Personal Asthma Action Plan
As part of your initial assessment, you should be encouraged to draw up a personal asthma action plan with your GP or asthma nurse.
If youve been admitted to hospital because of an asthma attack, you should be offered an action plan before you go home.
The action plan should include information about your asthma medicines, and will help you recognise when your symptoms are getting worse and what steps to take. You should also be given information about what to do if you have an asthma attack.
Your personal asthma action plan should be reviewed with your GP or asthma nurse at least once a year, or more frequently if your symptoms are severe.
As part of your asthma plan, you may be given a peak flow meter. This will give you another way of monitoring your asthma, rather than relying only on symptoms, so you can recognise deterioration earlier and take appropriate steps.
Want to know more?
What Are The Typical Symptoms Of A Severe Attack Of Asthma
First, well mention what the typical symptoms of an asthma attack are. These symptoms can go from mild to severe, depending on the patient. Also, your symptoms can progress and become more powerful or more frequent over time. The most common asthma symptoms include:;
- Coughing: More common at night due to temperature change. Asthma cough commonly comes with sputum as a result of increased mucus in the airway.;
- Wheezing: A high-pitched whistling sound that appears when you breathe. Occurs because of the passing of air through a closed airway.;
- Chest tightness or pressure: Resulting from the contraction of bronchi muscle and extra effort to breath.
- Shortness of breath.
- Feeling tired or even weak: Especially while exercising.;
- Alterations in lung function: Only can be measured with a peak flow meter.
- Difficulty sleeping or nocturnal asthma.
- Other respiratory symptoms: Like runny nose and sore throat, indicating a possible viral infection.
Now, you start to imagine what a severe asthma attack can look like. During a severe attack, asthma patients can experience:;
- Severe wheezing.
- Use of accessory muscles: Showing as tightened neck and chest muscles.;
- Blue lips or nails.
Common Terms Found In Medical Record Related To Asthma:
Asthma exacerbation: It is nothing but an acute increase of symptoms in a person with asthma. This can be coded only with the Physician diagnosis.
Status asthmatics : Another term for this is severe asthma exacerbation. It is considered as severe as this may lead to even respiratory failure due to hypoxemia. As soon as a patient comes to emergency room with asthma symptoms, physician treats initially with medicines such as bronchodilators. If patient has status asthmatics they do not respond to these medicines.
Inhaler : Medicine filled inhalers are given to patient to use comfortably at any place when symptoms occurs suddenly.
Nebulizer : Electricity powered machine filled with liquid medication which turns to mist and the patient breath in.
Nasal spray : A bottle with liquid medicine made with the ease of spraying to nose.
PFT : Pulmonary Function Test, use to check the lung function by measuring lung volume, capacity, rates of flow and gas exchange.
You May Like: Does Elderberry Help With Asthma
What Is Our Conclusion
To be honest, there really is no conclusion here. In fact, what I just described is just the beginning, at least as far as what researchers are learning about our disease. In upcoming posts, I will delve a little deeper into this subject, and perhaps even show you how this information should lead to better asthma medicine — perhaps even an eventual cure. So, stay tuned!
Asthma: A Surprisingly Silent Disease
Asthma is known for its obvious and noisy symptoms: wheezing, gasping, and coughing. But experts say that the typical impression of asthma is not always correct.
Asthma can sometimes be a silent disease, says Bernstein. People can walk around with very serious asthma, with significant blockages of their airways, and not show any symptoms.
Windom agrees. The severity of asthma symptoms really may not reflect the severity of the underlying disease, he says. Even if you feel fine, your asthma may still be damaging your airways and you may be closer to a serious attack than you realize.
Even if you do have symptoms, you may not have an accurate impression of how much they affect you.
Theres no question that people with asthma tend to think they have much better control over their condition than they actually do, Edelman tells WebMD.
In a 2005 poll of over 4,500 adults with asthma in the U.S. sponsored by the Asthma and Allergy Foundation, 88% said that their condition was under control. But experts question their optimistic judgment. About 48% said that their symptoms disturbed their sleep. And 50% said that asthma has made them give up in the middle of a workout. Those are severe symptoms for people who supposedly have their condition under control.
While many adults have trouble assessing their own asthma, its a special problem for children. They may not remember life without symptoms.
