How Is Copd Treated And Managed
If you smoke and have COPD, quitting is your best bet. Its virtually impossible to slow the progression of damage to the lungs if you dont. Of course, this process can feel daunting and be really challenging, but it can be done. If youre not sure where to start with quitting, the Centers for Disease Control and Prevention has a lot of resources to help, which includes support groups and a free quitline you can call .
Other COPD treatment options include:
Medications used to treat COPD symptoms include non-steroid medications that relax the small muscles around the airways and corticosteroids to reduce inflammation, both of which are usually breathed in using an inhaler. Oral steroids can be used during exacerbations to help calm your airways down, and a few other types of medications are available for severe COPD or when other medications dont work.
To avoid infectionssomething people with COPD are susceptible toyour doctor may prescribe an antibiotic during flare-ups.
People with moderate to severe COPD may require oxygen therapy, which is a lightweight portable unit that delivers supplemental oxygen to your lungs. It can help people with COPD feel more comfortable and allow them to carry on with daily activities.
Finally, surgery is an option for certain people with severe emphysema. That can include:
When To Get Medical Advice
See a GP if you have persistent symptoms of COPD, particularly if you’re over 35 and smoke or used to smoke.
Do not ignore the symptoms. If they’re caused by COPD, it’s best to start treatment as soon as possible, before your lungs become significantly damaged.
The GP will ask about your symptoms and whether you smoke or have smoked in the past. They can organise a breathing test to help diagnose COPD and rule out other lung conditions, such as asthma.
Find out more about how COPD is diagnosed.
Asthma And Copd: Whats The Difference And Is There A Link
Asthma and chronic obstructive pulmonary disease are lung diseases. Both cause swelling in your airways that makes it hard to breathe.
With asthma, the swelling is often triggered by something youâre allergic to, like pollen or mold, or by physical activity. COPD is the name given to a group of lung diseases that include emphysema and chronic bronchitis.
Emphysema happens when the tiny sacs in your lungs are damaged. Chronic bronchitis is when the tubes that carry air to your lungs get inflamed. Smoking is the most common cause of those conditions .
Asthma gets better. Symptoms can come and go, and you may be symptom-free for a long time. With COPD, symptoms are constant and get worse over time, even with treatment.
Recommended Reading: Are Chihuahuas Good For Asthma
What Is Niehs Doing
NIEHS conducts and supports asthma research from basic studies in laboratories to human clinical trials. This research focuses on complex relationships among the environment and peoples genetics and immune system. Projects include:
- Development of sensors that measure personal environmental triggers of asthma.
- Clinical trials that examine if reduced indoor air pollution can improve asthma symptoms.
- Data science methods that combine environmental data gathered across the United States.
Join an asthma study!
The goal of the Natural History of Asthma with Longitudinal Environmental Sampling study is to help scientists understand how bacteria and other factors in the environment affect people who have moderate to severe asthma.
Who can participate?
- Moderate to severe asthmatics.
- Males and females, aged 18-60.
- Females should not be pregnant or breastfeeding at the start of the study, but may still participate if they become pregnant during the study.
- Nonsmokers who are also not around significant amounts of secondhand smoke.
- No history of chronic obstructive pulmonary disease, emphysema, cystic fibrosis , pulmonary fibrosis, non-CF bronchiectasis, sarcoidosis, unstable angina, or pulmonary hypertension.
- Not allergic to methacholine.
