Effective Management Of Adult Patients With Asthma
Therese Marie Bidder Clinical nurse specialist, Department of Specialist Allergy and Clinical Immunology, Royal National Throat, Nose and Ear Hospital, University College London Hospitals NHS Foundation Trust, London, England
Why you should read this article:
-
To enhance your understanding of the signs and symptoms of asthma and how the condition is diagnosed
-
To be aware of the treatments available that can achieve asthma control and reduce the risk of acute exacerbations of asthma
-
To count towards revalidation as part of your 35 hours of CPD, or you may wish to write a reflective account
-
To contribute towards your professional development and local registration renewal requirements
Asthma is a chronic respiratory condition that can affect people of all ages. Globally, asthma is one of the most common non-communicable diseases and is associated with significant personal, financial and societal costs. In some cases, asthma can be fatal, although many fatalities would have been preventable with appropriate management. People with asthma often underestimate the effects of their symptoms, and nurses should develop their knowledge and skills so that they can provide appropriate management advice. This article outlines the causes of asthma and its symptoms. It also explains the interventions used in the management of this condition, including medicines, patient education, appropriate lifestyle changes and referral to specialist services.
Peer reviewCorrespondence
Lessons Learnt: The Unique Challenges Of Implementing Qi In The Ed
It has been said that changing the behaviour of physicians is as difficult as that of patients, and merely informing physicians of the benefits and standards of care alone is unlikely to reach sustained adherence. This is particularly true in the ED setting, where organisational and cultural factors feature prominently in hindering QI. Despite various attempts to improve the quality of asthma care in EDs around the world, enduring challenges are likely to remain due to the high-paced and unpredictable nature of the emergency care. ED physicians are frequently under the competing pressures of heavy workloads and overcrowding, frequent interruptions at work, and the need to multitask, and many experience occupational stress and burnout. In addition, the exigencies of attending to the medical emergencies may contribute to reduced emphasis and prioritisation of resources on good holistic asthma care.
In our ED, junior ED physicians are often ultimately responsible for making the referral to the A-CARE nurse, issuing medication prescriptions and arranging for outpatient follow-up after discharge from the ED. Although A-CARE received broad support from senior ED physician leaders in our hospital, we were unsuccessful in engaging junior ED physicians and this was perhaps the most important factor underlying the low referral rate to the A-CARE nurse.
What Happens During An Asthma Attack
In Asthma, three processes occur. First is a hypersensitivity of the bronchial passages. Second is inflammation of the airway passages. Lastly is airway obstruction. Together, this produces an asthma attack. The patient will not be able to breathe properly.
Hypersensitivity occurs due to an exaggerated response from a variety of stimuli. This could be an allergic reaction, emotional response or a hormonal change . Inflammatory mediators or chemical substances are released such as histamines, prostaglandins, and leukotrienes as well as neutrophils, eosinophils and lymphocytes. The result is narrowing of the bronchial passages mucous is produced as well as inflammation in the trachea, bronchi, and the bronchioles. Additionally, the smooth muscles in the bronchial system spasm, and there is a thickening of the walls in the airway. The narrowed airway makes it difficult to breathe in air . Receptors in the lungs trigger hyperventilation or attempts at rapid breathing. The exchange of air and oxygen in the alveoli becomes erratic. Hypoxemia or low oxygen level in the blood occurs, and carbon dioxide levels rise as it can no longer escape through exhaling. If the asthma attack continues without treatment respiratory failure can occur .
Read Also: What Is The Best Treatment For Exercise Induced Asthma
Assessment And Diagnostic Findings
To determine the diagnosis of asthma, the clinician must determine that episodic symptoms of airway obstruction are present.
- Positive family history. Asthma is a hereditary disease, and can be possibly acquired by any member of the family who has asthma within their clan.
- Environmental factors. Seasonal changes, high pollen counts, mold, pet dander, climate changes, and air pollution are primarily associated with asthma.
- Comorbid conditions. Comorbid conditions that may accompany asthma may include gastroeasophageal reflux, drug-induced asthma, and allergic broncopulmonary aspergillosis.
A Stepwise Management Approach
There is no National Institute for Health and Care Excellence guidance for asthma management. However, a quality standard outlines 11 high-priority areas for quality improvement linked to British Thoracic Society and Scottish Intercollegiate Guidelines Network guidance on asthma management .
