What Are The Different Types Of Delivery Devices For Asthma Medicines
You take most asthma medicines by breathing them in using an inhaler or nebulizer. An inhaler or nebulizer allows the medicine to go directly to your lungs. But some asthma medicines are in pill form, infusion form, or injectable form.
Inhalers
There are four types of asthma inhaler devices that deliver medicine: metered dose inhalers , dry powder inhalers , breath actuated inhalers, and soft mist inhalers.
- Metered dose inhalers have medicine plus a propellant. The propellant sprays the medicine out of the inhaler in a short burst.
- Dry powder inhalers do not have a propellant and do not spray the medicine out of the inhaler. The medicine is released from the inhaler when you breathe it in.
- Breath actuated inhalers have a dry powder or aerosol medicine. The medicine does not spray out of the inhaler. The medicine is released from the inhaler when you breathe it in.
- Soft mist inhalers do not have propellant, but they do spray the medicine out of the inhaler. They create a cloud of medicine that sprays out softly.
Different types of asthma devices
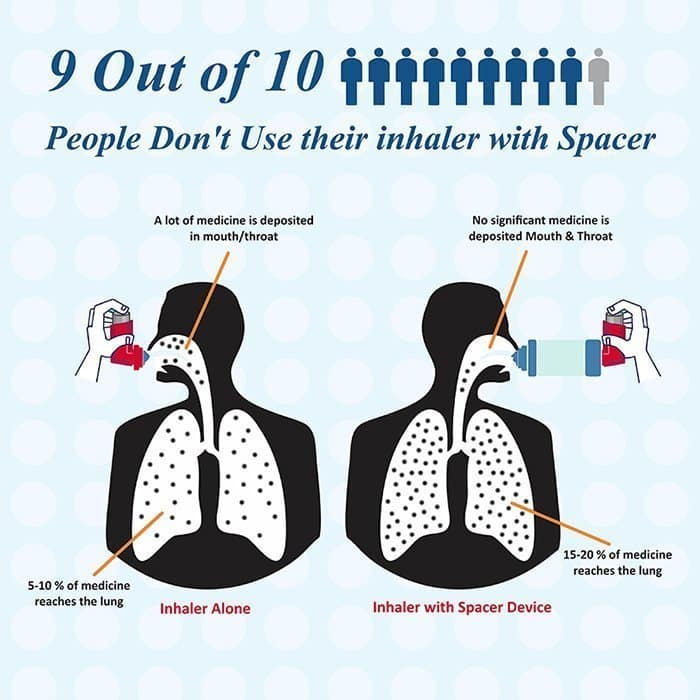
For inhalers to work well, you must use them correctly. But 70 to 90% of people who use inhalers make at least one mistake when using their inhaler.1 Inhaler mistakes can lead to uncontrolled asthma. Ask your doctor or nurse to watch you use your inhaler to make sure you are using it correctly.
Spacers and valved holding chambers
Nebulizers
Injectables
Determine If You Have A More Severe Form Of Asthma
If your asthma is uncontrolled or partially controlled despite taking high-dose inhaled steroids plus a second controller medication, or taking oral corticosteroids, you may have severe asthma, according to guidelines from the American Thoracic Society and European Respiratory Society. Severe asthma doesnt respond to standard treatments, but there may be other options for you.
For instance, nearly half of people with severe asthma have high levels of eosinophils in their lungs and blood, according to the NHLBI. These white blood cells can build up and cause inflammation and swelling in your airways, and today, medications called biologics can be prescribed to target those eosinophils. To diagnose eosinophilic asthma, your doctor will perform a blood test, a sputum induction test, or a bronchial biopsy to measure your level of eosinophils.
I Was Unprepared Get A Plan
Remember to follow advice you’ve been given for an attack everyone should have their own personal asthma plan.
I didnt realise how unprepared I was. Now I know how important it is to be prepared and informed. Im going to talk to my nurse about having my own and Ill keep a photo of it on my phone and send a photo to my husband, so well all know what to do if it happens again.