- Able to provide your own transportation to clinic visits on the NIEHS campus in North Carolina. For more information about this study:
- NHALES: Asthma Study
Inflammatory Cells In Asthmatic Airways
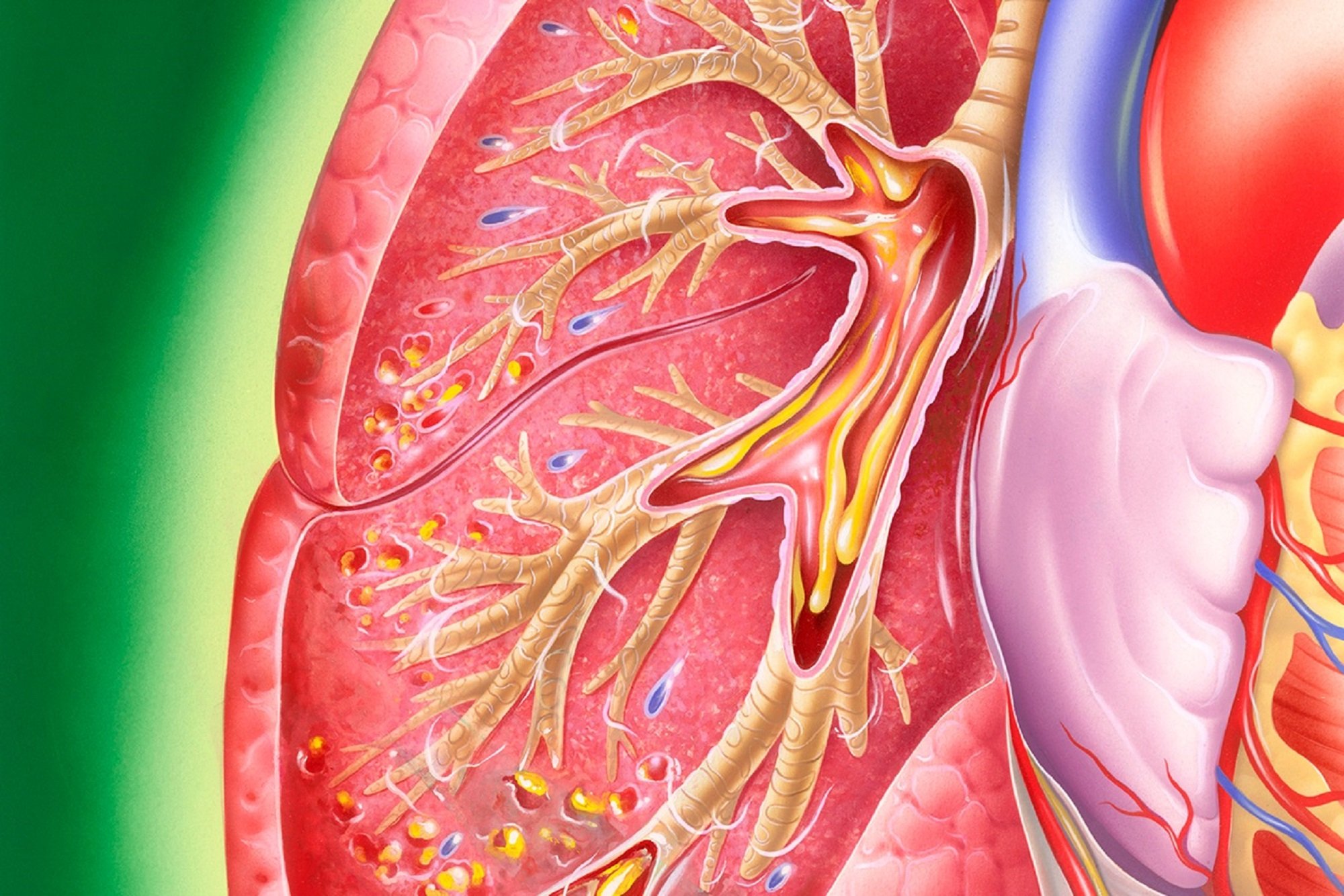
Mast cells -activated mucosal mast cells release bronchoconstrictor mediatorshistamine, cysteinyl leukotriens, prostaglandin D2. They are activated by allergens through IgE receptors or by osmotic stimuli . Eosinophils are in increased number in airways, release basic proteins that may damage epithelial cells, and have a role in releasing a growth factors and airway remodeling , T lymphocytes are in increased number and release specific cytokines, including IL-4, IL-5, IL-9, IL-13 that orchestrate eosinophilic inflammation and IgE production by B lymphocytes . There may also be an increase in inKT cells which release large amounts of T helper: Th1 and Th2 cytokines . Dendritic cells,Macrophages are in increased number, and release inflammatory mediators and cytokines that amplify the inflammatory response . Nutrophils are in increased number in airways and sputum of patients with severe asthma and in smoking asthmatics, but the role of these cells is uncertain and their increase may even be due to steroid therapy .
