Severe Asthma Is Asthma That Remains
Uncontrolled
- Frequent severe exacerbations / flare-ups / attacks
- Serious exacerbations
- Controlled asthma that worsens on tapering of corticosteroid treatment
Despite treatable factors having been addressed
- Treatment adherence
And maximal inhaled therapy being taken regularly
- High-dose inhaled corticosteroids AND
- Long-acting beta agonists or other controller
Having severe asthma symptoms does not necessarily mean that the person has severe asthma. To explain this, it is important to understand two key concepts in asthma management: asthma control and asthma severity.
Asthma Control
ASTHMA CONTROL
- symptom control, meaning how often the person has symptoms, night waking and limited activity due to asthma
- the persons risk of having adverse outcomes in the future, particularly asthma flare-ups, accelerated decline in lung function, or medication side-effects.
Well-controlled asthma means that asthma symptoms are infrequent , there is no night waking due to asthma, no limitation of normal activities, and the person is at a low risk of flare-ups.
Uncontrolled asthma, as well as burdening the patient with symptoms, can result in frequent flare-ups / attacks, adverse reactions to medication and chronic morbidity. In Australia, about 45% of adults with asthma have uncontrolled symptoms, and around one quarter have had a flare-up in the past year . Some patients have risk factors that increase their chance of flare-ups, even if they have few symptoms .
Inflammation And Adaptive Immunity
Potential immune-inflammatory and cellular interactions contributing to the pathogenesis of phenotypes of asthma. CXCL: CXC chemokine ligand CCL24/26: CC chemokine ligand 24/26 DUOX: dual oxidase EPO: eosinophil peroxidase IFN: interferon- IgE: immunoglobulin E IL: interleukin iNOS: inducible nitric oxide synthase MUC5AC: mucin 5AC NO: nitric oxide OX40/L: CD134 ligand PGD2: prostaglandin D2 Tc1: cytotoxic T-cell type 1 TGF: transforming growth factor- Th1: T-helper cell type 1 Th2: T-helper cell type 2 TSLP: thymic stromal lymphopoietin.
The mechanisms for airway neutrophilia are less clear. Corticosteroids themselves can contribute to the neutrophilia to some degree and even Th1 factors may play a role . Th17 immunity has been implicated as a cause for neutrophilia, primarily in murine models of asthma, with some supporting data from severe asthma .
The underlying mechanisms for severe asthma in those patients with little or no inflammation remain poorly understood, but could involve activation of resident cellular elements including smooth muscle cells, fibroblasts and neurons. Importantly, while emphasis has been placed on assessing inflammation by analysis of sputum samples, its relationship to cellular profiles in airway/lung tissues is poor and remains poorly understood .
Respiratory infections
Activation of innate immune pathways
Structural abnormalities
Recommended Reading: Help Asthma Without Inhaler
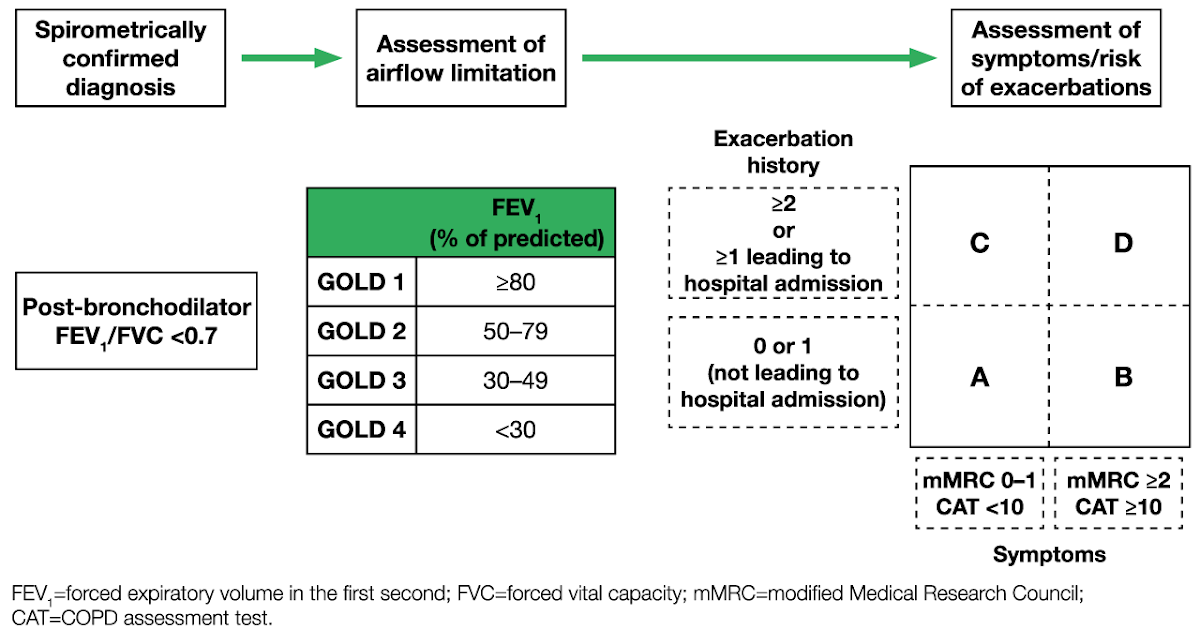
Airflow Limitation In Copd