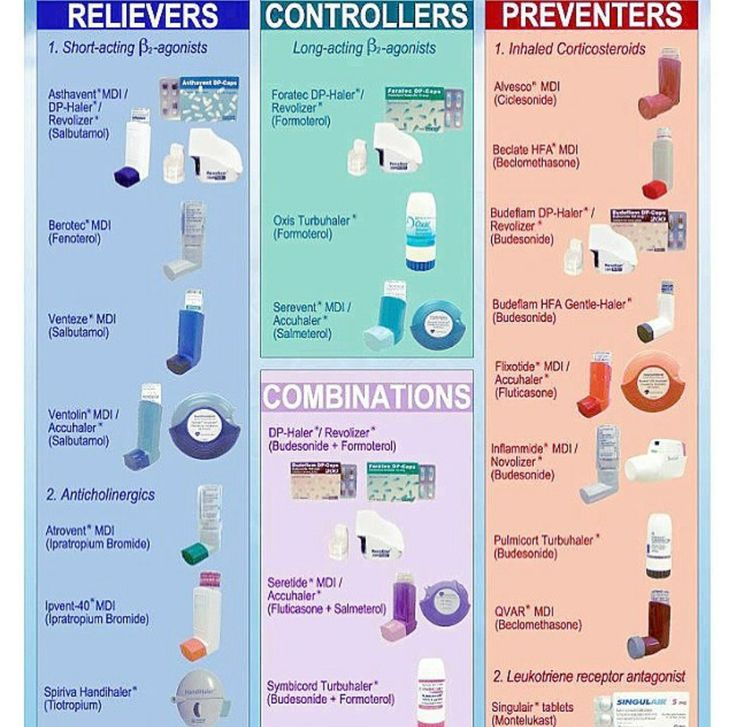
In most patients, asthma is effectively managed with inhaled corticosteroids and inhaled ß2-agonists according to steps 1-3 of the BTS/SIGN stepwise management plan . However, a minority of patients have poorly controlled asthma despite the prescription of optimal inhaled medication. These patients require additional maintenance therapies such as leukotriene receptor antagonists, sustained-release theophylline, oral ß2 agonists, or intermittent or regular oral corticosteroids . All patients at step 4 or 5 require referral to specialist asthma services for assessment and evaluation of their suitability for individualised therapy .
Read Also: How Do You Get Tested For Asthma
No Matter What Questions You Have About Your Asthma Youve Got A Team Behind You That Can Help
Health advice > Asthma care in the NHS
Your healthcare team is made up of professionals such as GPs, asthma nurses, pharmacists and specialists. They may be based in the community and in hospitals. This will be different for everyone because of where you live, your age, and your individual asthma needs.
Theres a lot of research that shows that if you know who to ask when you have a question, youll feel more confident about managing your asthma in between appointments.
Most people with asthma usually only need to see their GP or asthma nurse. If youre caring for a child with asthma, or if your symptoms are more unpredictable and harder to manage, you may need extra help from healthcare professionals with other areas of knowledge.
Healthcare professionals who can help you with your asthma
Helping The Patient With Asthma
The main goal is to prevent asthma attacks and minimize risks. Identify any environmental triggers such as dust, pollen or insects. Molds, pets, and even foods can also trigger an attack. Once triggers have been identified, a plan can be developed with the patient to avoid the triggers and how to handle an attack when it occurs. A plan should include teaching the patient to recognize signs and symptoms of an attack, how to use the medication provided, what triggers to avoid and when to seek medical attention . It is also a good idea to ask the patient to keep a journal of when their attacks occur and what medications worked best. This will help with the treatment plan.
One of the goals of patient care is teaching the patient to recognize early symptoms or worsening symptoms . The care giver should also make sure that the patient understands how to properly use all medications including inhalers and oxygen. Typically, the patient will have a long-term medication such as an inhaler to reduce inflammation which is taken daily. However, they can also have quick-relief medication that is used during asthma attacks. The quick-relief medication relaxes the muscle of the airway, relieving symptoms. The patient should also know when to contact emergency services for help when needed.
