Why Does It Occur
Underdiagnosis may be due to medical professionals failing to recognise the disease, and perhaps attributing symptoms to obesity, deconditioning, cardiac disease or other causes. The patient may appear well with no abnormality on examination and if objective tests for asthma are carried out, particularly as a one off or when the patient is already on treatment, they may be falsely reassuring or misunderstood by the treating physician as excluding asthma. One might speculate that because asthma is so prevalent, patients are less likely to be referred to specialists for confirmation of the diagnosis when it is unclear, whereas patients with suspected diseases that are less familiar may be more likely to be referred.
How Do Doctors Diagnose Asthma
To determine whether or not you have asthma, your doctor will probably ask you some medical questions, including about your familys medical history.Asthma can be hereditary , so knowing your familys health history can indicate whether its a possibility for you.
The doctor will also ask about symptoms, triggers, exercise habits, etc. Once all of the basic questions have been answered, your doctor will perform a physical exam.
Asthma Signs & Symptoms
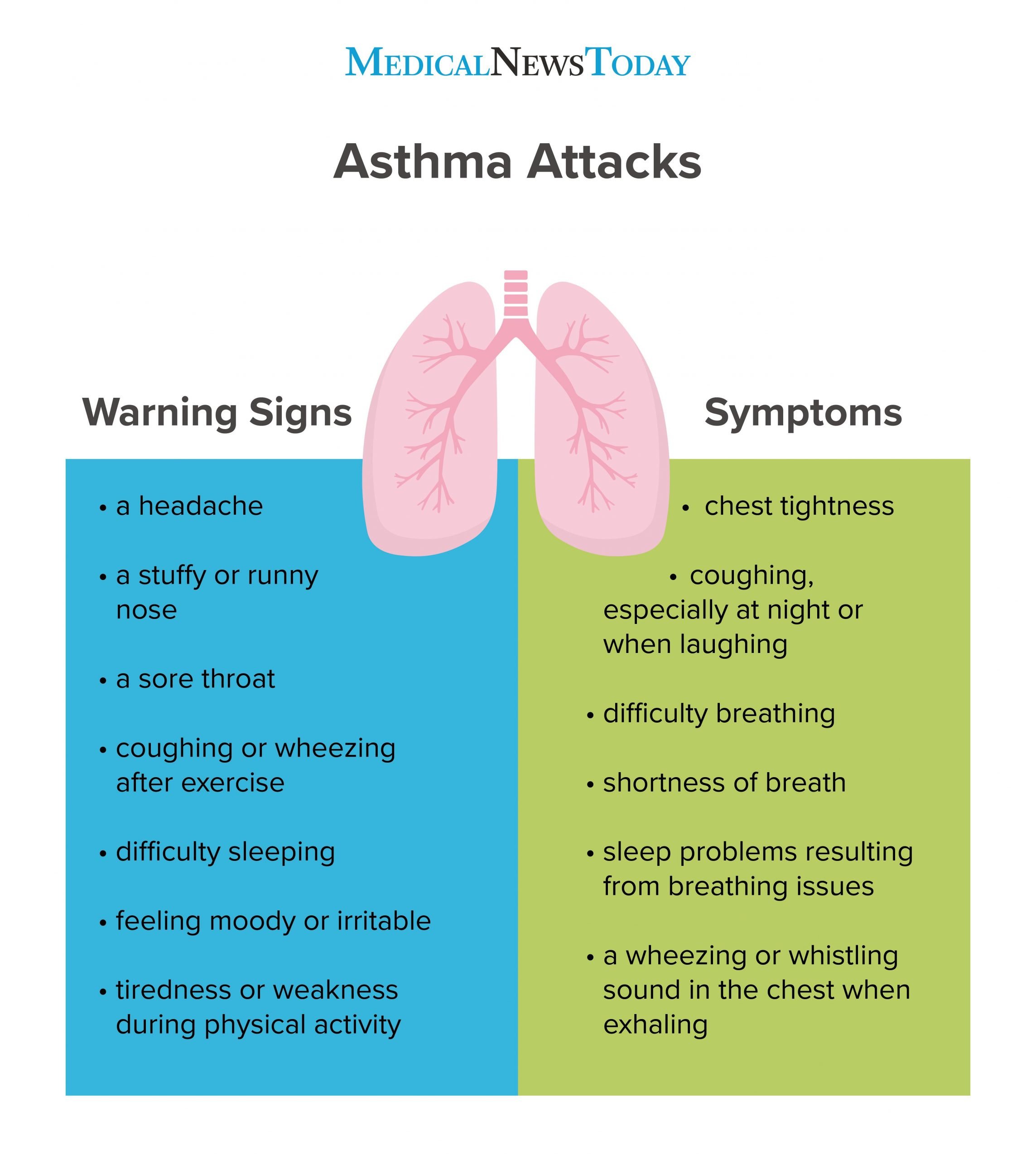
People with asthma experience symptoms due to inflammation in the airways. They might only occur when you encounter an asthma trigger. Common symptoms that can lead to a diagnosis of asthma include:
- Persistent or recurring coughing: which often occurs at night or early in the morning, although it can happen at any time. Coughing is a major feature of asthma, especially in children and can sometimes be the only sign of asthma.
