How Is Asthma Diagnosed
To diagnose asthma, a doctor will do a physical exam and ask about the person’s medical history, including whether anyone else in the family has asthma.
The doctor might do tests like spirometry or peak flow meter tests. These involve blowing into devices that can measure how well the lungs are working. Allergy tests or exercise tests can tell doctors if asthma is brought on by allergens or physical activity. Doctors may use X-rays to rule out other problems.
The Cell Biology Of Asthma
- Abbreviations used in this paper:
Rho-associated coiled-coil containing protein kinase
SAM-pointed domaincontaining Ets-like factor
signal transducer and activator of transcription 6
J Cell Biol
David J. Erle, Dean Sheppard The cell biology of asthma. J Cell Biol 9 June 2014 205 : 621631. doi:
The clinical manifestations of asthma are caused by obstruction of the conducting airways of the lung. Two airway cell types are critical for asthma pathogenesis: epithelial cells and smooth muscle cells. Airway epithelial cells, which are the first line of defense against inhaled pathogens and particles, initiate airway inflammation and produce mucus, an important contributor to airway obstruction. The other main cause of airway obstruction is contraction of airway smooth muscle. Complementary experimental approaches involving cultured cells, animal models, and human clinical studies have provided many insights into diverse mechanisms that contribute to airway epithelial and smooth muscle cell pathology in this complex disease.
What Else Should I Know
The best way to manage asthma is to prevent flare-ups. Do that by following your asthma action plan and avoiding triggers, taking any medicines your doctor prescribes as directed, and getting a flu shot each year.
Your doctor also may ask you to keep track of your asthma symptoms in an asthma diary. This can help the doctor track how you feel after taking medicines. Your doctor might also ask you to use a peak flow meter as a way to monitor your asthma.
Caring for asthma takes a bit of work. But if you follow your asthma action plan, take your medicines properly, recognize your symptoms and triggers, and check in with your doctor regularly, you can do anything that people without asthma do.
Don’t Miss: How To Treat Asthma Attack Without An Inhaler
Looking At Genes And The Environment To Work Out What Causes Wheezing In Preschool Children And Find Treatments To Prevent Development Of Asthma
- Supervisor: Dr Sejal Saglani
- Type of grant: PhD studentship
- Institution: Imperial College London
- Grant duration: 48 months
- Start date: October 2016
Project title: Gene-environment interactions mediating preschool wheeze: the role of 17q21, farmyard microbes and innate cytokines
About one-third of children under the age of 5 experience wheezing and breathlessness, but not all of them go on to develop asthma by school age. Children with asthma have a reduced lung function by age 6 that is irreversible.
Recent research has shown that some children who wheeze when they have a cold or other viral infection before the age of three, who dont go on to develop asthma and are thought to have outgrown it, are actually at an increased risk of developing lung conditions like COPD as adults.
There are no medicines to prevent the progression from wheeze to asthma, or ways to predict who will prevent lung damage later in life.Previous studies have shown strong associations between a particular area of DNA, including two particular genes – called ORMDL3 and GSDMB – and people who wheeze in early life and go on to develop asthma.
Additionally, we know that growing up on a farm protects children from developing asthma as the types of bugs that they breathe in seem to be protective. Even those with the genetic susceptibility of the genes above halve their chance of developing asthma following viral wheezing early in life if living on a farm.
What Part Of The Respiratory System Is Affected By Asthma
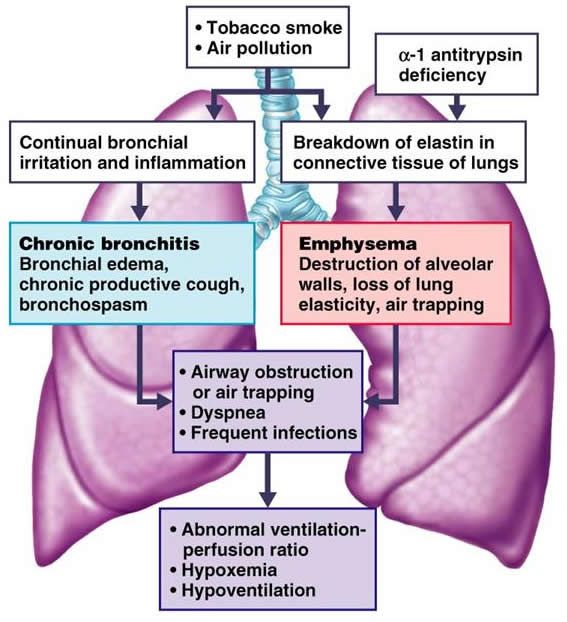
Asthma is a chronic condition that affects 10s of thousands of people across the world. Although it isnt curable it is controllable. Asthma is the Greek word for pant or to breath hard. The Greeks named it asthma because of the wheezing sound which is diagnostic of the condition.