The chronic airflow limitation of COPD is caused by a mixture of small airway disease and parenchymal destruction , the relative contributions of which vary from person to person . Chronic inflammation causes structural changes and narrowing of small airways. Destruction of the lung parenchyma, also by inflammatory processes, leads to the loss of alveolar attachments to the small airways and decreases lung elastic recoil in turn these changes diminish the ability of the airways to remain open during expiration .
So in COPD inflammation causes small airway disease and parenchymal destruction that all lead to airflow limitation .
You May Like: Albuterol And Weight Loss
Staging And Treatment Of Asthma
The goals of long-term management of asthma should include the following: 1) achievement and maintenance of control of symptoms 2) prevention of asthma exacerbations 3) maintenance of pulmonary function as close to normal levels as possible 4) maintenance of normal activity levels, including exercise 5) avoidance of adverse effects from asthma medications 6) prevention of the development of irreversible airflow limitation and 7) prevention of asthma mortality.
The recommended GINA treatment algorithm, together with the clinical features and staging of severity of asthma, are available on the GINA website . It is important to note that the forced expiratory volume in one second levels are before treatment, i.e. in the unmedicated state.
Until the advent of anti-inflammatory drugs, asthma was treated on an as-needed basis and treated as an acute disease rather than a chronic disease. With the recognition that asthma is a chronic inflammatory disease, there has been a gradual move towards treating it more aggressively and earlier in the hope that this may change the natural history of asthma and prevent some of the remodelling that sometimes occurs.
Canadian Chronic Disease Surveillance System
The CCDSS is a collaborative network of provincial and territorial chronic disease surveillance systems, led by the Public Health Agency of Canada . The CCDSS identifies chronic disease cases from provincial and territorial administrative health databases, including physician billing claims and hospital discharge abstract records, linked to provincial and territorial health insurance registry records using a unique personal identifier. Data on all residents eligible for provincial or territorial health insurance are captured in the health insurance registries thus, the CCDSS coverage is near-universal with the exception of some small populations. Case definitions are applied to these linked databases and data are then aggregated at the provincial and territorial level before being submitted to PHAC for reporting at the provincial, territorial and national levels.
The CCDSS has expanded from its initial mandate of diabetes surveillance to include data on several additional chronic diseases and conditions including: hypertension, mental illness, mood and/or anxiety disorders, heart failure, ischemic heart disease, acute myocardial infarction, stroke, osteoporosis, arthritis and neurological conditions. Asthma and COPD were added to the CCDSS in 2012.
