What Asthma Treatment Options Are There
You have options to help manage your asthma. Your healthcare provider may prescribe medications to control symptoms. These include:
- Bronchodilators: These medicines relax the muscles around your airways. The relaxed muscles let the airways move air. They also let mucus move more easily through the airways. These medicines relieve your symptoms when they happen and are used for intermittent and chronic asthma.
- Anti-inflammatory medicines: These medicines reduce swelling and mucus production in your airways. They make it easier for air to enter and exit your lungs. Your healthcare provider may prescribe them to take every day to control or prevent your symptoms of chronic asthma.
- Biologic therapies for asthma: These are used for severe asthma when symptoms persist despite proper inhaler therapy.
You can take asthma medicines in several different ways. You may breathe in the medicines using a metered-dose inhaler, nebulizer or another type of asthma inhaler. Your healthcare provider may prescribe oral medications that you swallow.
Acute Exacerbation Of Asthma
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Heres our process.
What happens during an acute exacerbation of asthma?
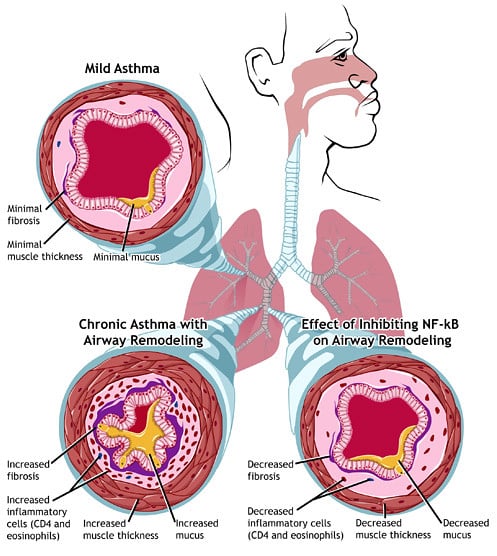
Asthma is a chronic lung disease. It causes inflammation and narrowing of your airways. This can affect your airflow.
The symptoms of asthma come and go. When symptoms flare up and get progressively worse, it can be called:
- an exacerbation
Your airways become swollen during an acute exacerbation. Your muscles contract and your bronchial tubes narrow. Breathing normally becomes more and more difficult.
Even if youve had exacerbations before and know what to do, its still a good idea to contact your doctor. An acute exacerbation of asthma is serious and can even become life-threatening. Thats why its important to recognize the symptoms early and to take appropriate action.
Its important to develop an asthma plan for how to treat your symptoms. Work with your doctor to come up with a method for what to do when your symptoms flare up.
Postdischarge Therapy And Importance Of An Action Plan
Before discharge from the hospital or the emergency department, arrangements for follow-up within 12 weeks should be made for patients. Patients who are hospitalized for their asthma may be especially receptive to information and advice about how to control symptoms and avoid future exacerbations. Health-care providers or an asthma educator should provide detailed education to all patients before discharge. Discussion should assure that the patient understands the cause of his or her exacerbation, modifiable risks factors , the purpose and correct use of medications, and an updated asthma action plan. The action plan should identify each discharge medication, the dose, and frequency. It should also outline how often to take the quick reliever medications if symptoms increase or PEF/FEV1 decreases, when to consider taking oral corticosteroids, and how to reach their primary care provider or obtain emergency care if their asthma does not respond to a step-up in therapy. Patients > 5 y of age usually are discharged with a flow meter, with instructions to keep track of their values until they are seen in follow-up. This is especially important for patients with brittle asthma or for patients identified at risk for near-fatal exacerbations of asthma. Patients should demonstrate the proper use of their inhalers and be discharged with a sufficient quantity of medication to last for at least 12 months.
Don’t Miss: What Happens If You Smoke Weed With Asthma
What Are Common Asthma Attack Triggers
You can have an asthma attack if you come in contact with substances that irritate you. Healthcare providers call these substances triggers. Knowing what triggers your asthma makes it easier to avoid asthma attacks.
For some people, a trigger can bring on an attack right away. For other people, or at other times, an attack may start hours or days later.