- Wheezing: is difficulty breathing accompanied by a whistling sound coming from your airways
- Shortness of breath: gives you the feeling that you cant get enough air into your lungs, and may even find it difficult to eat, sleep or speak
- Chest tightness: an unpleasant sensation of heaviness or pressure in the chest that can make it hard to breathe
- Increased mucus production: is characterized by high levels of thick fluid or phlegm accumulating in your airways
- Difficulty breathing while exercising: having trouble breathing while performing physical activities can be a sign of asthma
- Losing Sleep: Being unable to sleep through the night because of breathing troubles
Don’t Miss: How Can You Tell If You Have Asthma
Signs And Symptoms Of An Asthma Attack
The difference between having asthma and having an asthma attack is the severity of the symptoms. Otherwise, the symptoms, themselves, are mostly the same.
So, if you have asthma, you will likely have had most of the symptoms of an asthma attack already, just in a milder form, says Troy Madsen, MD, a professor of emergency medicine at the University of Utah.
Some of the most common symptoms of an asthma attack include:
- Extreme shortness of breath
- Tightness in your chest
Fourth Stage: Severe Persistent Asthma
This is the most severe level of asthma, where control is basically non-existent. Quality of life is greatly affected and missed school and work days are frequent.
Symptoms. Daytime symptoms are continual and nighttime symptoms are frequent. Basically, the person in this stage will feel as though they are in a continuous flare-up.
Lung function tests. In this stage of asthma, the FEV 1 is 60% or less of normal values. Peak flow readings have more than 30% variability.
Treatment. The preferred controller medication is an inhaled medium-dose steroid plus a long-acting beta agonist . Alternatives include an inhaled medium-dose steroid, plus either a leukotriene receptor antagonist or theophylline. If neither of those medication regimes result in asthma control, then an inhaled high-dose steroid plus a long-acting beta agonist combination will be tried. And if that does not produce control, then an inhaled high-dose steroid/long-acting beta agonist combination will be prescribed, plus an oral steroid, such as prednisone. Other treatment options for uncontrolled asthma might include:
- tiotropium mist inhaler for patients with a history of exacerbations
- omalizumab for severe allergic asthma
- mepolizumab for severe eosinophilic asthma
Recommended Reading: How To Relieve Asthma Without Inhaler
The Test Can Save Money
A spirometry test generally costs less than $100. Not having the test can cost a lot more money. If the test shows that you do not have asthma, this can save you hundreds of dollars a month for asthma medicines. If you do not have the test and you have asthma, an emergency room visit for an asthma attack can cost thousands of dollars.
Treating Acute Loss Of Asthma Control5
1. Assess the severity of the asthma attack:
- Severe life-threatening: While arranging urgent transfer to an acute care facility treat the patient with short-acting beta2-agonists , controlled oxygen and oral corticosteroids .
- Mild-moderate: treat in the primary care setting .
2. Goals of treatment:
- Identify and address the cause of the asthma attack, and
- Reduce risk of relapse by reviewing and adjusting maintenance treatment plan.
3. Treatment steps:
Recommended Reading: How To Get Rid Of Asthma Without Inhaler
Tests For Other Conditions
The doctor may also do tests for other conditions that can make asthma worse, like:
- Gastroesophageal reflux disease
The Canadian Lung Association: “Signs and Symptoms of Asthma: Diagnosis.”
National Jewish Medical and Research Center: “How Is Asthma Diagnosed?”
American College of Allergy, Asthma & Immunology: “About Asthma: Diagnosing Asthma.”
Mayo Clinic: âAsthma: Steps in testing and diagnosis.â
Medscape: âAsthma Guidelines.â
American Academy of Asthma, Allergy, and Immunology: “What to expect at the doctor’s office.”
American Lung Association: “Spirometry and Other Lung Function Tests Fact Sheet.”
American Medical Association: Essential Guide to Asthma.