Recommended Reading: How Many People Have Asthma In The Usa
Asthma Symptoms In Kids
The most important asthma symptoms in children are:
- Cough: caused by the need to cough up extra mucus in the lungs or from the irritation of the airways
- Wheezing: the musical noise made by air coming out of narrow lung passages
- Shortness of breath
- Chest tightness or pain
Asthma attacks or flares come and go. When an attack begins, you will notice that your child’s symptoms become worse and may worsen rapidly. During an attack, you will likely notice that:
If the attacks become more severe, breathing can be very difficult, like trying to breathe through a straw. Your child may become less active and appear tired.
Knowing The Differences Between Copd And Asthma Is Vital To Good Practice
This content was published in 2011. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
The Outcomes strategy for people with chronic obstructive pulmonary disease and asthma was launched in July 2011 by the Department of Health, with the overall aim to drive improvements in outcomes for patients.1 Once implemented, it is expected to help people to avoid lung disease and lead longer and healthier lives. The strategy recognises the role of community pharmacy in supporting the management of people with respiratory disease through medicines use reviews and new pharmacy services.
In addition, the introduction of national target groups for MURs in England, under amendments to the NHS Community Pharmacy Contractual Framework, aims to ensure the service is provided to those who will benefit most. One of the target groups is patients with asthma or COPD.2 Both diseases have a major impact in the UK in terms of mortality and morbidity3 and the aim of MURs with these patients is to support them to take their medicines as intended, increase their engagement with their condition and medicines, and promote healthy lifestyles, in particular stopping smoking.
Read Also: What Do You Do When You Have An Asthma Attack
Diagnosing Asthma In Children Younger Than 6
It can be hard to tell whether a child under age 6 has asthma or another respiratory condition, because young children often cannot perform a pulmonary function test such as spirometry. After checking a childs history and symptoms, the doctor may try asthma medicines for a few months to see how well a child responds. About 40% of children who wheeze when they get colds or respiratory infections are eventually diagnosed with asthma.
Cdcs National Asthma Control Program
NACP was created in 1999 to help the millions of people with asthma in the United States gain control over their disease. The programs goals include reducing the number of deaths, hospitalizations, emergency department visits, school days or workdays missed, and limitations on activity due to asthma. The NACP collects data on state-specific levels to focus efforts and resources where they are needed.
The NACP leads national initiatives and provides state funding for a variety of activities focuses on surveillance, intervention, partnerships and evaluation. The NACP funds states, cities, school programs, and non-government organizations to help them improve surveillance of asthma, train health professionals, educate individuals with asthma and their families, and explain asthma to the public. The program has improved asthma treatment, management, and control in the U.S.
Don’t Miss: Does Weight Gain Make Asthma Worse
Inflammatory Cells In Copd
Neutrophils are present in sputum of smokers but increased in COPD and related to disease severity. They may be important in mucus hypersecretion and through release of proteases. Macrophages: big numbers are in airway lumen, lung parenchyma, and bronchoalveolar lavage fluid. They produce increased inflammatory mediators and proteases and may show defective phagocytosis. T lymphocytes: both CD4+ and CD8+ cells are increased in the airway wall and lung parenchyma, with big CD8+/CD4+ ratio. Increased is the number of CD8+ T cells and Th1 cells which secrete interferon- and express the chemokine receptor CXCR3. CD8+ cells may be cytotoxic to alveolar cells. B lymphocytes: are increased in peripheral airways and within lymphoid follicles, possibly as a response to colonization and infection. Eosinophils: increased eosinophil proteins in sputum and eosinophils in airway wall during exacerbations. Epithelial cells: May be activated by cigarette smoke to produce inflammatory mediators .