Don’t Miss: How To Prevent Asthma Attacks
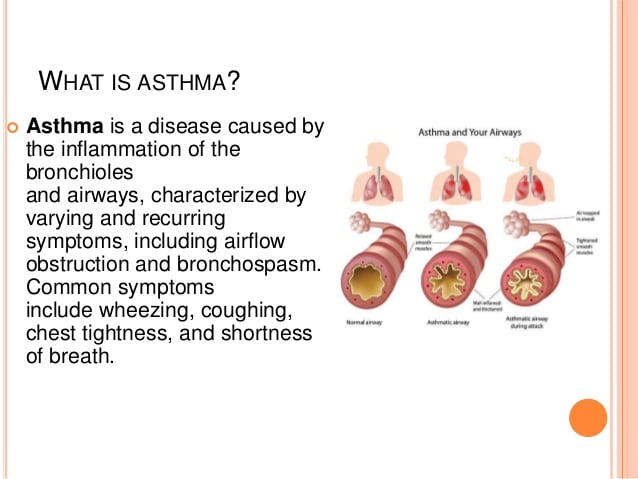
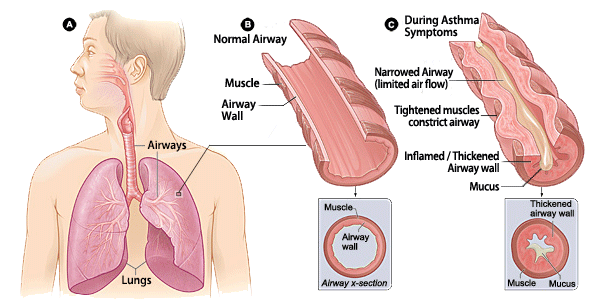
What Happens To The Lungs In Asthma
Asthma is a condition in which the airways of the lungs become either narrowed or completely blocked, obstructing normal breathing. This obstruction of the lungs, however, is reversible, either spontaneously or with medication . That is why asthma is technically called Reversible Obstructive Airway Disease . The basic abnormality causing asthma is the hyper responsive reaction of the body to specific and non-specific stimuli.
Air reaches the lung through the windpipe , which divides into two large tubes , one for each lung. Each bronchi further divides into many little tubes , which eventually lead to tiny air sacs , in which oxygen from the air is transferred to the bloodstream, and carbon dioxide from the bloodstream is transferred to the air.
Although the airways normally have the potential for constricting in response to allergens or irritants, the asthmatics airways are more prone to constriction due to increased response to allergens. This insult makes the airways more prone to infection leading to inflammation and swelling causing further constriction of the pipes. Infection also causes increased mucus production and this clogs the narrowed airways.
Once the airways have become obstructed, it takes more effort to force air through them and breathing becomes labored. This forcing of air through constricted airways can make a whistling sound, called wheezing. Irritation of the airways by excessive mucus may also provoke coughing.
Hypoxemia Hypercapnia And Lactic Acidosis
Intrapulmonary shunt appears to be practically absent in the majority of patients because of the collateral ventilation, the effectiveness of the hypoxic pulmonary vasoconstriction, and the fact that the airway obstruction can never be functionally complete . Hypoxemia is therefore common in every asthmatic crisis of some severity; mild hypoxia is easily corrected with the administration of relatively low concentrations of supplemental oxygen . More severe hypoxemia and the need for higher concentrations of supplemental oxygen may relate to some contribution of shunt physiology.
Analysis of arterial blood gases is important in the management of patients with acute, severe asthma, but it is not predictive of outcome. In the early stages of acute, severe asthma, analysis of arterial blood gases usually reveals mild hypoxemia, hypocapnia and respiratory alkalosis. If the deterioration in the patient’s clinical status lasts for a few days there may be some compensatory renal bicarbonate secretion, which manifests as a non-anion-gap metabolic acidosis. As the severity of airflow obstruction increases, arterial carbon dioxide first normalizes and subsequently increases because of patient’s exhaustion, inadequate alveolar ventilation and/or an increase in physiologic death space.
Recommended Reading: Does Medicare Cover Asthma Inhalers
Asthma And Your Respiratory System
When youve been diagnosed with asthma, the lining of your airways tends to always be hypersensitive meaning that theyre often inflamed and red. This means that patients may have flare-ups after exercising, being outdoors in cold weather, being sick, or having an allergy attack.
However, when exposed to an allergen, your bodys response is to trigger an asthma attack to protect you from potential harm. When your bodys immune system is triggered, your airways will swell even more in an attempt to block out the allergen. The muscles that surround your airways will also tighten, which is what makes it harder to breathe. Its common for many patients to have a secondary asthma flare-up after their initial asthma attack.
How Smoking Affects The Alveoli
Smoking is an important risk factor for lung disease. Tobacco smoke affects the respiratory tract at every level. This includes the alveoli.