Recognize when the asthma attack is getting worse. Signs include :
You May Like: What Happens If You Use An Inhaler Without Asthma
The Vital Role Of The School Nurse In Managing Asthma
- Carl O. Helvie R.N., Dr.P.H.Advanced Practice Nursing in the Community1998
- Supporting Childrenâs Health and Wellbeing2017
- SAGE KnowledgeBook chapter Schools and the Health of Children: Protecting Our Future2000
- Paul C. McCabe and more…Pediatric Disorders: Current Topics and Interventions for Educators2010
- Robert F. Rich and more…Encyclopedia of Health Services Research2009
- Encyclopedia of Lifestyle Medicine & Health2012
- Paul C. McCabe and more…Psychiatric Disorders: Current Topics and Interventions for Educators2010
- Schools and the Health of Children: Protecting Our Future2000
How Specialist Services Work
Specialist asthma services provide detailed, complex evaluations of patients with severe asthma using a systematic approach, thereby ensuring patients receive an appropriate diagnosis, support and access to specialist treatments . Although each specialist service has its own locally defined pathway, all services are commissioned under a standard NHS contract to ensure comparable patient care, and all adopt a multidisciplinary approach.
Teams are composed of at least two severe asthma respiratory consultants, severe asthma nurse specialists, dietitians, physiotherapists, allergy specialists and clinical psychologists , and may include pharmacists and speech therapists. The multidisciplinary team evaluates newly referred patients to define their asthma phenotype , as well as the most appropriate individualised treatment plan.
Patients managed by specialist severe asthma services show improved outcomes, including a decreased steroid burden, fewer hospital admissions and improved QoL . The benefits for patients cannot be overestimated to see the life-changing impact of this care on one patient.
Respiratory nurse specialists play a central role in specialist asthma services, carrying out initial and follow-up assessments, acting as patient advocates, providing continuity of care and ensuring a holistic approach to management.
Don’t Miss: How To Make An Asthma Action Plan
Nhs Stop Smoking Services
Who are they and what do they do?
The NHS stop smoking services has a national network of advisers who are trained to help you quit smoking.
The advisers provide advice on how to stop smoking. They can also give you professional support during the first few weeks after youve stopped.
When should you see them?
If you need advice or support to help you stop smoking, the NHS stop smoking services can help.
How do you access them?
Your GP can refer you, or you can phone your local NHS stop smoking service to make an appointment with an adviser. If there isnt a service in your area, your pharmacist may be able to advise you instead.
England
Wales
Northern Ireland
And not forgetting you!
The good news is that alongside your healthcare team, you have the power to make a big difference to how well you or your child feels. From taking your preventer medicines every day as prescribed to making sure you go for a regular asthma review there are plenty of things you can do to help manage your asthma.
Working with your healthcare team
Here are our top tips to help you make the most of your healthcare teams expertise.
Next review due August 2022
What Are The Sign And Symptoms Of Asthma
Asthma symptoms can be very different from person to person and from the type of asthma. Some symptoms may only be irritating while other symptoms can be life threatening. It is important to keep in mind that symptoms should be treated as soon as they appear. Symptoms most seen are coughing, wheezing, and dyspnea. A cough can be either dry or have mucus production. A chronic cough should be reported to the nurse for possible asthma assessment. Wheezing, on the other hand, is caused by the constriction of the bronchioles. Wheezes are sometimes heard with or without a stethoscope. Dyspnea is shortness of breath. The patient may also complain of chest tightness and anxiety from not being able to breath properly.
Asthma is classified according to severity . In adults and children, the classifications include intermittent, mild, moderate, and severe. The classifications range from two attacks per week to several times a day. This includes nighttime awakenings, interference with daily activities and use of medications. The classifications should direct care and help in developing a long-term management plan.
Sleep disturbances can also be an issue with a patient who has asthma . There is some research that indicates those with asthma can contribute to the development of sleep apnea. Remember that although these symptoms are part of asthma, they may also be present in other disease states. It is important to collect subjective and objective data to report to the nurse.
Recommended Reading: Southwest Allergy And Asthma Center
Asthma Nurse Asthma Nurse Specialist Or Practice Nurse
Who are they and what do they do?
Some GP surgeries have a dedicated asthma nurse who has had specialist training in the treatment and management of asthma.
In some surgeries where there is no dedicated asthma nurse, the practice nurse may see people with asthma instead.
When should you see them?
Your asthma nurse can help support you so you can look after your asthma better by:
- Making sure youre taking the right medicines
- Going through your written asthma action plan with you
- Carrying out your regular asthma review with you
- Answering any questions you may have about your asthma.
How to access them
Ask your GP or GP receptionist about what asthma nurse support is available to you and how best to access it.
How Can A School Nurse Help Your Child With Asthma
School nurses play a vital role in creating asthma-friendly schools. Registered professional school nurses provide professional healthcare services that no other school staff members are equipped to offer.