Asthma and Allergy Foundation of America: “Peak Flow Meters.”
Grayson, M. ACP Medicine, 2005.
National Asthma Education and Prevention Program: “Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma — 2002.”
National Heart, Lung and Blood Institute: “Asthma: How is Asthma Diagnosed?”
MedlinePlus: “Pulmonary Function Tests.”
National Lung Health Education Program: “Spirometry.”
Definitive Diagnosis Of Asthma
The diagnosis of asthma requires a history or current presence of respiratory signs and symptoms consistent with asthma , combined with the objective demonstration of variable airflow obstruction. Variable airflow obstruction means that the obstruction is not necessarily present at all times, varying with time, exposure to asthma triggers and treatment. A good response to asthma treatment in a patient with a typical history of asthma supports a diagnosis of asthma. However, objective confirmation of the variable airflow obstruction characteristic of asthma, using spirometry or peak expiratory flow monitoring, is required, especially for patients whose response to treatment is suboptimal or whose symptoms are not highly suggestive of asthma.,,
Spirometry is recommended for all patients to confirm the diagnosis of asthma before initiation of possibly lifelong therapy. This form of objective testing is preferred over peak flow measurement because of the wide variation in predicted values for peak flow rates . Diagnosis is consequently less accurate if it is based on peak flow monitoring or a trial of therapy. Unfortunately, many clinicians diagnose asthma without confirming the diagnosis with objective testing, and misdiagnosis and mistreatment, particularly overtreatment, are therefore common.,
The presence of one of the following is required to confirm reversibility of airflow obstruction, which is the hallmark of asthma :
You May Like: What Happens If You Smoke Weed With Asthma
Adult Vs Childhood Asthma
Its common for children to have asthma symptoms that come and go, for example triggered by allergy or a respiratory infection. Adult-onset asthma tends to have persistent symptoms that are often not associated with allergic triggers.
About one in ten adults with asthma have uncontrolled symptoms and exacerbations despite treatment. Such difficult-to-treat asthma can reduce quality of life and also lead to more deaths than we see with childhood asthma. We dont know why adult asthma doesnt respond as well to treatment as childhood asthma. It may be because adult lungs can be stiff and function less well than a childs lungs. Also the bodys immune response may change as we get older.
Its reassuring to remember that death from asthma in adulthood is still uncommon.
Adults also tend to have other illnesses that are affected by asthma and allergy medications. For example oral steroids can worsen the symptoms of glaucoma, cataracts and osteoporosis.
Tests To Identify Triggers
If you have persistent asthma and take medicine every day, your doctor may ask about your exposure to substances that cause an allergic reaction. For more information about testing for triggers, see the topic Allergic Rhinitis.
Allergy tests can include skin tests and a blood test. Skin tests are needed if you are interested in immunotherapy, such as allergy shots.
Also Check: How To Get Rid Of Asthma Without Inhaler
Second Stage: Mild Persistent Asthma
Although this stage is still relatively mild, asthma is beginning to become more noticeable and starting to interfere with your quality of life.
Symptoms. In mild persistent asthma, daytime symptoms are occurring 3 to 6 times a week. Nighttime symptoms interfere with sleep nearly every week, or 3 to 4 times a month. Flare-ups are more severe and may affect activity levels.
Lung function tests. As with intermittent asthma, the FEV1 is 80% or more above normal values. Peak flow readings show less than 20-30% variability.
Treatment. A low dose inhaled steroid will be used as a controller medication to prevent and control symptoms. Less common alternatives might include cromolyn, a leukotriene receptor antagonist , or theophylline. The doctor will also prescribe a quick-relief inhaler for flare-ups.
Key Points About Asthma In Adults
Asthma is thought to be caused by a combination of genetic and environmental factors.
Don’t Miss: Asthma Waiver Army
Complete Pulmonary Function Testing
Your asthma care provider may want to determine your lung volumes and diffusing capacity. This is often done if your asthma diagnosis is unclear. The test requires you to sit inside a special box that helps determine how much air you breathe in and out.
- Lung Volumes: Your asthma care provider may order body plethysmography test to determine your lung volumes. Asthma may cause certain changes in lung volumes that will assist your asthma care provider in diagnosing or treating your asthma.
- Diffusion Capacity: Diffusion capacity measures how well oxygen flows from the lungs into your blood. Poor diffusion indicates damage to the lung where the oxygen and blood meet in the lungs. Diffusion capacity is usually normal in asthmatics.
