Complications And Associated Conditions
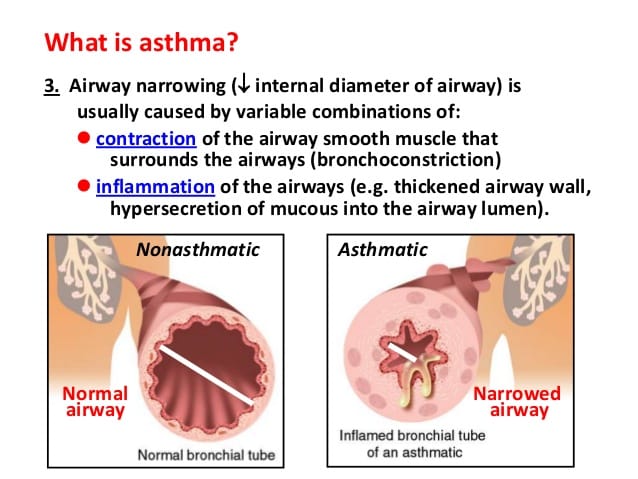
If left untreated, bronchoconstriction can become life-threatening. For this reason, its important to follow your doctors treatment and management plans.
Bronchoconstriction may also cause airway remodeling. Airway remodeling occurs when a condition like bronchoconstriction changes the pattern of your airways, thickens them, or increases the amount of mucus produced there. Airway remodeling is still being studied, so its causes arent clear. Its suggested such changes may be from the mechanical force of your bronchi constricting damaging tissue cells during repeated episodes of bronchoconstriction or other lung conditions.
Additional complications of EIB may include the following:
- not enjoying favorite activities due to poor performance
- avoiding exercise and missing the health benefits it provides
Some conditions that are associated with bronchoconstriction include:
- asthma
Specific Targeting Of Asm Cells
A strategy specifically targeting ASM cells should be developed to treat the abnormalities in asthmatic ASM cells. To date, no specific targeting of ASM cells in vivo has been performed. Whether specific targeting is possible and feasible remains to be answered. However, some possible techniques to target these cells are discussed in the current paper.
To specifically target ASM cells, strategies such as local delivery or using an ASM-specific promoter could be used. Local delivery with a bronchoscope or administration via an aerosol can specifically target some parts of the airways without systemic involvement and this would reduce unwanted side-effects. The SM22 promoter can perhaps be used to target genes specifically to ASM cells , . Post-transcriptional inhibition at the mRNA level can be accomplished using antisense oligonucleotides and small interfering RNAs ; these gene-silencing nucleic acids prevent the production of proteins from mRNA. For instance, application of siRNA against NF-B by transfection of airway epithelial cells reduced TNF–induced IL-6 and IL-8 release . Antisense oligonucleotides can be administered via an aerosol and have been shown to be distributed throughout the lung .
Asm Is Involved In Asthma Through Other Mechanisms
In addition to inflammatory mediators and growth factors, many emerging mechanisms have been reported to be involved in ASM and airway remodeling. For example, vitamin D has been shown to inhibit remodeling in;vitro and in;vivo . However, its mechanism involving airway ASM cells is still under investigation . Another emerging mechanism is thyroxine, which has been reported to enhance ASM proliferation , while low thyroxine levels cause airway developmental malformations . Some reports also suggest that insulin appears to enhance ASM proliferation and ECM formation . In addition, sphingolipids participate in airway inflammation, AHR, and remodeling. In particular, sphingosine-1-phosphate can promote ASM contractility and regulate inflammation and airway remodeling .