Triggers can be different for each person. But some common triggers include:
Blood Oxygen Level Tests
During a severe asthma attack, it may be necessary to check the level of oxygen in your blood. This can be done using a pulse oximeter. A pulse oximeter is a small device thats placed on the end of your finger. The test takes a few seconds to complete and can even be performed at home.
Shop for a pulse oximeter to use at home.
Most of the time, asthma exacerbations can be managed at home or with a visit to your doctor. The asthma plan you developed with your doctor can help you manage your symptoms and acute attacks.
However, acute exacerbations often result in a trip to the emergency room. Emergency treatment may include:
- inhaled beta-2 agonists, such as albuterol
- corticosteroids, such as fluticasone
An acute exacerbation requires close monitoring. Your doctor may repeat diagnostic tests several times. You wont be discharged until your lungs are functioning adequately. If your breathing continues to be labored, you may have to be admitted for a few days until you recover.
You may need to take corticosteroids for several days following the exacerbation. Your doctor may also recommend follow-up care.
Recommended Reading: How Do You Know If Your Asthma Is Getting Worse
What Is Status Asthmaticus
Status asthmaticus is respiratory failure that comes with the worst form of acute severe asthma, or an asthma attack. If an attack comes on quickly and it doesnât respond to regular treatment, it can lead to status asthmaticus, If it happens, you may have to go to the hospital to get it treated. If you have a bad asthma attack and your rescue inhaler or your nebulizer doesn’t help, you need medical care right away.
If you have a steroid medicine at home , you can take a dose of it on your way to the emergency room.
Many people have asthma. And there are many treatments to manage it. Itâs important to follow the asthma action plan that you made with your doctor, avoid your triggers, take your medicine, and keep up with your doctor appointments.
Still, asthma attacks can happen, and some severe ones are an emergency.
With any asthma attack, never wait to see if it goes away on its own. It could worsen so much that you need to go to a hospital.
You may hear a severe asthma attack called a âsevere asthma exacerbation.â In its most severe form, you may hear it called status asthmaticus.
Canadian Paediatric Society Acute Care Committee
Members: Carolyn Beck MD,Kevin Chan MD , Laurel Chauvin-Kimoff MD , Kimberly Dow MD , Karen Gripp MD, Kristina Krmptoic MD, Marie-Pier Lirette MD , Kyle C McKenzie MD , Evelyne D. Trottier MDLiaisons: Laurel Chauvin-Kimoff MD, CPS Paediatric Emergency Medicine Section Sidd Thakore MD, CPS Hospital Paediatrics Section
Also Check: How Long Can An Asthma Flare Up Last
The Role Of Antibiotics In Severe Asthma Exacerbations And Critical Asthma Syndrome
The role of antibiotics in acute severe AEBA and critical asthma syndrome is very limited. One study evaluating the value of anti-bacterial antibiotics in 60 adults with AEBA found no difference in length of hospital stay, time taken for 50 % improvement in symptoms and symptoms and respiratory function at the time of discharge . Another study in children admitted with status asthmaticus or critical asthma syndrome without signs of bacterial infection found no benefit in hospital course, complications or duration of hospital stay . However, the additional benefits of antibiotics may play a role that underlies their direct antibacterial effect.
Overall, the role of empiric antibiotic therapy without clear evidence of a bacterial trigger for an acute severe asthma exacerbation and critical asthma syndrome is unclear. Bacterial pathogens play a lesser role when compared to viral agents, but both typical and atypical bacteria are found with relative frequency. During the initial management moments of an acute severe exacerbation or critical asthma syndrome, the etiology, particularly an infectious one, may not be clearly evident. An approach to the use of antibiotics and antiviral therapy in severe AEBA is shown in Fig. 1.
Fig. 1
Antibacterial And Antiviral Approach To A Patient With Severe Aeba Or Critical Asthma Syndrome
Early empiric therapy in both bacterial and viral pneumonia has been shown to reduce morality, especially when initiated within 12 h . Additionally, acute exacerbations of asthma predominately have an infectious trigger, most particularly viral, but their early treatment in AEBA does not correlate with the similar outcomes of community acquired pneumonia . However, given the immediate need for care, we recommend an approach of early empiric therapy with aggressive de-escalation.