First Stage: Intermittent Asthma
At this stage, asthma is likely more of on occasional bothersome occurrence, rather than a disease that interferes significantly with day to day quality of life. I speak from experience — my asthma has been at this stage for some years, although when I was younger and living in a different climate, it was more severe.
Symptoms. With intermittent asthma, daytime symptoms generally occur less than twice a week. Nighttime symptoms that interfere with sleep occur less than twice a month. Although symptoms might intensify into a flare-up at times, severity varies and the flare is brief. In between flare-ups, there are no active symptoms.
Lung function tests. To aid with diagnosis and treatment, the doctor may order a lung function test that measures your ability to breathe effectively. The test is expressed in terms of FEV, or Forced Expiratory Volume, and the resultant FEV1 will be 80% or more above normal values. If a peak flow meter is used, the readings show less than 20% variability am-to-am or am-to-pm, day-to-day.
Treatment. In terms of treatment for intermittent asthma, a daily controller medicine is usually not needed. However, a quick-relief, or rescue, inhaler will be prescribed to be used when symptoms do arise or flare-up.
Read Also: How Can You Tell If You Have Asthma
What Are The Treatments For Asthma
If you have asthma, you will work with your health care provider to create a treatment plan. The plan will include ways to manage your asthma symptoms and prevent asthma attacks. It will include
- Strategies to avoid triggers. For example, if tobacco smoke is a trigger for you, you should not smoke or allow other people to smoke in your home or car.
- Short-term relief medicines, also called quick-relief medicines. They help prevent symptoms or relieve symptoms during an asthma attack. They include an inhaler to carry with you all the time. It may also include other types of medicines which work quickly to help open your airways.
- Control medicines. You take them every day to help prevent symptoms. They work by reducing airway inflammation and preventing narrowing of the airways.
If you have a severe attack and the short-term relief medicines do not work, you will need emergency care.
Your provider may adjust your treatment until asthma symptoms are controlled.
Sometimes asthma is severe and cannot be controlled with other treatments. If you are an adult with uncontrolled asthma, in some cases your provider might suggest bronchial thermoplasty. This is a procedure that uses heat to shrink the smooth muscle in the lungs. Shrinking the muscle reduces your airway’s ability to tighten and allows you to breathe more easily. The procedure has some risks, so it’s important to discuss them with your provider.
How Can Adult Onset Asthma Be Managed
If you manage your asthma, you can expect to lead a normal lifestyle. Basically, there are four key steps to managing asthma successfully:
1. Learn about asthma and stay up-to-date on new developments.
2. Take prescribed medications. Dont make any changes until you check with your physician. Dont use over- the-counter medications unless prescribed by your physician!
3. Check your lungs daily at home by using a peak flow meter. Asthma patients often can detect lung changes with a peak flow meter before they actually experience any changes. Visit your physician regularly for further in-office tests. Lung testing is painless and provides valuable data that helps your physician make adjustments in your medication.
4. Make an asthma management plan with your physician. A plan establishes guidelines that tell you what to do if your asthma symptoms get worse.
Don’t Miss: After Asthma Attack
How Do You Use A Peak Flow Meter
Step 1: Before each use, make sure the sliding marker or arrow on the Peak Flow Meter is at the bottom of the numbered scale .Step 2: Stand up straight. Remove gum or any food from your mouth. Take a deep breath . Put the mouthpiece of the peak flow meter into your mouth. Close your lips tightly around the mouthpiece. Be sure to keep your tongue away from the mouthpiece. In one breath, blow out as hard and as quickly as possible. Instead of slowly blowing, blow a fast, hard blast until you have emptied out nearly all of the air from your lungs.Step 3: The force of the air coming out of your lungs causes the marker to move along the numbered scale. Note the number on a piece of paper.Step 4: Repeat the entire routine three times. Step 5: Record the highest of the three ratings. Do not calculate an average. This is very important. You can’t breathe out too much when using your peak flow meter but you can breathe out too little.Step 6: Measure your peak flow rate close to the same time each day. You and your healthcare provider can determine the best times. One suggestion is to measure your peak flow rate twice daily between 7 and 9 a.m. and between 6 and 8 p.m. You may want to measure your peak flow rate before or after using your medicine, or both. Try to do it the same way each time.Step 7: Keep a chart of your peak flow rates. Discuss the readings with your healthcare provider.