Asthma is a chronic respiratory condition that arises from allergies or allergic responses in the lungs and is characterized by sudden attacks of labored breathing, chest constriction and coughing. So what part of the respiratory system does asthma affect?
The respiratory system supports the oxygen needs of the body by taking in air, removing the oxygen at the level of the alveoli and delivering the oxygen to the blood, which then transports the life supporting oxygen around the body. This is a continual system.
The air is exchanged constantly not just when you take air in. There are thousands of tiny air sacs that store the air and oxygen for use. The air is exchanged with each pass of the blood through the pulmonary system.
During an asthmatic event the muscles surrounding the air tubules constrict. This constriction doesnt allow the air in the alveoli to be released and the lungs become over inflated. This over inflation forces the sufferer to cough in an attempt to get rid of the trapped air.
Also Check: What Is The Blood Test For Eosinophilic Asthma
Looking For Small Genetic Differences As A Cause Of Asthma
- Researcher: Dr Rachel Clifford is a researcher at the University of Nottingham
- Start date: March 2016
- How long will the project run for? 36 months
- Project type: Project grant ).
- Cost: £299,645
Project title: Airway smooth muscle DNA methylation: A novel target for asthma therapy
All of our cells contain all of our DNA this is a lot of information, and each cell will only need to use a tiny amount of it to do its job well. The body has a very clever system to ‘wrap up’ the DNA that isn’t needed so that it fits into a small space, and for highlighting the genes that should be used by a cell. This means that a cell in the muscles in our airway only ‘sees’ information that will help it to be an airway muscle cell and irrelevant information about its job, for example information about the colour of our eyes, is locked out of the way.
However, sometimes there are genes within a cell that are needed sometimes and not others these will be ‘visible’ to a cell, and a separate clever signalling process is used to show which genes should be ‘on’ and which should be ‘off’ at any time.
Sometimes, this signalling process goes awry and gives the cells the wrong signal this can result in cells that misbehave. In the case of asthma, it’s thought that airway muscle cells in people with asthma have this confusion, which results in them becoming more ‘twitchy’ and contracting too often, causing asthma symptoms.
How Are Asthma And Pneumonia Diagnosed
If you have the symptoms of asthma, your doctor will want a complete medical history. A physical exam includes inspecting your nose, throat, and airways.
Your doctor will use a stethoscope to listen to your lungs as you breathe. A whistling sound is a sign of asthma. You may also be asked to breathe into a spirometer to test your lung function. They may also perform allergy tests.
If your symptoms point toward pneumonia, your doctor will probably start by listening to your lungs. One of the hallmarks of pneumonia is that your lungs make a crackling sound when you breathe.
In most cases, a chest X-ray can confirm the diagnosis. If necessary, a CT chest scan can get a more detailed look at lung function.
You may also need blood work to make sure youre getting enough oxygen and to get a count of your white blood cells . Checking your mucus can also help your doctor determine what type of pneumonia you have.
Asthma requires both short-term treatment and long-term management. In most cases, doctors can treat and cure pneumonia within a short time.
Don’t Miss: T2 Asthma
Evaluating An Asthma Attack
Because people who are having a severe asthma attack commonly have low blood oxygen levels, doctors may check the level of oxygen by using a sensing monitor on a finger or ear . In severe attacks, doctors also need to measure levels of carbon dioxide in the blood, and this test typically requires obtaining a sample of blood from an artery or, occasionally, a vein. However, carbon dioxide levels can sometimes be monitored in the person’s breath using a sensor placed in front of the nose or mouth.
Doctors may also check lung function, usually with a spirometer or with a peak flow meter. Usually, a chest x-ray is needed only when asthma attacks are severe, in order to rule out other serious conditions .
