Predictors Of Duration Of Observation Of Patients With Acute Asthma Exacerbations
The demographics, clinical variables, pharmacologic and non-pharmacologic parameters for patients with short and long durations of observation were compared in a univariate analysis . There were significant associations between duration of observation of the patients and their gender , asthma severity , and administration of intranasal oxygen .
Table 3 Univariate analysis of the factors associated with duration of admission for 63 children with acute asthma exacerbation.
In multivariate analysis of pharmacologic and non-pharmacologic variables associated with duration of observation of the patients, adjusting for the three covariates with significant p-values in the univariate analysis, only gender and asthma severity were significantly associated with long duration of observation in the hospital. The odds of long observation in the hospital were lower for male compared to female children . Also, the odds of long observation in the hospital were lower for children with mild compared to moderate asthma exacerbation .
Table 4 Multivariate analysis of the factors associated with duration of admission for acute asthma exacerbation.
Can You Do Exercise And Sports Despite Having Asthma
Sports and physical activity are important for most people who have . Regular physical activity helps improve the performance of your heart and lungs. It increases the uptake of oxygen and the amount of air that is exhaled when you breathe out.
Because physical exertion is a relatively common trigger , many affected people think they ought to avoid exercise. But special asthma treatment can prevent problems due to physical activity. Research suggests that sports and exercise can actually reduce asthma symptoms in the long term. There is also some that interval training can prevent exercise-induced asthma. In interval training, high-energy exercise is alternated with periods of rest.
It’s important to choose physical activities that match your level of fitness, though. This may mean, for example, taking a break or doing something less strenuous if you notice signs of breathing difficulties. Warming up before doing sports, and gradually increasing the intensity, helps too. It’s also important to have reliever ‘ medication on you so you can react quickly if you do have an attack. Sometimes using reliever medication before physical exertion can help as well.
Box : Summary Of Pharmacological Treatment For Asthma Of Varying Severity
Mild intermittent asthma
-
Short acting 2-agonists as required.
Mild persistent asthma
-
Add low dose inhaled corticosteroids.
Moderate persistent asthma: select one of the following options
-
Low dose inhaled corticosteroids plus long acting 2-agonist.
-
Higher dose inhaled corticosteroids.
-
Low dose inhaled corticosteroids plus leukotriene antagonist.
-
Low dose inhaled corticosteroids plus oral theophylline.
Severe persistent asthma
-
High dose inhaled corticosteroids plus one or more of the following: long acting 2 agonist leukotriene antagonist oral theophylline oral 2-agonist.
-
Add oral corticosteroids if control still not achieved.
-
Consider corticosteroid sparing agents.
Don’t Miss: What Supplements Are Good For Asthma
What Kind Of Breathing Exercises Could Help In Asthma
People with can choose between many different breathing exercises and techniques. They are meant to have a general relaxing effect, and also help to maintain calm, controlled breathing during asthma attacks.
Relaxation and breathing techniques such as those practiced in yoga may help to prevent symptoms and improve your overall wellbeing. But there are only a small number of studies on the use of these techniques in people with asthma, and those studies aren’t very good quality. Although they suggest that the techniques might help, these findings should be interpreted with caution.
Certain techniques are meant to help people breathe more easily during serious attacks. These include techniques to help you breathe calmly and in a controlled way during an attack, or at the beginning of an attack. Panic and fear can lead to rapid and shallow breathing in such situations. Most people can still inhale quite well during asthma attacks, even during more severe ones. Exhaling can be a problem, though. Patient education can help people learn how to use breathing techniques such as pursed-lip breathing, which involves slowly breathing out through tightly pressed lips.
Treatment Of Acute Asthma Exacerbations During Admission
Patients were observed in the hospital for a short duration of 12 h or > 12 h during acute asthma exacerbations . Majority of the patients were observed in the hospital for 12 h. Nebulized salbutamol was the initial bronchodilator used to treat acute asthma exacerbations in 48 patients. Additional intravenous aminophylline was received by 9 of the 16 patients with moderate asthma exacerbations. Systemic corticosteroids , administered as intravenous or oral , were used to treat airway respiration among the patients.
Figure 4 Duration of admission for children with acute asthma exacerbation.
All patients with moderate asthma exacerbations received supplemental intranasal oxygen, based on measured SpO2 levels, while 14 had oral or intravenous antibiotics comprising amoxicillin , ampicillin/cloxacillin , cefuroxime , amoxicillin/clavulanate , and erythromycin .