Don’t Miss: When To Take Child To Hospital For Asthma
How Is Asthma Diagnosed
Only your health care provider can tell if you have asthma. They will ask you questions about how you are feeling in general and also specific questions about your breathing. You will be asked about your past health, your familys health, about any medications you take, and if you have any allergies. Your health care provider will likely give you a physical exam and check your nose, listen to your lungs and heart, etc. to make sure you dont have any other problems. You might be asked to breathe into a tube that measures how much air your lungs can hold. If you are diagnosed with asthma you may be referred to a specialist.
Asthma: Action Plan And Getting Help
Posted under Health Guides. Updated 21 January 2021.
- Asthma affects how you feel and breathe.
- Asthma runs in families.
- Theres no cure for asthma, but it can be controlled.
An asthma action plan is a proactive way to keep your asthma under control. Its written with your health care provider and its personalized . An asthma plan has 3 zones green, yellow, and red.
- The green zone lists what medications you should take every day when you are feeling well.
- The yellow zone tells you what to do at the first sign of a cough, cold, or wheeze.
- The red zone tells you what to do if your Albuterol isnt helping, or if you are very short of breath.
The idea behind having a plan is having important information such as: steps you need to take to stay symptom-free, a list of your medicines the doses and how often you take them, your health care providers phone number, and a list of your asthma triggers, so you can have all these facts in one central location. You should have a copy of your Asthma Action Plan at home and with the nurse at school. You can also make a copy of your action plan and keep it with you. An asthma action plan also includes simple and clear instructions about how to identify early symptoms of an asthma flare-up, how to treat them, and when to go to the emergency room. You should feel comfortable talking with your HCP about your action plan and update it as things change.
You May Like: Best Places To Live For Asthma
Types Of Asthma Medicines
The following medicines are commonly used to treat asthma. It is important to follow your healthcare provider’s advice about your treatment.
Bronchodilators relax the muscles around the airways . When the airways are more open, it is easier to breathe. There are two general types of bronchodilators, and you may be prescribed one or both types:
- Short-Acting bronchodilators work quickly after you take them so that you feel relief from symptoms quickly.
- Long-Acting bronchodilators have effects that last a long time. They should not be used for quick relief. These medications are only recommended for use when combined with an anti-inflammatory asthma medicine .
Anti-inflammatory medicines reduce the swelling and mucus production inside the airways. When that inflammation is reduced, it is easier to breathe. These medicines also are called corticosteroids or steroids. Most often, these are inhaled medications and it is important to rinse out your mouth with water immediately after using them to avoid getting thrush, a yeast infection in your throat.
Some corticosteroids come in pill form and usually are used for short periods of time in special circumstances, such as when your symptoms are getting worse.
There are a few medicines that combine inhaled bronchodilators and inhaled corticosteroids.
Why Your Asthma Treatments Might Not Be Working For You
Managing a chronic pulmonary disease like asthma can be difficult and extremely stressful. Many things people take for granted can cause an asthma attack such as exercise, weather extremes, and environmental allergies. These can leave you feeling helpless if you have no way to control your exposure. Your best support for managing asthma can be medication. But what happens if it is not effective?
If you need to use a rescue inhaler more than twice a week this indicates that your asthma is severe or uncontrolled. There are a variety of ways to better support your pulmonary condition, but the first step is to find a medication that works best for your symptoms and your lifestyle.
If you are already on an asthma medication, ensure you are using the medication correctly and as prescribed by your healthcare team.
Recommended Reading: How To Treat Bronchial Asthma At Home
Video: Signs That Your Asthma Is Getting Worse
Transcript for Signs that your asthma is getting worse
0:00 Asthma attacks rarely happen out of the blue.
0:03 They often take a few days to build up.
0:07 Asthma is different for everybody.
0:10 By learning how to recognise when your asthma symptoms are getting worse,
0:14 itll help you to stay in control.
0:18 So, signs that your asthma is getting worse are variable.
0:23 The most common sort of signs are you may feel some wheezing,
0:26 you may have a cough, you may find a tightness in your chest.
0:32 If you keep a peak flow diary, you may find that your peak flow scores are reducing a bit.
0:38 You may also find that youre using your blue reliever inhaler more frequently than you usually would.
0:45 If your symptoms continue to be worse and youre using your blue inhaler a lot,
0:52 then please do call us on the helpline or contact us by email,
0:56 especially if youre not sure what to do next.