The data presented in this report and subsequent updates can be accessed on the Public Health Agency of Canada’s Public Health Infobase.
Don’t Miss: What Happens If You Smoke Weed With Asthma
What Is The Overlap Between Asthma And Copd
A patient who has features of more than one condition exhibits an overlap syndrome. The pathogenesis of overlapping asthma and COPD may be mediated by inflammatory/immune mechanisms and/or structural alterations. The clinical recognition of overlapping asthma and COPD requires an assessment of increased variability of airflow and incompletely reversible airflow obstruction. Numerous studies have documented the presence of partial reversibility after short-term and long-term bronchodilator administration in patients with COPD., Current guidelines emphasize a fixed or irreversible component to airway obstruction in some patients with asthma., Thus, the use of phenotypic characteristics may be useful in differentiating disease characteristics and in understanding similarities in the development and progression of both obstructive airway diseases. A recent study found that 17% to 19% of patients with obstructive airway diseases had more than one condition, or overlap. The overlap of asthma and COPD has been confirmed in older patients by objective testing and is becoming an important clinical consideration.
Are Asthma And Copd Disabilities
According to the Asthma and Allergy Foundation of America , the American Disabilities Act and Section 504 state that having a mental or physical impairment that severely limits one or more life activities, including breathing, can be considered a disability.
For people with asthma, this applies even if symptoms only show at certain times, and if the person uses medication, such as an inhaler, to control the problem.
To qualify for social security disability benefits with COPD, a person must have:
- A forced expiratory volume one that is the minimum for your height or less, from 1.05 to a person who is 5 feet tall to 1.65 to someone who is 6 feet tall.
- Chronic impairment of gas exchange resulting from a documented COPD.
Those who do not meet these requirements may be able to get other types of help, such as as medical-vocational allowance for people on a low income.
Also Check: What’s An Asthma Attack Feel Like
What Is The Number One Inhaler For Copd
Advair. Advair is one of the most commonly used inhalers for the maintenance treatment of COPD. It is a combination of fluticasone, a corticosteroid, and salmeterol, a long-acting bronchodilator. Advair is used on a regular basis for the maintenance treatment of COPD and it is typically taken twice per day.
Airflow Restriction: Reversible Or Permanent
- Asthma treatment generally returns lung function to normal or near-normal and you should not have many asthma symptoms between asthma exacerbations. Airflow restriction in asthma is generally considered reversible, though some people who have severe asthma develop irreversible damage.
- Even with COPD treatment, airflow restriction and lung function will likely not return to normal or may only partially improveeven with smoking cessation and bronchodilator usage.
Don’t Miss: Nocturnal Asthma Or Sleep Apnea
Q& a: When Youre Diagnosed With Both Asthma And Copd
When youre diagnosed with asthma or chronic obstructive pulmonary disease , it can be difficult to breathe. But did you know that about 15% to 55% of adults with one of these lung diseases actually qualify for a dual diagnosis?
This dual diagnosis is called asthma-COPD overlap syndrome . People at risk for ACOS are typically those with asthma who smoke, but healthcare providers also see cases in those who dont use tobacco. The right diagnosis is important with lung conditions, and education is key to understanding treatment options. To learn more about ACOS, read the answers to some common questions below.
Contact Post Acute Medical Today
If you have asthma or COPD, learn more about the cardiopulmonary health services available to you by contacting Post Acute Medical today. At Post Acute Medical, we concentrate on quality care, patient satisfaction and long-term positive outcomes. Providing high-quality care to our patients is our top priority.
Find out how Post Acute Medical can help you manage your COPD or asthma by locating the facility nearest you and calling for more information.
Recommended Reading: Free Albuterol Inhaler Coupon
Which Is Worse: Copd Or Asthma
COPD is worse than asthma. With a well-designed treatment plan, asthma symptoms can be controlled sufficiently to return lung function to normal, or very close to normal, so the condition is generally considered reversible. Though COPD symptoms can be well-managed with various treatments, the respiratory disease is irreversible, so any damage impairing lung function that has occurred cannot be restored.
