 15 % of people having pulmonary fibrosis have a family member who has it too. Researchers say that certain genes are linked to the condition, however, more study about the role of genetics is necessary.
Recommended Reading: Does Weight Gain Make Asthma Worse
Lung Inflammation And Scarring
In severe cases, the lungs may become scarred. The scarring causes stiffness in the lungs, which can make it difficult to breathe and get oxygen to the bloodstream, resulting in long-term breathlessness and difficulty managing daily tasks.
This inflammation and scarring of the lungs is called interstitial lung disease.
Now, this study, called the UK Interstitial Lung Disease Long-COVID19 study, will investigate:
- whether post-COVID-19 lung damage will improve or worsen over time
- how long it will last
- the best strategies for developing treatments.
Early evidence indicates that lung damage occurs in approximately 20% of patients discharged from hospital, but the effects on people who experience Long-COVID in the community are currently unclear.