Recommended Reading: Is There A Cure For Asthma Disease
A Retrospective Audit Of Pharmacologic And Non
- 1Department of Pharmacology, Therapeutics and Toxicology, Lagos State University College of Medicine, Ikeja, Nigeria
- 2Department of Clinical Pharmacy and Pharmacy Practice, Usmanu Danfodiyo University, Sokoto, Nigeria
- 3Department of Pediatrics and Child Health, Usmanu Danfodiyo University, Sokoto, Nigeria
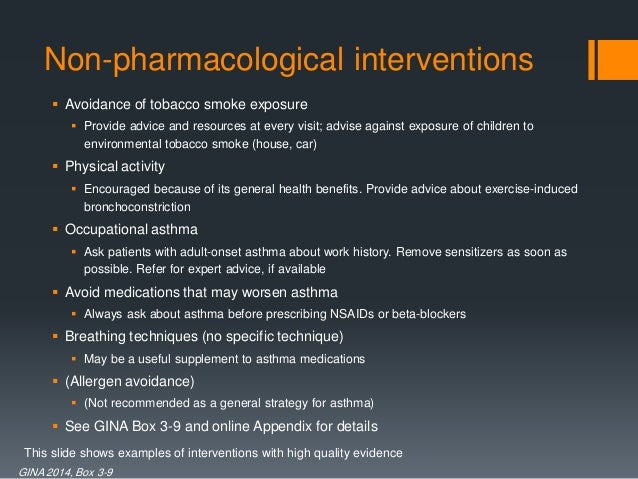
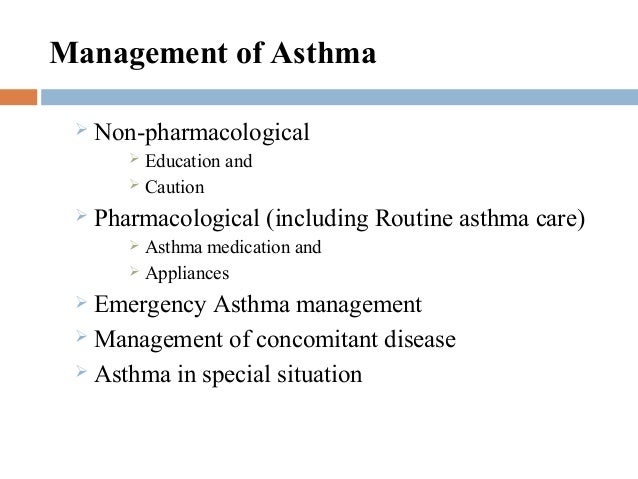
Background: Adequate management of childhood acute asthma exacerbation requires optimal non-pharmacotherapy and pharmacotherapy. Global asthma guidelines provide critical information and serves as a quick reference decision-support material for clinicians.
Objectives: We aimed at evaluating hospital management of childhood acute asthma exacerbation to ascertain its conformity to the global treatment guidelines, and to identify factors that predict short or prolonged observation in the hospital.
Method: This was a retrospective audit of the management of acute asthma exacerbation in children seen between 01 January 2017 and 31 December 2018 at Usmanu Danfodiyo University Teaching Hospital , Sokoto, Nigeria. Relevant data on demography, asthma triggers and severity, functional and clinical diagnoses, types of controller medications used before and after presentation, non-pharmacotherapy and pharmacotherapy instituted during presentation, duration of observation in the hospital, and treatment outcomes were extracted from the case file of each eligible patient.
Pharmacological Treatment Pathway For Children And Young People
This section concerns children and young people with newly diagnosed asthma or asthma that is uncontrolled on their current treatment. Where the recommendations represent a change from traditional clinical practice, children and young people whose asthma is well controlled on their current treatment should not have their treatment changed purely to follow guidance.
Also Check: What To Do If You Have An Asthma Attack
Recent Advances In The Pharmacogenetics Of Asthma
Pharmacogenetics, the study of how genetic differences influence the variability of individual patient responses to drugs, aims to distinguish responders from non-responders and thus lead to rationalised drug therapy. The clinical heterogeneity of asthma has lead to increasing interest in the study of the genetic variability of this disease. There has been particular interest in the pharmacogenetics of 2-agonists and modifiers of the cysteinyl-leukotriene pathway.