0:59 We can discuss whats been going on with you
1:01 and make a plan for a way forward.
1:05 If you are using your preventer inhaler as prescribed,
1:09 every day, even when youre well and using really good inhaler technique,
1:14 and despite this, your asthma symptoms are getting worse,
1:18 its a good idea to see your GP.
Related resources
Adult action plan
Using an asthma action plan will help you to stay well. Download and fill in with your GP.
Asthma Medication Not Working Try Another
People who supplement rescue inhalers with a second asthma medication sometimes get little relief at first, but theres good news: Those who keep trying different options often find a medication that works, according to Rutgers researchers.
The researchers analyzed data from 2,025 patients who used any of six FDA-approved severe asthma treatments known as biologics because they contain monoclonal antibodies found in living organisms.
The practical takeaway here is pretty simple: Patients who arent getting good relief from a particular biologic should try others, said lead author Reynold A. Panettieri Jr., vice chancellor for translational medicine and science director at the Rutgers Institute for Translational Medicine.
Overall, according to findings published in the Annals of Allergy, Asthma & Immunology, these injectable medications provided significant relief. Patients starting biologics during the study period experienced a 58 percent reduction in exacerbations, and 89 percent of those who used biologics at any point during the study period continued to do so at the end.
Some 324 patients switched medications at least once during the study period most commonly because their symptoms worsened on the first medication or because initially strong effects waned over time and their strategy was rewarded, the researchers found. Switching medications was consistently associated with a reduction in exacerbations.
Don’t Miss: Where To Buy Asthma Inhaler
Test For Airflow Obstruction And Inflammation
A variety of tests can help your doctor tailor your treatment to your specific asthma. For example, your doctor might ask you to breathe into a machine for a lung function test known as spirometry. You might then be asked to repeat the test, possibly after taking a puff from an inhaler, so that your doctor can compare results and check whether the inhaler helped improve your airflow.
Additional tests look for signs consistent with inflammation, in particular allergic inflammation, says Levy. These tests might include a peripheral blood eosinophil count, serum immunoglobulin E level, and exhaled nitric oxide level.
Preventing An Asthma Attack
The best way to prevent having an asthma attack is to make sure that your asthma is under control. People with asthma typically use two types of medication:
- Long-term. This involves medication that you take every day to control airway inflammation and prevent asthma attacks. These medications can include things like inhaled corticosteroids, leukotriene modifiers and long-acting bronchodilators.
- Quick-relief. This is rescue medication that you take for short-term relief of asthma symptoms. These medications are referred to as short-acting bronchodilators and work to open your airways.
You should also work with your doctor to develop a personalized asthma action plan. This can help you to better understand and control your asthma. An asthma action plan includes:
- your asthma triggers and how to avoid them
- how and when to take your medications, both for symptom control and for quick relief
- indicators of when youre controlling your asthma well and when you need to seek emergency medical attention
Your family and those close to you should have a copy of your asthma action plan so that theyll know what to do if you have an asthma attack. Additionally, it may be helpful to keep it on your phone as well, in case you need to reference it quickly.
Its possible that you may still have some questions regarding asthma attacks. Well try to answer some of these now.
Recommended Reading: How To Help Asthma In Toddlers
A Word About Summer Breaks From Asthma Medicines
Asthma is a chronic yet variable disease everyones asthma is different. Asthma attacks or flare-ups are more common the spring and fall so children with asthma need to take their asthma medicines year round â even in the summer . Control or preventive medicines keep airways from swelling due to exposure to allergens, irritants or respiratory illnesses but they can take weeks to be fully effective again. Stopping controller medicines in the summer allows the airways to lose their protective armor against triggers. It can take weeks before the protection is gone but it also can take up to 3 months of daily use to get that protection back.
Because children returning to school are more likely to be exposed to the flu and colds, it creates a much greater risk that their asthma will flare up resulting in extra visits to a providers office or the ER and missed school days. Remember, summer break doesnt apply to asthma medicines.
2Biologics for Asthma: Attacking the Source of the disease, not the symptoms, American College of Allergy, Asthma & Immunology
What Is A Bronchodilator

A bronchodilator is a type of medication that relieves the symptoms of asthma, chronic obstructive pulmonary disease and other lung conditions. It quickly relaxes the muscle bands that tighten around your airways . When those muscles relax, more air comes in and out of your lungs so you can breathe comfortably.