All patients presenting with severe acute asthma exacerbation and at risk for critical asthma syndrome should have a microbiologic work up that consists of standard sputum culture and a viral respiratory panel, regardless of presenting symptoms or apparent triggers. Once microbiologic testing is performed, antibacterial therapy geared towards the agents of community-acquired pneumonia . A cephalosporin, e.g., ceftriaxone with a macrolide, e.g. azithromycin is the preferred therapy over a fluoroquninolone given its anti-inflammatory properties in asthma. However, there is no clinical data to support this choice over a fluoroquinolone. In the Fall and Winter months, anti-influenza therapy with oseltamivir should be administered at 150 mg twice daily. Antibacterial and antiviral agents should be continued for at least 48 h until an alternative trigger is determine and cultures return without a specific agent. If microbiologic studies return with an agent, therapy should be tailored to that agent only.
Read Also: Is It Bad To Smoke If You Have Asthma
Will My Wheezing Or Coughing Be Worse
Not necessarily. You might be surprised to learn that you may not have more of these than usual during a severe asthma attack. So donât judge how bad your asthma attack is based on how much you wheeze or cough.
In fact, very severe asthma attacks may affect your airways so much that you donât get enough air in and out of your lungs to make a wheezing sound or cough.
Epidemiology Of Viral Infections In Aeba
Viruses are the most common cause of upper respiratory infections and lower respiratory tract infections in both children and adults. URIs occur frequently in children and most adults experience 24 URIs per year . The role of viral infections in acute exacerbations of asthma is well known with approximately 85 % to 95 % of acute exacerbation of bronchial asthma in children caused by viral infections and up to 60 % of asthma exacerbations in adults related to upper respiratory tract infections . Recent advances in the detection of viral DNA and RNA, e.g., viral respiratory panel, have helped to confirm this data with a significant increase in the weighted average of viral identification noted in patients of all ages with asthma exacerbation . The main features of viruses that may impact asthma are listed in Table 1.
Table 1 Main features of viruses that may impact asthma
You May Like: Is Tea Good For Asthma
In Addition To Ics It Is Recommended To:
| Table 3. Inhaled daily dose of corticosteroids for asthma therapy in children is available as a supplementary file. |
Fungal Infections And Acute Exacerbations Of Bronchial Asthma
The role of fungi and mold in AEBA is much less clear than viral and bacterial infections. It has been shown that fungal sensitization increases the risk of having more severe asthma and the risk of dying in asthma patients increases with increased spore exposure . Additionally, fungal sensitivity to Aspergillus and Clasdosporium species increases the risk of adult-onset asthma . The term severe asthma associated with fungal sensitization has been previously coined to describe patients with fungal sensitivity and persistent severe asthma who have some improvement with antifungal therapy . Denning et al. demonstrated a significant improvement in quality of life in patients with SAFS who were treated with oral itraconazole for 8 months . More specifically, sensitivity to Aspergillus fumigatus has been directly linked to severe persistent asthma in adults and is the cause of allergic bronchopulmonary aspergillosis . Both oral corticosteroids and antifungal therapies have been shown to be partially successful in controlling symptoms of ABPA including improving asthma related symptoms.
You May Like: What Are The Symptoms Of An Asthma Attack
Hows An Acute Exacerbation Of Asthma Diagnosed
If youve had an acute exacerbation before, youll probably recognize the symptoms. Your doctor will be able to make a quick diagnosis.
If its your first acute exacerbation, your doctor will need to know your medical history, particularly your history of asthma. To make a proper diagnosis, your doctor will likely perform a physical exam and a test of your lung function.