Viral Infection To Predisposition
The fact that early-in-life sensitization to multiple allergens carries the greatest risk for developing asthma brings the question of what factors result in a predisposition to this phenotype. Although infection with rhinovirus is the major cause of acute exacerbation, in those genetically at risk of asthma, rhinovirus-induced wheezing in the first three years in the life is also the greatest risk factor for developing asthma at 6 years of age . Impaired TLR3-mediated IFN- and – production by asthmatic epithelial cells would make susceptible to both viral infection and allergic sensitization . Reduced primary IFN production by lower-airway epithelial cells enables some viruses to replicate, leading to cytotoxic cell, release of inflammatory products and enhanced viral shedding. Such events provide a strong stimulus for recruitment of immature DCs and their priming for allergen sensitization . When asthmatic epithelial cells are received to damage by rhinovirus infection, the cells generate increased amounts of the pro-Th2 cytokine thymic stromal lympoietin , which stimulates DCs and increases allergic inflammation, whereas exogenous IFN-b applied to asthmatic epithelium exerts anti-Th2 as well as antiviral properties .
Don’t Miss: Can A Humidifier Help With Asthma
Medical Conditions In Adults
- This list is presented in alphabetical order and not in order of risk.
- CDC completed an evidence review process for each medical condition on this list to ensure they met criteria for inclusion on this webpage.
- We are learning more about COVID-19 every day, and this list may be updated as the science evolves.
Cell Biology Of Airway Epithelium
The airway is covered with a continuous sheet of epithelial cells . Two major airway cell types, ciliated and secretory cells, establish and maintain the mucociliary apparatus, which is critical for preserving airway patency and defending against inhaled pathogens and allergens. The apparatus consists of a mucus gel layer and an underlying periciliary layer. Ciliated cells each project 300 motile cilia into the periciliary layer that are critical for propelling the mucus layer up the airway. In addition, cilia are coated with membrane-spanning mucins and tethered mucopolysaccharides that exclude mucus from the periciliary space and promote formation of a distinct mucus layer . Secretory cells produce a different class of mucins, the polymeric gel-forming mucins. The two major airway gel-forming mucins are MUC5AC and MUC5B. Some secretory cells, known as mucous or goblet cells, produce mucins and store them within easily visualized collections of mucin granules, whereas other cells produce and secrete mucins but lack prominent granules. Gel-forming mucins are secreted into the airway lumen and are responsible for the characteristic viscoelastic properties of the mucus gel layer.
You May Like: What Happens If You Smoke Weed With Asthma
How Can I Stop My Asthma Getting Worse Over Time
The best way to stop your asthma getting worse over time is to stick to a good routine of taking your preventer medicines as prescribed.
And if you notice your symptoms are getting worse, see your GP or asthma nurse as soon as possible so they can review your treatment.
You can also cut your risk of frequent asthma attacks, and your asthma getting worse, by stopping smoking.
Having an asthma review at least once a year, gives you a chance to talk through any symptoms or new triggers. You can check youre on the right medicine and that youre using your inhaler in the right way to get the most benefits.
You can also talk to your GP or asthma nurse about whether you need a higher dose or an add-on treatment to help with symptoms.
Reducing The Burden Of Asthma
Asthma cannot be cured, but good management with inhaled medications can control the disease and enable people with asthma to enjoy a normal, active life.
There are two main types of inhaler:
- bronchodilators , that open the air passages and relieve symptoms and
- steroids , that reduce inflammation in the air passages. This improves asthma symptoms and reduces the risk of severe asthma attacks and death.
People with asthma may need to use their inhaler every day. Their treatment will depend on the frequency of symptoms and the different types of inhalers available.
It can be difficult to coordinate breathing using an inhaler especially for children and during emergency situations. Using a spacer device makes it easier to use an aerosol inhaler and helps the medicine to reach the lungs more effectively. A spacer is a plastic container with a mouthpiece or mask at one end, and a hole for the inhaler in the other. A homemade spacer, made from a 500-ml plastic bottle, can be as effective as a commercially-manufactured inhaler.
Access to inhalers is a problem in many countries. In 2019, only half of people with asthma had access to a bronchodilator and less than one in five had access to a steroid inhaler in public primary health-care facilities in low-income countries .