Are There Lifestyle Changes That Can Help
Weve said it already, but well say it again: It’s crucial to stop smoking whether you have either condition, as it can worsen the symptoms of both conditions, says Dr. Ogden.
Another step you can take is filtering out triggers that exacerbate asthma and COPD. Since fumes, allergens, irritants, and poor ventilation can worsen both COPD and asthma, Dr. Ogden suggests getting an air purifier with a HEPA filter, , and it can filter out up to 99.97% of dust, mold, pollen, bacteria, and other airborne particles of a certain size. Its sort of like a vacuum for the air you breathe.
She also suggests using the exhaust fan on your range hood when you cook, and using a vacuum with a HEPA filter.
Other small changes that can make a big difference: Avoid cleaning with products that could irritate your airways, and consider cleaning or doing activities such as gardening and yard work with a mask during peak season if youre allergic to outdoor allergens, Dr. Ogden adds.
Read Also: Can You Take Ibuprofen If You Have Asthma
Treatment Options For Obstructive Vs Restrictive Lung Disease
Treatment options will be somewhat different for these two types of respiratory illness.1 With obstructive lung disease, the goal is to reduce inflammation and relax the airways. So, treatments might include bronchodilators and/or inhaled steroids. Some medications are long-acting and some are shorter-acting.1
In addition, with COPD, supplemental oxygen therapy might be helpful. This is not generally prescribed in people who have asthma. Changes in lifestyle may also be helpful. For example, with asthma, learning to avoid your triggers can help keep your asthma under control.1
With restrictive lung disease, the treatment options are often more limited. They may also vary greatly, depending on the specific type of restrictive disease. Steroids and bronchodilators are sometimes used. Medications that suppress the immune system may also be helpful.1 Other options might include supportive oxygen therapy and even lung transplants.1
What Are The Symptoms Of Asthma
Asthma can range from very mild to more severe. Here are some of the common symptoms of asthma that are caused by airway inflammation and muscle spasm:
- Cough, with or without mucus/phlegm
- Shortness of breath
- Wheezing
- Activity limitation
Symptoms may be triggered or worsened by factors such as viral infections, common allergens, irritants , exercise and stress. In some cases, these respiratory symptoms can also be triggered by exercise or occur at night. Speak with your resource person to check what symptoms you may still feel when you are at your best.
Don’t Miss: What Happens If The Military Finds Out You Have Asthma
Strengths And Limitations Of The Systematic Review
One significant strength of this systematic review is being the first review to offer comprehensive information about the extent of availability and affordability of medicines and diagnostic tests of asthma and COPD in SSA. Despite this, some of the limitations are heterogeneity of the study findings and health facilities surveyed and the low methodological quality of the eligible original studies.
Therapeutic Responses In Asthma Copd And Overlap Syndrome
A comprehensive review of the available treatments for obstructive airway diseases is beyond the scope of this article however, it is important to appreciate that the nature of the underlying inflammation differs between asthma and COPD, as does the response to different classes of medications. Although specific interventions vary by disease, the treatment goals of asthma and COPD are similar and driven primarily by patient-centered outcomes such as controlling symptoms, optimizing health status and quality of life, and preventing exacerbations .
In general, therapies for COPD have a much more limited effect compared with those for asthma. While inhaled corticosteroids are the cornerstone of the pharmacologic management of patients with persistent asthma, inhaled bronchodilators are the therapeutic mainstay for patients with COPD. There are no disease-modifying medications currently available that can alter the progression of AO in either asthma or COPD. Smoking cessation, however, is an essential component of the successful management of any obstructive airway disease.