Cigarette smoke affects how the alveoli work. Smoke causes damage down to the molecular level. It disrupts your bodys ability to repair itself after an infection or trauma. If exposure to smoke continues, alveolar damage continues to worsen.
You May Like: How To Help Someone With Asthma
Anatomy Of An Asthma Attack
When the respiratory system is working properly, the air we breathe passes in and out of the lungs through a network of airways.
But for people with asthma, even a minor irritant will set off an immune response that can shut down the airways.
Asthmatic symptoms are usually quite variable, someone with asthma may go for periods of time without symptoms, and then suddenly have severe episodes for days at a time. The most common symptom is wheezing.
Routine treatment for asthma includes inhaled bronchodilators, injected epinephrine , or intravenous theophylline.
Bronchodilators are drugs which open up or dilate the constricted airways.
Taking anti-inflammatory drugs, aimed at reducing asthma is a relatively new approach to treating asthma. The idea behind it is that if the underlying inflammation of the airways is reduced, the bronchi may become less hyperactive, making future attacks less likely.
For asthma which is strongly triggered by allergies, allergen avoidance can often greatly reduce the amount of medication needed to control the asthma. Taking anti-allergic medications or taking shots for allergy desensitization are other alternatives.
What Is Good Asthma Care
Your doctor or nurse will tailor your asthma treatment to your symptoms. Sometimes you may need to be on higher levels of medication than at others.
You should be offered:
- care at your GP surgery provided by doctors and nurses trained in asthma management
- full information about your condition and how to control it
- involvement in making decisions about your treatment
- regular checks to ensure your asthma is under control and your treatment is right for you
- a written personal asthma action plan agreed with your doctor or nurse
It is also important that your GP or pharmacist teaches you how to properly use your inhaler, as this is an important part of good asthma care.
Recommended Reading: Can Acid Reflux Cause Asthma
Don’t Miss: Is Chocolate Good For Asthma
How Many People Can It Affect
Asthma is a prevalent condition worldwide.;According to the World Health Organization, it affects approximately 300 million people and kills 250,000 annually throughout the world; likewise, the United States affects nearly 7,5% of the population. It happens to be the most common chronic condition in childhood affecting 7 million US children.
In fact, due to the significant burden of this condition on the healthcare system, economy, and the overall society.;A global initiative for asthma is in charge of widespread education about it;for better management and diminishing its complications.
Dont Miss: Is Drinking Water Good For Asthma
Who Is More Likely To Develop This Condition
Many risk factors can make you more likely to develop it. The most important risk factors include:;
- Gender: In small children, boys are more likely to develop asthma than girls. Then, this proportion changes in the adult years, and women are more likely than men to develop asthma.;
- Family history of asthma: In this condition, the genetic factor has a lot of weight on your chances of getting it. A person who has a parent with asthma has three to six times more chance of having it. In fact, more than half of the patients with asthma have at least one parent who suffers from this disease.;
- History of allergic reactions: Or, as doctors call it, atopy is a major risk factor. If you suffer from other allergic conditions like rhinitis, conjunctivitis, or dermatitis , you are more likely to have this disease. This happens because of a higher sensibility to allergens, and it is known as allergic asthma.;
- Obesity: Many significant studies show that obese adults and children have a higher chance of suffering from this condition.;
- Environmental factors: People who are constantly exposed to air pollution, cigarette smoke, mold, or toxic fumes have a higher chance of asthma. The same happens to people who live in very cold or humid places. All these allergens can make you develop this disease in the long term.;
Don’t Miss: How To Help A Child Having An Asthma Attack
Bronchial Asthma: A Complex Disease
Bronchial asthma is a chronic disease characterized by airway hyperresponsiveness to a series of allergens or irritants. Coexistence of airway inflammation and remodelling has led to the hypothesis that the disease is inflammatory in nature, although the relationship between the inflammatory process and AHR has not been consistently shown. For example, studies examined by Brusasco etâal. revealed that markers of inflammation correlated with AHR in no more than 50% of the cases. In addition, pharmacological interventions have shown that inflammation can be modified independently of AHR and vice versa. It is significant that, despite a multitude of studies on cellular and molecular lung biology and immunology, the precise pathogenesis of asthma still remains unknown. In this review, we examine the disease from a different perspective. Specifically, we suggest that the pathogenesis of asthma can be better understood if we start from the principle that the lung is a complex organ and any chronic disease affecting it will also become complex.
How Do Your Airways Work When You Have Asthma
When you have asthma, your airways aren’t able to function as well as they should.