Bronchodilators also help clear mucus from your lungs. As your airways open, mucus moves more freely, which allows you to cough mucus out of your body easily.
Bronchodilators are primarily available as inhalers and nebulizer solutions.
Read Also: How Often Can You Use An Inhaler For Asthma
When Should I See My Healthcare Provider
Talk to your healthcare provider if you have any symptoms that affect your lungs. Symptoms may include difficulty breathing, coughing or wheezing. They can order pulmonary function testing . Lung function tests help diagnose a lung condition that a bronchodilator may treat.
Its also a good idea to talk to your healthcare provider if you need to use SABAs more than twice per week. Using SABAs more than twice a week is a sign of unstable asthma. Your healthcare provider may wish to change the dose of any long-term control medicines that you take.
A note from Cleveland Clinic
Lung conditions such as asthma and chronic obstructive pulmonary disease affect your airways. Bronchodilators are medications that can help you control the symptoms of a lung condition.
Always follow your healthcare providers medication plan. If your bronchodilators arent controlling your symptoms, reach out to your healthcare provider right away. They can answer your questions, address any concerns and find the right care plan for you.
Last reviewed by a Cleveland Clinic medical professional on 08/09/2022.
References
Your Gp Or Asthma Nurse Can Help Your Asthma Symptoms
Theres a lot your GP or asthma nurse can do to help stop symptoms building up to an asthma attack. Book an appointment now to get the support you need to lower your risk.
Your GP/asthma nurse can:
- Talk to you about why your asthma symptoms have got worse
- Check youre taking your preventer medicine every day. If you havent been taking it regularly, they can suggest ways to get into a good routine with it so its easier to remember.
- Look at your inhaler technique to make sure youre getting the medicine you need
- Suggest a higher dose, or more puffs, of your preventer inhaler for a while
Don’t Miss: How To Use Asthma Pump Properly
Will Medicine Help Me Breathe Better When I Exercise
Yes. Exercising, particularly in cold air, may cause airway swelling or exercise-induced bronchoconstriction . Quick-relief asthma medicines, taken before exercise, usually control this. If you need repeated doses of quick-relief medicine during and after exercise talk with your doctor. Your medicines may need to be adjusted. Thanks to these medicines, many Olympic and professional athletes have successful sports careers even with their asthma.
It is important for everyone, including people with asthma, to be as active as possible for good health. Talk with your doctor about how you can be physically active while keeping your asthma well-controlled.
Addressing Nonpharmacologic Aspects Of Care
As outlined in previous Canadian consensus guidelines for the management of asthma,15 it is essential that all patients receive appropriate asthma education. Surveys of Canadians with asthma have revealed that many lack a rudimentary understanding of their medications and often confuse reliever medications with preventive medications.13 Furthermore, few have seen a certified asthma educator, and the vast majority do not have written action plans to guide management of exacerbations.14 Most rely on physicians or pharmacists to answer their questions about asthma, but the time and resources available for such counselling are often limited.13 Many patients have poor inhaler technique and hence fail to achieve control of their disease.18 Comprehensive education must include not only information about appropriate use of medications, but also the teaching and assessment of optimal inhaler technique. Even the simple-to-use dry powder inhalers can be mishandled. In addition, it is important to evaluate whether environmental factors in patients homes or workplaces may be worsening their asthma symptoms.
You May Like: Where Does Asthma Come From
Understand Your Asthma Medication
There are a variety of medicines available to treat asthma, but there is no “best” medicine for all people. Each person’s asthma is different, and your healthcare provider and healthcare team can work with you to set up the best plan for you based on your symptoms and needs.
- Do more of the things you want to do
- Have fewer asthma symptoms
People with asthma are often treated with a combination of quick-relief and long-term controller medicines.
Quick-Relief Medicine works quickly to relax your airways and help you breathe easier.
- You need to take this medicine if your asthma symptoms get worse.
- Be sure to start treatment as soon as your symptoms begin.
Long-Term Control Medicine reduces the swelling and inflammation in your airways and prevents symptoms
- You need to take these medicines every day, even when you feel well.