Symptoms And Signs Of Copd And Asthma
COPD
COPD symptoms differ on the basis of disease severity . Most patients with COPD usually first develop a chronic productive cough. However, dyspnea is the hallmark symptom of COPD and usually prompts patients to seek medical care. As disease severity progresses, cough and dyspnea result in decreased exercise tolerance and increased disability. COPD mainly affects the lungs however, notable systemic effects are also associated with COPD. Patients with COPD often experience changes in their metabolism and in caloric intake. Indeed, 50% of patients with severe disease experience weight loss, which is associated with a poorer prognosis.3 Patients with COPD also develop decreased strength, decreased exercise capacity and a reduced quality of life.3 COPD is associated with an increased risk of cardiovascular disease, respiratory infections, osteoporosis and glaucoma.
Asthma
Physiologic changes associated with asthma include bronchoconstriction, airway hyperresponsiveness and airway inflammation. Therefore, patients with asthma typically develop wheezing, shortness of breath and cough. Because asthma is also characterized by reversible airway obstruction, its symptoms are intermittent and cover a spectrum from mild-to-severe disease.
Several symptoms overlap in patients with COPD and asthma. Nevertheless, a history of wheezing strongly suggests a diagnosis of asthma, whereas chronic cough productive of sputum is more indicative of COPD.
Don’t Miss: Reduce Asthma Symptoms
Exacerbation/infection: Changes In Inflammatory Features And Cytokine Profiles
Exacerbations of asthma and COPD are clinically significant events. They are frequently triggered by viral infections of the airways and are associated with a decline in lung function and symptomatic aggravation. During exacerbation, airway inflammation becomes more exaggerated than in the mild and stable disease states, and the inflammation pattern changes. Neutrophil recruitment is a prominent feature of acute exacerbation of chronic asthma, probably owing to respiratory tract infection by viruses., Furthermore, neutrophilic inflammation in the absence of eosinophils is largely present in sudden-onset fatal asthma, and neutrophil numbers are highly elevated in status asthmaticus., Thus, severe and fatal asthma may be mediated by neutrophils, which is quite different from the classical Th2-driven eosinophilic form of the disease. In COPD patients, an allergic profile of inflammation can occur, particularly during exacerbation. Airway eosinophilia is observed in chronic bronchitic patients with exacerbation and is associated with the upregulation of RANTES in the airway epithelium., Recently, Siva et al. demonstrated that the minimization of eosinophilic airway inflammation was associated with a reduction in severe COPD exacerbation. Taken together, these studies indicate that the inflammatory characteristics of asthma and COPD are interchangeable during exacerbation and infection.
Comorbid Diseases Or Conditions
Comorbidity is the simultaneous existence of two or more diseases or conditions in an individual. Comorbidity for the purpose of respiratory disease in the CCDSS was defined as the co-existence in an individual of one of either asthma or COPD with diabetes, hypertension, mood and/or anxiety disorders, asthma or COPD .
For asthma, the prevalence of four comorbid diseases or conditions was calculated among those with and without asthma. For diabetes and mood and/or anxiety disorders, the prevalence was calculated for those age one and older for hypertension, it was calculated for those aged 20 years and older and for COPD, for those aged 35 years and older.
For COPD, the prevalence of COPD was reported among those with and without each of the comorbid conditions. Therefore the prevalence of COPD was calculated among those with and without diabetes, mood and/or anxiety disorders, hypertension and asthma. The prevalence was calculated among those aged 35 years and older among all four comorbid diseases or conditions, corresponding to the reporting age for COPD.
The following case definitions were used for the comorbid diseases and conditions:
Diabetes
Hypertension
Mood and/or Anxiety Disorder
Individuals aged one and older with at least one physician billing claim listing a mood and/or anxiety diagnostic code in the first field, or one hospital discharge abstract listing a mood and/or anxiety diagnostic code in the most responsible diagnosis field in a one-year period.