What Are The Consequences Of Overdiagnosis
One of the problems of misdiagnosis is that there may be an alternative diagnosis that is not made in a timely fashion. Some of the final diagnoses in the study by Aaronet al. , such as ischaemic heart disease, subglottic stenosis and pulmonary hypertension, were serious and could lead to patient harm if unrecognised. In addition to this risk, patients are often on long-term inhaled therapy unnecessarily, leading both to potential side-effects and significant ongoing healthcare costs as these drugs are likely to be issued for many years after a diagnosis of asthma. In the past, many mild asthma patients were simply on an as required SABA inhaler, but increasingly this is discouraged with daily ICS therapy recommended for all but a few . This represents a burden to the patient and could conceivably cause side-effects such as an increased risk of adrenal suppression, diabetes, cataract formation and pneumonia . If the wrong diagnosis is made patients are also likely to remain symptomatic, and potentially have their asthma treatment stepped up, adding to both the cost and the potential for side-effects.
Read Also: Does Asthma Ever Go Away
How To Get A Diagnosis
The first thing to do is book an appointment. Your GP or an asthma nurse can help confirm or rule out a diagnosis of asthma.
They can do this by:
- talking about your symptoms, what sets them off, and when you get them
- asking if anyone else in the family has asthma
- finding out if you, or anyone in your family, have other allergies, like hay fever
- testing how your lungs are working
- listening to your chest for any sounds of wheezing
- prescribing asthma treatments to see if they make a difference
- considering any other symptoms that might suggest something else.
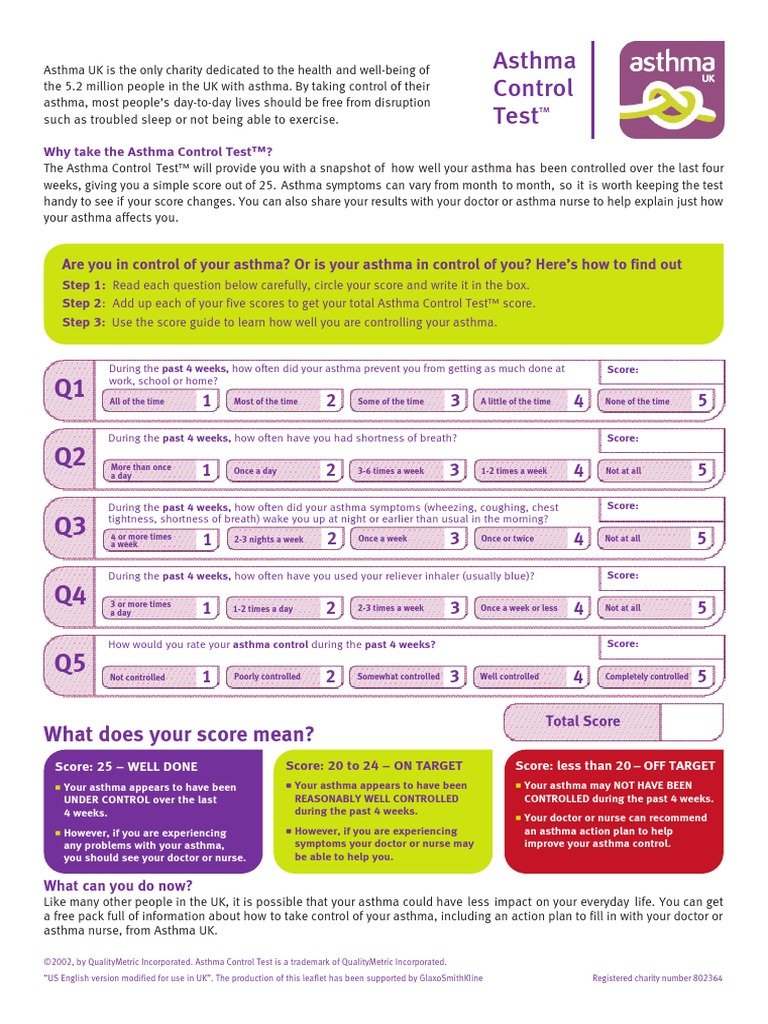
Asthma tests
Alongside a full clinical assessment by your GP, youll need some asthma tests to confirm or rule out asthma. Your GP can see how your lungs are working with tests like peak flow, spirometry, and FeNo .
Your GP can usually perform these tests during the appointment, and you can see the results straight away. But you may need to do tests again on another day before your GP can confirm you have asthma.
You may be given a peak flow meter to use at home for a couple of weeks. This is so you can record your own peak flow scores in a diary.
When you take it back to your appointment, your GP or asthma nurse will be able to see a pattern of scores that could suggest asthma.
Trying out asthma treatments
Your GP or asthma nurse may prescribe asthma treatments to see if they help. This is sometimes called a trial of treatment.
If your symptoms start to get better, it suggests you could have asthma.