Also Check: Army Eczema Waiver
Notch Signaling Regulates Mucous Cell Differentiation
Notch signaling is also important for mucous metaplasia . Notch is a transmembrane receptor that binds to cell-surface ligands in the Delta-like and Jagged families. Ligand binding activates -secretasemediated proteolytic cleavage and liberates the Notch intracellular domain, which enters the nucleus, associates with transcription factors, and drives expression of downstream Notch genes. Genetic manipulation of Notch signaling in mice has different effects depending on the developmental stage. In explanted embryonic lungs, addition of Notch ligand or expression of a constitutively active form of Notch increased MUC5AC-containing mucous cells, whereas a -secretase inhibitor reduced mucous cells . Notch-induced mucous metaplasia did not require STAT6 activation, suggesting that the Notch and STAT6 pathways may operate in parallel. In contrast, in postnatal mouse lung, disruptions of Notch signaling induced mucous metaplasia , a process that principally depends on the Notch ligand Jagged1 . The Notch target Hes1 appears to be critical for inhibition of mucous metaplasia and MUC5AC transcription, although inactivation of Hes1 was not sufficient to induce mucous metaplasia . The observation that a -secretase inhibitor reduced IL-13induced mucous metaplasia in cultured human airway epithelial cells suggests that further attention to the role of epithelial Notch signaling in asthma is warranted.
The Normal Respiratory System
To understand what happens in asthma you need to be familiar with the normal breathing system and how the lungs and airways are arranged.
Normally, air entering through the mouth and nose travels through the main airway through a series of smaller branching airways called bronchi. The bronchi divide up into even smaller airways called bronchioles, which end in millions of tiny air sacs called alveoli.
When air enters the alveoli, the oxygen it contains passes through the thin membrane covering each sac into surrounding blood vessels. The oxygen attaches itself to red blood cells which then circulate around the body, releasing the oxygen into the body tissues.
What happens during an asthma attack?
Also Check: Does Weight Gain Make Asthma Worse
Higher Risk Not Limited To Respiratory Conditions
Sure enough, Dr. Juhns research showed that children and adults with asthma have a much higher risk of developing shingles compared to patients who do not have asthma. These findings were replicated by other research groups. Similarly, adult asthma patients have a higher risk of developing community-acquired E. coli blood infection, rheumatoid arthritis, heart attack and diabetes. Children with asthma have higher risks of developing celiac disease and appendicitis compared to those without asthma.
The Secretory Pathway In Mucous Cells
ORMDL3, a member of the Orm family of transmembrane ER proteins, has also been implicated in asthma. Genetic polymorphisms at loci close to ORMDL3 were strongly associated with asthma in multiple genome-wide association studies . Allergen challenge induced ORMDL3 expression in airway epithelial cells in a STAT6-dependent fashion, although ORMDL3 does not appear to be a direct target of STAT6 . Studies involving overexpression or knockdown of ORDML3 in HEK293 cells indicate that ORMDL3 is involved in regulating ER stress responses and ER-mediated calcium signaling . In addition, Orm proteins form complexes with serine palmitoyl-CoA transferase , the first and rate-limiting enzyme in sphingolipid production, and may thereby help coordinate lipid metabolism in the secretory pathway . Genetic and pharmacologic reductions in SPT activity induced airway hyperresponsiveness in the absence of inflammation or mucous metaplasia . Further studies are required to determine whether ORMDL3s role in modulating sphingolipid production, ER stress, calcium signaling, or other ER functions in airway epithelial cells or other cells is important in asthma.
Also Check: Can You Join The Army If You Have Asthma
How Is It Diagnosed
If youve been diagnosed with asthma but dont seem to respond well to treatment, your doctor may suspect you have a less common subtype of asthma. Theyll likely evaluate your condition and look for additional signs or symptoms that can direct them toward a diagnosis.
In the case of EA, the easiest step is to check your levels of white blood cells. For this, your doctor will collect blood, sputum, or saliva and send it to a lab. High levels of eosinophils can affirm your doctors suspected diagnosis.
In addition to the blood test, however, your doctor may conduct a physical exam. Certain physical symptoms, such as nasal polyps, can confirm the suspected diagnosis. The combination of the blood test and the physical exam may be enough for your doctor to diagnose you.
1 in 12 people has asthma. As doctors now recognize that asthma is more than one condition, they realize that the subtypes need specific treatments. Individual treatments for each subtype can help you achieve the best outcome for the condition.
Traditional asthma treatment involves inhaled corticosteroids and a rescue inhaler. However, people with EA dont always respond well to inhaled corticosteroids. Higher doses may lose their impact too, requiring a switch to an entirely new treatment.
The most common treatments for EA include the following.