Read Also: Pediatric Spirometry Normal Values
Recombinant Mfge8 Reduces Mfge8/ And Wt Asm Contraction
We were next interested in defining the time at which Mfge8 was required for its effect on ASM contraction. To address this question, we incubated tracheal rings that had been treated with IL-13 for 12 h with rMfge8 for 1 h before measuring contraction. Incubation with rMfge8 for 1 h completely rescued enhanced contraction in Mfge8/ tracheal rings . These data indicate that the effect of Mfge8 on ASM does not require new protein synthesis and is unlikely to be the result of chronic structural changes in Mfge8/ ASM. We next examined whether longer incubation with rMfge8 would have a greater effect on reducing ASM contraction. A 12-h incubation of IL-13treated Mfge8/ tracheal rings with recombinant protein markedly reduced ASM contraction to untreated Mfge8/ levels whereas it had no effect on the force of untreated tracheal ring contraction . We also examined whether rMfge8 would decrease WT tracheal ring contraction. A 1-h incubation with rMfge8 significantly reduced, and 12 h incubation completely abrogated, the IL-13induced increase in contractility in WT tracheal rings treated with IL-13 .
Asthmatic Asm Cells: Is Ccaat
Recent studies point to a role for the transcription factor CCAAT-enhancer binding protein in the altered contractile, proliferative and secretory capacities in ASM cells from asthmatics. Asthmatic ASM cells in culture were shown to lack the anti-proliferative isoform of c/EBP , . This transcription factor may be important in many processes in ASM cells, including the contractility of ASM, as c/EBP is a possible negative regulator of MLCK expression , . Furthermore, it is thought that the lack of the anti-proliferative isoform of c/EBP in ASM cells from asthmatics results in the increase in ASM mass, as this transcription factor regulates proliferation through the regulation of the cell cycle inhibitor p21waf/cip1. In addition, steroids also exert their effect via c/EBP through an interaction of the glucocorticoid receptor and c/EBP that activates p21 . Due to the lack of c/EBP, these drugs are not very potent in inhibiting proliferation of ASM cells from asthmatics.
A recent review by Borger et al. describes the role of c/EBP in airway inflammation. In short, c/EBP can silence the inflammatory response through interference with nuclear factor -B-driven gene expression; a lack of c/EBP will result in more expression of NF-B-dependent inflammatory genes.
Recommended Reading: Asthma Help Without Inhaler
The Secretory Pathway In Mucous Cells
ORMDL3, a member of the Orm family of transmembrane ER proteins, has also been implicated in asthma. Genetic polymorphisms at loci close to ORMDL3 were strongly associated with asthma in multiple genome-wide association studies . Allergen challenge induced ORMDL3 expression in airway epithelial cells in a STAT6-dependent fashion, although ORMDL3 does not appear to be a direct target of STAT6 . Studies involving overexpression or knockdown of ORDML3 in HEK293 cells indicate that ORMDL3 is involved in regulating ER stress responses and ER-mediated calcium signaling . In addition, Orm proteins form complexes with serine palmitoyl-CoA transferase , the first and rate-limiting enzyme in sphingolipid production, and may thereby help coordinate lipid metabolism in the secretory pathway . Genetic and pharmacologic reductions in SPT activity induced airway hyperresponsiveness in the absence of inflammation or mucous metaplasia . Further studies are required to determine whether ORMDL3s role in modulating sphingolipid production, ER stress, calcium signaling, or other ER functions in airway epithelial cells or other cells is important in asthma.
Autonomic Innervation Of The Airways
It is well-established that in the GI tract there is parasympathetic innervation which exerts both excitatory and inhibitory control on the tone of the smooth muscle as well as sympathetic innervation that has a predominantly inhibitory effect during extra-uterine life . However, in the case of the human respiratory tract, sympathetic innervation is sparse and predominantly supplies blood vessels and submucosal glands. In contrast to humans, spinal adrenergic sympathetic nerves supply ASM in some mammals such as guinea pigs, cats and dogs . In humans it is the cranial parasympathetic nervous system that predominantly controls the ASM through extensive plexuses. The vagus nerve carries both cholinergic and non-adrenergic non-cholinergic nerves, activation of the former leading to constriction and the later to relaxation. Selective vagotomy results in loss of the normal rhythmic contraction of ASM and bronchodilation. Given the position of parasympathetic ganglia which are predominantly located along the trachea and large bronchi, it is possible the effect of thermoplasty may be on neuronal control of ASM.