- Wheezing
- Chest tightness
Asthma causes inflammation, or swelling, in the lungs. It can also cause squeezing, called bronchoconstriction , and extra sensitive or twitchy airways.
When something bothers your airways, you have trouble breathing. This is;called an asthma attack or episode.;It gets harder to breathe because the tiny muscles around your airways squeeze tightly and they have swelling inside.
Your airways will make more mucus inside your airways, which makes it even harder to breathe. These changes in your airways can cause coughing and wheezing.
There is no cure for asthma. But you can take steps to manage it. If you have asthma, it’s important to see an asthma specialist, like an allergist or pulmonologist, to come up with the right asthma treatment plan. Medicines and avoiding asthma triggers can help reduce swelling and relax tight muscles in your airways.
ASTHMA Care for Adults
Don’t Miss: Can Asthma Make You Cough
What Happens During Asthma Attacks
Again, its an abnormal immune response. Your immune system is “abnormally” trained to recognize one or more asthma trigger. When you are not exposed to them you will probably experience no symptoms at all. So, between attacks, most asthmatics feel no symptoms; their breathing is normal . However, when exposed to asthma triggers, your immune system abnormally recognizes these triggers as harmful and initiates an abnormal immune response.
What Is An Overactive Immune Response
Asthma triggers, like dust mites, are harmless to most people. But, for those with asthma genes, they are treated as harmful pathogens. Airway cells respond to them the same way they respond to pathogens, by releasing chemicals. These chemicals cause airway inflammation. This is needed to trap and kill pathogens. But, in our case, it’s not needed. And, worse, this airway inflammation irritates cells in such a way as to causes asthma and asthma symptoms.
Also Check: Is Ice Cream Bad For Asthma
How Asthma Affects The Respiratory System
Most people with asthma are not always experiencing symptoms; they will go through times when it is worse, and other times where they feel perfectly well. Asthma can be classed as an inflammatory disease because the symptoms present when parts of the respiratory system become inflamed. When looking in more detail, it is actually the bronchi and the bronchioles which become inflamed. As well as this, there are special cells and glands which produce small amounts of mucous normally; and this is normal for every human being whether they suffer from asthma or not. However, in the context of people with asthma, the mucous glands can become swollen.
The combination of swollen glands and the inflamed bronchi and bronchioles results in a narrowed airway. This can sometimes create a wheeze or chesty cough, which is the bodys normal reaction to a narrowed airway. If you consider when you have a cold and there are extra amounts of fluid-like mucous and phlegm in your airway, your body coughs to try and remove it. However with asthma, it is actually the respiratory system inhibiting itself, so coughing does not normally actually help the problem.
For more details on Asthma visit our video online training course at www.proasthma.co.uk
Does That Mean Asthma Is An Autoimmune Disorder
No! An autoimmune disorder occurs when your immune system cannot tell the difference between pathogens and your own healthy tissue. When this happens, your immune system attacks healthy cells as though they were foreign invaders. This causes these cells to become inflamed and damaged. Examples include rheumatoid arthritis, psoriasis, lupus, type-1 diabetes, ulcerative colitis, and Addisons disease. However, there is one subgroup of asthma affected here, and its called Churg-Strauss Syndrome. But, overall, asthma is not an autoimmune disorder.
Don’t Miss: What Happens If The Military Finds Out You Have Asthma
Your Respiratory System And Asthma
An asthma patients guide to how the respiratory system works, with tips on keeping asthma under control.
Asthma is a common respiratory condition that affects over 26 million adults and children in the United States. Here’s a look at how the respiratory system works and how asthma impacts the respiratory system.
Upper respiratory tract The main parts of the upper respiratory system include the nose, mouth, throat and voice box. When you breathe in through your nose, the nasal cavity warms the air to keep it from irritating your sensitive airways. Cilia and mucus in the nasal passages trap germs and allergens. Once air is warmed and purified, it travels from your nose down to your throat and voice box and into the lower portion of your respiratory system.
Lower respiratory tract The lower respiratory tract is made up of the windpipe and lungs, including the bronchi, bronchioles and alveoli. The air moves down through your windpipe and into the bronchi. Airways that branch off into the lungs have cartilage embedded in their walls to keep the bronchi open. Inside the lungs, these airways then move into smaller passages called bronchioles. These are susceptible to swelling and constriction because there is no cartilage to hold them open.
Avoiding the impact of asthma These simple steps can help you keep your respiratory system healthy:
Medically reviewed in May 2018.