There are several tests that may be used to see how well your lungs are working:
Therapy In The Emergency Department
Patients with mild-to-moderate asthma exacerbations may present to the emergency department to seek medical care. These patients should be treated as an out-patient when following the recommendation detailed above. Patients with severe or life-threatening asthma should always be managed in the emergency department. A focused, expedited history and physical examination should be carried out in all patients. It is critical to rule out other conditions that may mimic a severe asthma exacerbation, such as pneumonia, congestive heart failure, pneumothorax, and myocardial infarction. In patients with a severe exacerbation, careful attention should be placed on the level of consciousness, oxygen saturation, breathing frequency, resting pulse, and blood pressure, and on the use of accessory respiratory muscles. Patients with severe asthma may have a fast deterioration of their clinical presentation, so continuous monitoring of these patients is warranted. In the advanced stages of an asthma exacerbation, the pulmonary physical examination may reveal a silent chest, which may herald impending respiratory failure. Patients with severe asthma should also be monitored for potential complications of asthma, such as pneumothorax, pneumomediastinum, and anaphylaxis.
Also Check: What Causes Asthma In Children
Types Of Asthma And Biomarkers
Types of asthma and biomarkers
In adults, two common types of asthma are distinguished: allergic asthma, where there is a clear relationship to allergy, and intrinsic or eosinophilic asthma, which usually starts in adulthood without evidence of any relevant allergies.
In adults, two common types of asthma are distinguished. The first is allergic asthma, where there is a clear relationship with allergy. Onset is often during childhood or adolescence and often accompanied by allergic rhinitis and/or atopic dermatitis this form is known as early-onset asthma. The second is an intrinsic type, usually with onset in adulthood and usually without evidence of any relevant allergies this form is referred to as adult-onset or late-onset asthma) . In both types of asthma, an increased level of typical cytokines and eosinophil granulocytes is found, together with dysfunction of structural cells characteristics referred to collectively under the name type 2 asthma . The inflammation can be measured through biomarkers . Routine diagnostic procedures covered by statutory health insurance carriers in Germany include blood eosinophil count and allergy markers fractional exhaled NO measurement is available as a self-pay option. It should be noted that these biomarkers can be falsified: for example, eosinophil counts can be greatly reduced by inhaled or oral steroids and FeNO levels by tobacco smoke .
Assessment Of Respiratory Distress
Effective treatment depends on an accurate and rapid assessment of disease severity and the elimination of other differential diagnoses . Assessment should include:
- Signs and symptoms of respiratory distress and airway obstruction, including documentation of vital signs. Pulse oximetry should be used in all patients. Pulse oxygen saturation of 92% or less on presentation is associated with higher morbidity and ED management failure .
- A focused asthma history recording triggers for exacerbation, previous medications and risk factors for ICU admission and death :
- Previous life-threatening events, admissions to an intensive care unit , intubation
- Hospitalizations or ED visits for asthma in the last year
- Deterioration while on, or recently after stopping, systemic steroids
- Using > 1 canister of salbutamol per month
- Lack of an asthma action plan or poor adherence to treatment
- Low socioeconomic status, psychosocial concerns
Particularly when risk factors are identified, prompt and aggressive treatment is indicated, and caution should be used in determining readiness for discharge. Early consultation with a tertiary care paediatric ED and/or paediatric intensive care unit specialist to discuss patient management and transport when response to treatment is insufficient is advised.
Recommended Reading: Can Asthma Make Your Heart Race
Unproved Alternate Therapy In Status Asthmaticus
Although the application of noninvasive ventilation has proved to be safe and effective in COPD, the use of NIV in severe asthma is not clearly defined. A systematic review found 5 studies with > 200 subjects with severe asthma randomized to NIV or placebo. Two of the studies found no difference in the number of subjects who required intubation and mechanical ventilation , whereas one study demonstrated fewer admissions in the NIV group. NIV should not be attempted in patients who are agitated or uncooperative, and patients should be monitored closely if NIV is attempted. Although retrospective studies are encouraging about the potential benefits of NIV, in our experience, many patients with acute, severe asthma are unable to tolerate NIV.,
Although intravenous aminophylline is not likely to result in any additional bronchodilation when compared with standard care with inhaled bronchodilators and corticosteroids, some patients with near-fatal asthma may gain benefit with intravenous aminophylline. The usual loading dose of 5 mg/kg is given intravenously over 20 min and then infused at a rate of 0.50.7 mg/kg/h. Such patients are rare, and the potential adverse effects are not uncommon . Blood levels should be checked daily for all patients receiving aminophylline infusions.