Nitric oxide and vasoactive intestinal peptide act as the principle transmitters in the mammalian NANC parasympathetic bronchodilating system with the former predominating in humans . It appears that parasympathetic mediated relaxations of ASM requires higher frequency of stimulation than those needed to evoke parasympathetic cholinergic contractions .
Also Check: Does Asthma Make Chest Hurt
Viral Infection To Predisposition
The fact that early-in-life sensitization to multiple allergens carries the greatest risk for developing asthma brings the question of what factors result in a predisposition to this phenotype. Although infection with rhinovirus is the major cause of acute exacerbation, in those genetically at risk of asthma, rhinovirus-induced wheezing in the first three years in the life is also the greatest risk factor for developing asthma at 6 years of age . Impaired TLR3-mediated IFN- and – production by asthmatic epithelial cells would make susceptible to both viral infection and allergic sensitization . Reduced primary IFN production by lower-airway epithelial cells enables some viruses to replicate, leading to cytotoxic cell, release of inflammatory products and enhanced viral shedding. Such events provide a strong stimulus for recruitment of immature DCs and their priming for allergen sensitization . When asthmatic epithelial cells are received to damage by rhinovirus infection, the cells generate increased amounts of the pro-Th2 cytokine thymic stromal lympoietin , which stimulates DCs and increases allergic inflammation, whereas exogenous IFN-b applied to asthmatic epithelium exerts anti-Th2 as well as antiviral properties .
External Biomechanical Pressure On Airway Epithelium
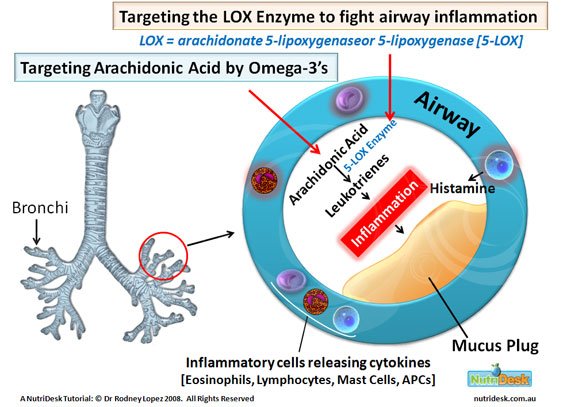
Airway inflammation that provokes the release of soluble mediators is commonly considered to be the cause of AR. Less commonly considered, but possibly no less important, is the effect of mechanical compression of the epithelial layer. Smooth muscle contraction creates stress forces on the 3-dimensional airway structure, including epithelial compression . The persistence of these forces are under-appreciated factors promoting ASM hypertrophy in asthma. Studies demonstrate the progression of asthmatic airway structural changes in the absence of inflammation, presumably due to airway compression.26
An acute asthma attack with enhanced ASM contraction not only causes airway constriction that reduces the airway luminal area beyond the normal contractile range, it creates mucosal folding of the airway epithelium which provokes intracellular responses that stimulate AR.27 In vitro models show that acutely compressed airway epithelial cells release factors that stimulate increased basal ASM contraction and proliferation, leading to a higher resting tone and a narrower resting airway lumen.28 For example, ASM constriction produces tension on integrin v5 fibers, this in turn activates TGF- which promotes ASM hyperreactivity and AR .29
Read Also: Is Asthma An Illness Or Disease
Is Loss Of Homeostasis And Hence Development Of Asthma Reflected In Bronchial Sensitivity And The Magnitude Of Airflow Obstruction And Hence Severity A Function Of The Reactivity
Bronchial Sensitivity
The observations that asthma can develop at any age and that many children outgrow their asthma, again suggests that sensitivity is not an absolute value and that it can be influenced by environmental factors, possibly via interactions with the host immune system and/ or epigenetic changes. Bronchial sensitivity appears to have two components; inherent baseline sensitivity and a more labile variable component. As with all physical and physiological traits there is likely to be a normal innate distribution of inherent sensitivity to constrictor stimuli. However, there is ample evidence that an individual’s bronchial sensitivity can vary over short periods of time, exemplified by the changes in sensitivity following the commencement and cessation of steroid therapy or the development of an inter-current respiratory viral illness. As noted above, this can affect bronchial sensitivity even in healthy individuals, though the effects are generally not marked. In those with an allergy, it can also be observed following a laboratory allergen challenge or during seasonal exposure to an allergen such as grass pollen. Conversely allergen avoidance such as moving to high altitude for house dust mite sensitive individuals appears to be associated with a reduction in sensitivity .