Also Check: How To Beat Asthma Without An Inhaler
Whats The Difference Between Copd And Asthma
They may cause similar symptoms, but COPD and asthma are far from the same condition. Find out about important COPD-asthma differences.
Coughing, wheezing, shortness of breath people with chronic obstructive pulmonary disease are just as familiar with these symptoms as people with asthma are, but the two conditions are actually very different from each other.
Its easy to mistake one condition for the other at first. After all, they have one big thing in common: The inability to get enough air into the lungs. Theyre also treated with some of the same medicines. So what makes them different?
Physical Changes: Common Threads, Distinct Differences
In some respects, the changes in the body that cause shortness of breath are similar between COPD and asthma. But a number of other COPD-asthma differences set the two conditions apart.
People who have COPD because of emphysema, meanwhile, have damaged air sacs in their lungs, which can lead to hyperinflation, or the inability of the lungs to return to their normal shape after expelling air. The lungs become swollen or expanded, says Anil Singh, MD, a pulmonary critical care specialist with Allegheny Health Network in Pittsburgh. That makes it hard to feel like youve caught your breath. Most people with COPD have a combination of both chronic bronchitis and emphysema.
Age of Onset: Youngsters and Adults
Causes: Genetics, Habits, and More
Treatment: The Meds Are the Same, Other Therapies Differ
What Are The Stages Of Copd
Doctors generally use the Global Initiative for Chronic Obstructive Lung Disease Program to stage COPD. These staging guidelines have been proven to be consistent and accurate by doctors and scientists. Other methods can be used to stage COPD, but they may be influenced by other factors.
There are many treatment options and ways to manage COPD. The newest 2017 guidelines emphasize the use of combined bronchodilators as first-line therapy for COPD. Doctors recommend vaccinations for people with the condition to decrease the risk of lower respiratory tract infections. Alterations in health-related behaviors is emphasized. Spirometry measurements can help determine the extent of obstructive lung disease. As COPD progresses, oxygen therapy, especially if you have obstructive sleep apnea, may help improve your survival.
Like COPD, there are many treatment options and ways to manage asthma. Your primary care doctor and/or an allergist will discuss and suggest the best choice of treatment and management drugs for you. Medications used include corticosteroids, short acting beta agonists , and occasionally anticholinergic medications for severe exacerbations.
Emergency treatment of life-threatening asthma or COPD may involve intravenous corticosteroids, intubation, mechanical ventilation, and oxygen treatment until the crisis is resolved.
Read Also: How To Make A Homemade Inhaler For Asthma
Why Does Overlap Happen
Having already analyzed all the potentially important common risk factors for overlapping asthma and COPD, such as increasing age, smoking, BHR, inflammation, remodeling and exacerbations, the big question is why does overlap happen. Dutch hypothesis tries to answer the question, stating that asthma and BHR predispose to COPD later in life and that asthma, COPD, chronic bronchitis, and emphysema are different expressions of a single airway disease. Furthermore, the presence of these expressions is influenced by host and environmental factors . Epidemiological studies, on the other hand, proved a correlation between respiratory illnesses during childhood and impaired adult lung function . Knowing that airway growth starts in utero, fetal or childhood exposures may contribute to adult asthma or COPD .
Q: Whats The Difference Between Asthma And Copd
Asthma occurs frequently in people with a family history of the disease and often begins in childhood. Symptoms include shortness of breath, wheezing, coughing, and chest tightness, and these symptoms flare up during an asthma attack. At other times, symptoms may fade or become minimal.
COPD is different and usually strikes later in life. Most people diagnosed with COPD either used to smoke, or still do. Some symptomssuch as chest tightness and coughingare similar to asthma. Other symptoms, such as mucus production, are distinct to COPD. Unlike asthma, symptoms rarely ever fade completely.
Don’t Miss: How To Get Rid Of Asthma Without Inhaler