You can help your child to manage asthma at school by talking with the school nurse at or prior to the beginning of the school year in August. Share your childs medical history and bring medications such as a rescue inhaler to the school along with a prescription from your healthcare professional.
The school nurse will need to know what your childs triggers are, as well as your childs signs and symptoms of asthma. If you know that a particular trigger may be present in the school environment on a permanent or temporary basis , the school nurse will work with you to develop a plan to assist your child.
Your school nurse can help you to decide whether your childs inhaler or emergency medications should be kept and administered by an adult or whether your child is ready to self-carry and self-medicate, in which case, you will receive a form to be signed by you and your healthcare professional.
Always inform the school nurse of any major changes in your childs condition. The school nurse is available to answer your questions and discuss your concerns.
The registered professional school nurse is also prepared to:
Sue Buswell, MSN, RN, NCSNRetired School Nurse – Helena
Recommended Reading: Is Mold Bad For Asthma
The School Nurse Role In Asthma Management: Can The Action Plan Help
- Carl O. Helvie R.N., Dr.P.H.Advanced Practice Nursing in the Community1998
- Schools and the Health of Children: Protecting Our Future2000
- Cailee E. Welch Bacon and more…SAGE Research Methods Cases
- Paul C. McCabe and more…Psychiatric Disorders: Current Topics and Interventions for Educators2010
- Health Psychology in Nursing Practice2016
- SAGE KnowledgeBook chapter Schools and the Health of Children: Protecting Our Future2000
- SAGE KnowledgeBook chapter Schools and the Health of Children: Protecting Our Future2000
Promoting Asthma Control In Children
Purchase hardcopyAbout this Guideline
This best practice guideline focuses on assisting nurses working in diverse practice settings in providing basic asthma care for children and their families.
The goal of this document is to promote asthma control in children, from infancy through to 18 years of age.
Nurses, working in partnership with the multidisciplinary health care team, have an important role in promoting the control of asthma in children through key interventions of assessment, education and referral across diverse contexts and settings. This guideline focuses on children who have a diagnosis of asthma along with their families, and includes recommendations for developmentally appropriate assessment, management, education, referral and follow-up. For simplicity throughout the document, the word child or children will be used to refer to individual from birth to 18 years of age. For individuals 18 years of age and older, refer to the RNAO nursing best practice guideline Adult Asthma Care Guidelines for Nurses: Promoting Control of Asthma .
Supplement: 2008
Don’t Miss: What Is The Best Treatment For Allergic Asthma
Managing Asthma In Primary Care
Since asthma is a lifelong condition, effective self-management is essential. Practice nurses play an important role in evaluating and systematically reviewing how well patients manage their condition. Box 1 features a checklist to help practice nurses identify patients who may have difficulties in achieving adequate asthma management. If areas of concern are identified, various measures can be put in place :
- Stepping up medication
- Helping patients with their inhaler technique
- Helping patients avoid asthma triggers by giving support and advice, including on smoking cessation
- Following up patients who do not attend appointments
- Increasing the frequency of reviews
- Working in partnership with patients to develop a personalised asthma action plan.
Box 1. How well do your patient manage their asthma?
Nurses may encounter patients who meet the criteria for a referral to specialist services . Referring patients does not imply that primary care has failed them indeed, it is consistent with the requirement for nurses to make a timely and appropriate referral to another practitioner when it is in the best interests of the individual needing any action, care or treatment .
Box 2. Which patients need a referral to specialist services?
A positive answer to one or more of the following questions should trigger a referral to specialist severe asthma services:
Pearls And Other Issues
Disposition
If the patient requires nebulized salbutamol and is not ordinarily on home nebulizers, he or she should be admitted. Anyone who has presented with severe or life-threatening asthma should usually be monitored to ensure that the disease does not return when the medication has worn off.
Pitfalls
Issues include forgetting to remove the nebulizer mask once the nebulizer is done , not assessing inhaler technique, and neglecting to stress the importance of maintenance therapy with inhaled steroids even when the patient is well.
Recommended Reading: Can Asthma Cause Dry Mouth
School Nurses’ Available Education To Manage Children With Asthma At Schools: A Scoping Review
Research on asthma education programs available to school nurses is limited.
-
Existing programs lack consistency in strategies, assessments, and evaluation methods.
-
Nurses’ challenges regarding receiving continuing education must be considered.
-
Use of technology will further remove barriers to continuing education.
-
School nurse interventions improve the health and well-being of children with asthma.