Bronchial Reactivity
Treating Asthma Means Treating Asm
Since ASM cells are the most important cells involved in AHR, and have been shown to be involved in remodelling and inflammation, the present authors propose that these cells should be targeted, rather than targeting inflammation or treating symptoms. As described previously, ASM cells cultured from biopsies from asthmatics show different characteristics in different studies. They can either be hypercontractile, hyperproliferative or hypersecretory. Several molecules are thought to be involved in these processes and could be targeted. Table1 lists some of these molecules and their functions. Possible interventions and known drugs are also identified.
Airway smooth muscle targets for therapy
Don’t Miss: Why Are Asthma And Eczema Related
Loss Of Effective Airways Smooth Muscle Homoeostasisthe Key To Understanding Asthma
As will be argued in more detail below, the fundamental defect leading to asthma appears to be a loss of the normal post-natal homeostatic control. Antenatally, ASM contracts vigorously and frequently with regular peristaltic waves moving distally from even in the earliest stages of lung development. This is vital for lung development but toward term these peristaltic waves cease. In contrast to it its marked physical contractions prenatally, post-natal ASM maintains a relatively constant length with relatively minor and non-coordinated oscillations around an optimal length, probably controlled by classic negative feedback loops. To date no clear role for ASM in a healthy individual after birth has been identified. The most likely role, if any, is likely to be helping to maintain an optimal luminal diameter in the conducting airways in order to minimize resistance to airflow while at the same time minimizing the dead space within the conducting airways.
The Same Indefinite Application Of The Term Still Remains In Vulgar Use
Depressingly, over- and under-diagnosis of asthma remains common . The lack of focus on objectively documenting the presence of the key component of asthma is one of the principle reasons for over diagnosis. Conversely a failure to recognize that the degree of bronchial reactivity follows a bell shaped distributed amongst asthmatics, with many having relatively mild constriction when triggered, results in under diagnosis at the milder end of the spectrum. Children with relatively mild asthma may not wheeze with intercurrent viral illnesses and present with coughing that takes many days or weeks to regress to the mean. Hence their symptoms are all too often dismissed as just another viral infection. Additionally, the ability of subjects to adjust to impaired lung function and thus minimize symptom reporting results in ongoing under-diagnosis. It is not rare to see an adolescent with an FEV1 of 54 and 40% reversibility who show no overt evidence of respiratory distress, are free of wheeze and who state they are fine and don’t know what the fuss is about.
In those with objective evidence of asthma, difficult asthma is almost always attributable to either
failure to deliver the ICS to the lungs or
having asthma and a co-morbidity such as those outlined above with symptoms caused by the co-morbidity being managed with ever escalating doses of medication .