2-Agonist pharmacogenetics
The cell surface 2-adrenergic receptor, via which 2-agonists exert their effects, contains a number of genetic variants. Single nucleotide polymorphisms resulting in amino acid substitutions at positions 16 and 27 of the receptor and at position 19 of its upstream peptide are particularly common in white populations and are related to each other. The role of these genetic polymorphisms in 2-agonist treatment response remains unclear, however. Some studies, for example, have suggested that the 2-adrenergic receptor position 16 genotype is associated with the response to 2-agonist treatment with Gly16 homozygotes having diminished and Arg16 homozygotes exaggerated treatment responses. Other studies, however have failed to demonstrate such an association. It is possible that combinations of different alleles rather than single nucleotide polymorphisms are important in determining treatment responses.
Leukotriene pharmacogenetics
Demographics And Asthma Profile For The Patients
A total of 119 children presented with features of suspected acute asthma exacerbations during the study period but only 63 that met the inclusion criteria were evaluated in this study . The median age of the patients was 8 years. More males than females presented with acute asthma exacerbations. The patients presented with mild and moderate asthma exacerbations. There was no statistically significant association between gender of the patients and asthma severity . About one-third of the patients had at least one asthma related allergic condition, of which 22 had rhinitis only and 2 had both rhinitis and allergic conjunctivitis.
You May Like: Can Hay Fever Cause Asthma Like Symptoms
Practice And Research Implications
A clinical algorithm for asthma management based on objective measures and asthma symptoms could potentially reduce asthma exacerbations during pregnancy. The goals of asthma management in pregnant women are the same as in non-pregnant patients, which are to control asthma symptoms, maximize lung function, minimize medication side effects and prevent asthma exacerbations. These goals need to be considered when designing interventions, in addition to pharmacological treatment, to improve health outcomes in pregnant women with asthma. The cost-effectiveness of interventions and satisfaction of patients and health professionals also need to be assessed before implementation of such interventions in clinical practice. Further evidence is needed from well-designed prospective controlled studies in pregnant women with asthma investigating the effectiveness of interventions that incorporate patient education, patient self-management and periodic follow-up with health professionals.
Box : Factors Required For Good Asthma Control
Minimal
Nocturnal wakening due to asthma.
Asthma exacerbations.
Emergency general practitioner or hospital visits.
Time off work or school due to asthma.
Limitations to everyday activities and exercise.
Adverse effects of medication.
Peak expiratory flow/ forced expiratory volume in one second > 80% predicted for age and height
Read Also: Is It Possible To Develop Asthma
Adherence To The Gina Treatment Guidelines
In Table 2, we assessed the adherence scores for and the level of adherence to 17 major recommendations in the GINA guidelines. Of the 17 recommendations, good , moderate , and poor levels of adherence were observed. Further, evaluation of the total adherence level to all the 17 major recommendations for each patient treated by the doctors revealed moderate and poor levels of adherence in the management of 61 and 2 patients, respectively. Good adherence level to all the 17 recommendations was not observed.
Table 2 Adherence to Global Initiative for Asthma guidelines during hospital admission of 63 children with acute asthma exacerbation.
Adherence To Controller Medications Prior To Presentation
Only 40 patients were regularly or interruptedly using controller medications prior to the onset of acute exacerbations of their asthma. ICS combined with LABA was the controller medicine used by most of the patients prior to presentation . Inhaled salbutamol was the reliever medicine used by 30 patients prior to presentation.
Figure 3 Medicines used regularly by 40 patients on controller medicines prior to observation in the hospital. ICS refers to inhaled corticosteroid. LABA refers to long-acting 2-agonist. Seretide® refers to a combination of fluticasone and salmeterol. Franol® refers to a combination of ephedrine and theophylline.
Don’t Miss: How To Cause An Asthma Attack
Strengths And Weaknesses Of This Review
This is the first systematic review of the effectiveness of non-pharmacological healthcare interventions for managing asthma and improving health outcomes in pregnant women with asthma. Unpublished studies were not included in this review. A meta-analysis was not possible because of the clinical heterogeneity of the data and study designs.
What Role Does Tobacco Smoke Play
Smoking tobacco, in any form, can cause a number of medical conditions or make them worse. People with have oversensitive airways, so it’s particularly important for them to stop smoking, or not start smoking in the first place. When cigarette smoke is inhaled, many substances other than nicotine and tar get into the airways. Some, such as heavy metals and pesticides, are toxic. Just like other triggers, the substances in cigarette smoke can make the inflammation in the linings of the airways worse, causing the airways to become even narrower.
Besides this, cigarette smoke can lead to chronic over time even in passive smokers, including children who are exposed to cigarette smoke at home. Having parents who smoke is one of the main risk factors for . If teenagers who have asthma start smoking, their symptoms usually get worse.
Smokers will know how difficult it is to quit smoking. There are several therapies that can help make quitting a bit easier.