Recommended Reading: Can Allergies Cause Asthma Attacks
Recommended Reading: Beta Blockers In Asthmatics
Plasma And Sputum Biomarkers
The ongoing efforts in differential diagnosis of asthma-COPD overlap syndrome could not ignore plasma and sputum biomarkers. Iwamoto et al. investigated four potential biomarkers of COPD: surfactant protein a , soluble receptor for advanced glycation end-products , myeloperoxidase and neutrophil gelatinase-associated lipocalin . SP-A and sRAGE are pneumocyte-derived markers. MPO and NGAL are neutrophil-derived molecules, but NGAL can be also expressed by respiratory epithelial cells. There were five different subject groups: non-smokers, smokers, asthma patients, COPD patients, asthma-COPD overlap patients. In order to identify overlap syndrome, the researchers discovered that only sputum NGAL was significantly increased in overlap group, compared with COPD group and could differentiate patients with overlap from COPD patients. This means that elevated induced sputum levels of NGAL should point the overlap diagnosis, suggesting enhanced neutrophilic airway inflammation or airway epithelial injury in overlap, as Iwamoto and his colleagues have proven.
Are Asthma And Copd Disabilities
According to the Asthma and Allergy Foundation of America , the American Disabilities Act and Section 504 state that having a mental or physical impairment that severely limits one or more life activities, including breathing, can be considered a disability.
For people with asthma, this applies even if symptoms only show at certain times, and if the person uses medication, such as an inhaler, to control the problem.
To qualify for social security disability benefits with COPD, a person must have:
- A forced expiratory volume one that is the minimum for your height or less, from 1.05 to a person who is 5 feet tall to 1.65 to someone who is 6 feet tall.
- Chronic impairment of gas exchange resulting from a documented COPD.
Those who do not meet these requirements may be able to get other types of help, such as as medical-vocational allowance for people on a low income.
Also Check: What’s An Asthma Attack Feel Like
How To Know If My Asthma Is Well Controlled
Good asthma control means your symptoms are minimized. The following are indicators of asthma control:
- Daytime symptoms occur three times per week or less
- You don’t miss school, work or your activities because of asthma symptoms. Your asthma doesnt get in the way of exercise and physical activity
- Symptoms do not disturb your sleep
- You need your reliever less than four times per week
Defining Obstructive Vs Restrictive
Obstructive lung disease is a condition where the airflow into and out of the lungs is impeded.1 This occurs when inflammation causes the airways to swell, making them narrower. Because of that, breathing well becomes harder and air often gets trapped in the lungs. This results in something known as hyperinflation of the lungs. Exhaling becomes slower and shallower than in a person with a healthy respiratory system.1
Examples of obstructive lung disease include:1
Restrictive lung disease is a condition where the lungs don’t function effectively. People with this cannot take a full, deep breath and fill their lungs with air. This can be due to problems within the lungs themselves or due to some kind of damage from external forces .1
With intrinsic disorders, the lungs’ restriction is related to weak muscles, stiffness in the chest wall or damaged nerves.1 Examples of these diseases include:1
- Interstitial lung disease
- Sarcoidosis
- Pneumoconiosis
With extrinsic disorders, other non-respiratory diseases end up causing problems with the function of the airways and lungs. These can include:1
- Obesity
Also, both obstructive and restrictive disease will be diagnosed by using a careful medical history and a variety of pulmonary function tests. The results of those tests and your history will help a doctor determine which type of lung disease you might have.1
Don’t Miss: Side Effects Of Albuterol
What Are The Different Types Of Copd
The two most common conditions of COPD are chronic bronchitis and emphysema. Some physicians agree that asthma should be classified as a chronic obstructive pulmonary disease, while others do not. A brief description of asthma, is included below:
| 1
What is chronic bronchitis?Chronic bronchitis is a long-term inflammation of the bronchi , which results in increased production of mucus, as well as other changes. These changes may result in breathing problems, frequent infections, cough, and disability. |
1 |
Recommended Reading: Breathing Treatments Side Effects