Read Also: Does Asthma Make You Cough Constantly
Airway Smooth Muscle Hypercontractility In Asthma
Christopher Brightling
1Department of Infection, Inflammation and Immunity, Institute for Lung Health, University of Leicester, Leicester LE3 9QP, UK
Abstract
1. Introduction
Asthma is a chronic inflammatory disease characterized by variable airflow obstruction and bronchial hyperreactivity associated with airway remodelling . Most of asthma symptoms result from airflow obstruction caused by airway lumen narrowing. Although this narrowing is multifactorial in origin, abnormalities of airway smooth muscle structure and function have been identified as one of the main causes . Increased ASM mass has long been recognized as a major component of airway remodelling . More recently, asthmatic ASM was also found to be abnormal in its functional properties with increasing evidence showing intrinsic heightened contractility independent of other structural cells and independent of the asthma inflammatory milieu. In this paper we will examine the evidence of ASM hypercontractility in asthmatics, explore the potential mechanisms driving it, discuss its relevance, and briefly suggest its role in future asthma therapy.
2. Evidence of ASM Hypercontractility in Asthmatics
–
3. Potential Mechanisms Driving ASM Hypercontractility in Asthmatics
3.1. Physiology of Human ASM Contraction
3.2. Abnormalities of Contractile Proteins
3.3. Dysregulation of Calcium Homeostasis
3.4. Abnormal Calcium Sensitization
3.5. Increased Oxidative Stress Burden
3.6. SMAD3 and ORMDL3
6. Conclusion
Ciliated Cell Structure And Function In Asthma
In comparison with the extensive asthma literature regarding mucous cells, relatively few reports have focused on ciliated cells. One study of epithelial cell strips obtained by endobronchial brushing found decreased ciliary beat frequency and increases in abnormal ciliary beating patterns and ciliary ultrastructural defects in individuals with asthma compared with healthy controls . These abnormalities were more pronounced in severe asthma. Ciliary abnormalities were accompanied by increases in the numbers of dead cells and evidence of loss of epithelial structural integrity, which suggests that ciliary dysfunction may be a consequence of a generalized epithelial injury. In any case, these results suggest that ciliary dysfunction might be an important contributor to impaired mucociliary clearance in asthma.
Read Also: Can Asthma Patient Eat Eggs
Enhancing Healthcare Team Outcomes
Patient care is most successful when there are effective teamwork and coordination by physicians, nurses, pharmacists, and other health care professionals. Everyone, including the patients, needs to be aware of the possible adverse effects of muscarinic agonists. Physicians need to communicate goals, plans, and adverse effects with the patients and everyone involved in their care. Nurses will also need to b familiarize themselves with goals, treatment plans, and adverse effects to inform the physician when there is a noticeable change. Pharmacists can educate the patient on taking the drug, educating them on other possible drug-drug interactions, and keeping the prescriber informed if there are any issues. The patient also needs to notify the physician if adverse effects are developing. Through effective teamwork, managing the adverse effects of muscarinic agonists can be performed.
Article Details
Airway Smooth Muscle Cell Contraction
The main signaling pathway involved in ASM contraction is related to Ca2;+. The calcium pathways in ASM are induced by mediators acting mainly via G proteincoupled receptors . Phospholipase C beta1 cleaves phosphatidylinositol 4,5-bisphosphate into inositol 1,2-diacylglycerol and trisphosphate , which in turn stimulate the release of Ca2;+ from intracellular stores . In addition to IP3, Ca2;+ release is stimulated by the activation of the CD38/RYR3 pathway or others yet to be discovered. Also, Ca2;+ can flow across the cellular plasma membrane through ion channels .
Ca2;+ transfers the activation signal to myosin light chain kinase and RHOA. MYLK phosphorylates myosin light chain leading to ASM contraction, which is terminated by MLC phosphatase . RHOA activates Rho-associated coiled-coil-containing protein kinases 1 and 2 and the ROCKs directly phosphorylate and inactivate MCLP, allowing myosin phosphorylation to occur .
The reasons for ASM hypercontractility in patients with asthma remain unclear and are built on animal-based evidence. The proinflammatory cytokines IL-13, IL-1B, TNF, and IFNG, were shown to increase ASM contractility by facilitating CD38-mediated Ca2;+ release or RHOA expression .
M.S. Hazari, D.L. Costa, in, 2010
Also Check: How To Help Someone With Asthma