Read Also: Can Untreated Asthma Cause Fatigue
The Treatment Of Asthma: Where Are We Evolution Of A Concept
Asthma control medications reduce airway inflammation and help to prevent asthma symptoms among these, inhaled corticosteroids are the mainstay in the treatment of asthma, whereas quick-relief or rescue medicines quickly ease symptoms that may arise acutely. Among these, short-acting beta-agonists rapidly reduce airway bronchoconstriction .
National and international guidelines have recommended SABAs as first-line treatment for patients with mild asthma, since the Global Initiative for Asthma guidelines were first published in 1995, adopting an approach aimed to control the symptoms rather than the underlying condition a SABA has been the recommended rescue medication for rapid symptom relief. This approach stems from the dated idea that asthma symptoms are related to bronchial smooth muscle contraction rather than a condition concomitantly caused by airway inflammation. In 2019, the GINA guidelines review introduced substantial changes overcoming some of the limitations and weaknesses of the previously proposed stepwise approach to adjusting asthma treatment for individual patients. The concept of an anti-inflammatory reliever has been adopted at all degrees of severity as a crucial component in the management of the disease, increasing the efficacy of the treatment while lowering SABA risks associated with patients tendency to rely or over-rely on the as-needed medication.
Fig. 1
Algorithm : Pharmacological Treatment Of Chronic Asthma In Children And Young People Aged 516
Pharmacological treatment of chronic asthma in children and young people aged 516
- Offer a SABA as reliever therapy to children and young people with newly diagnosed asthma
- For children and young people with asthma who have infrequent, short-lived wheeze and normal lung function, consider treatment with SABA reliever therapy alone
- Offer a paediatric low dose of an ICS as the first-line maintenance therapy to children and young people with:
- symptoms at presentation that clearly indicate the need for maintenance therapy or
- asthma that is uncontrolled with a SABA alone
Also Check: How To Get Rid Of Phlegm Asthma
How Can You Avoid Things That Trigger Allergies
People who have that is caused by an can generally prevent asthma attacks by avoiding allergy triggers. But this isn’t always possible. For instance, it’s easier to avoid animal fur and certain foods than it is to avoid things like pollen. People who are allergic to dust mites might be able to prevent allergic reactions by making various changes in their home. These include wiping the floor with a damp cloth, using mite-proof mattress covers, regularly washing your bedding at temperatures above 55° C , and removing dust traps such as upholstered furniture and rugs.
Individual interventions like using special mite-proof mattress covers or dust mite sprays haven’t been proven to prevent symptoms, though. There is also not enough research on whether the type of bedcovers you use makes a difference. And it’s not known whether things like special air filters can help prevent asthma problems due to animal-related allergies.
Breathing Retraining Buteyko Techniques And Physical Training
There is increasing interest in breathing retraining techniques in asthma, particularly among patients and the lay press. The Buteyko technique, for example, which uses hypoventilation in an attempt to raise the partial pressure of carbon dioxide in the blood, has been advocated as a method to allow reductions in, or even withdrawal of, asthma medication. Unfortunately rigorous trials of these methods have not yet been published and they should therefore be viewed with caution. It has recently been recognised, however, that many patients treated for asthma in primary care also have symptoms suggestive of dysfunctional breathing patterns. Results of a physiotherapy based breathing retraining programme in such patients suggested significant improvements in health status in the short term, and more work in this area is clearly needed. It is likely that retraining techniques may improve symptoms and health status where there is dysfunctional breathing, either in the context of mild asthma or where asthma has been misdiagnosed. Physical training methods have been shown to improve cardiovascular fitness but not lung function in patients with asthma but effects on symptoms and quality of life have not been assessed.
You May Like: Can You Get Free Prescriptions If You Have Asthma
Targeting The Appropriate Therapy For Individual Patients
It is becoming clear that the key features of asthma: symptoms, disordered airway function, airway inflammation, exacerbations and long term decline in lung function, are not closely related to each other within patients and might have a different pathophysiological basis. Recent studies have questioned a direct causal association between eosinophilic airway inflammation and airway hyper-responsiveness, and have suggested that infiltration of airway smooth muscle by mast cells might be more important. In contrast, asthma exacerbations are more closely related to eosinophilic airway inflammation, such that the induced sputum eosinophil count has emerged as a good surrogate marker of exacerbation frequency. There is increasing evidence that some patients with asthma do not have eosinophilic airway inflammation and might not respond to inhaled corticosteroids.
Evidence for the efficacy of each class of treatment on the four major features of asthma
