Tests That Diagnose Autoimmune Diseases
No single test can diagnose most autoimmune diseases. Your doctor will use a combination of tests and a review of your symptoms and physical examination to diagnose you.
The antinuclear antibody test is often one of the first tests that doctors use when symptoms suggest an autoimmune disease. A positive test means you may have one of these diseases, but it wont confirm exactly which one you have or if you have one for sure.
Other tests look for specific autoantibodies produced in certain autoimmune diseases. Your doctor might also do nonspecific tests to check for the inflammation these diseases produce in the body.
BOTTOM LINE: A positive ANA blood test may be indicative of an autoimmune disease. Your doctor can use your symptoms and other tests to confirm the diagnosis.
Treatments are also available to relieve symptoms like pain, swelling, fatigue, and skin rashes.
Eating a well-balanced diet and getting regular exercise may also help you feel better.
BOTTOM LINE: The main treatment for autoimmune diseases is with medications that bring down inflammation and calm the overactive immune response. Treatments can also help relieve symptoms.
More than 80 different autoimmune diseases exist. Often their symptoms overlap, making them hard to diagnose.
Autoimmune diseases are more common in women, and they often run in families.
When To See A Doctor
See a doctor if you have symptoms of an autoimmune disease. You might need to visit a specialist, depending on the type of disease you have.
- Rheumatologists treat joint diseases, like rheumatoid arthritis as well as other autoimmune diseases like Sjögrens syndrome and SLE.
- Gastroenterologists treat diseases of the GI tract, such as celiac and Crohns disease.
- Endocrinologists treat conditions of the glands, including Graves disease, Hashimotos thyroiditis, and Addisons disease.
- Dermatologists treat skin conditions, such as psoriasis.
The Healthline FindCare tool can provide options in your area if you need help finding a specialist.
Organ Index Of Thymus Spleen Adrenal Thyroid And Testicular Glands In Different Groups
illustrated that rats in the KYDS and ASS groups with induced thymus atrophy indicated immune suppression ; however, showed in the Figures and , rats with OVA exposure had induced thymus and spleen hyperplasia compared to those without OVA exposure which suggested immune activation due to allergy exposure . Figures and demonstrated that the KYDS and KYDSA groups manifested adrenal and thyroid atrophy , but testicular hyperplasia , and above three glands had hyperplasia in the ASS and ASSA groups in contrast to the NC group. Moreover, the adrenal gland from the AC group was atrophy compared to the NC group, but there was no significant difference in thyroid and testicular glands. As seen in , the ASS group was more obvious in thyroid and testicular gland hyperplasia than other groups .
In order to evaluate possible atrophic and/or hyperplasia effects on immune organs and HPTOA glands due to modeling, thymus, spleen, adrenal, thyroid and testicular gland were removed, carefully trimmed, and weighed after rats were sacrificed. Data are expressed as mean ± SD, n = 10 rats per group. and : **P< 0.01, *P< 0.05, versus the NC group. : **P< 0.01, versus the KYDS group or the ASS group. : **P< 0.01, *P< 0.05, versus the NC group; #P< 0.05, versus the KYDS group. : **P< 0.01, *P< 0.05, versus the AC group. : *P< 0.05, versus the KYDS group or the KYDSA group or the ASSA group.
Also Check: Smoking Weed Asthma
Asthma Is Not A Disease Of Inhaled Steriod Deficiency
- Richard L. Henry
Introduction The Australian Paediatric Respiratory Group has recommended a stepwise approach to the treatment of asthma.1 Children with infrequent episodic disease should usually take an inhaled bronchodilator such as salbutamol ‘as necessary’. Those with frequent episodic symptoms should receive preventive therapy with regular sodium cromoglycate or nedocromil sodium, together with a bronchodilator as needed for break-through symptoms. Those with persistent asthma, characterised by daily symptoms, should receive regular inhaled corticosteroids together with intermittent bronchodilators as needed.
Other clinicians recommend a different approach to the treatment of asthma, using inhaled corticosteroids as first-line therapy. This approach claims that inhaled corticosteroids should be started at the onset of asthma to prevent untreated airway inflammation leading to permanent lung damage.
Severity of asthma At one end of the spectrum of asthma are the children who have persistent disease. These children have persisting airways obstruction for weeks or months at a time, manifested by cough, wheeze and breathlessness. There is unanimous agreement that these children need regular preventive therapy and that inhaled corticosteroids will be the mainstay of drug management.
What Does Science Say About Vitamin D And Asthma
Research shows an important relationship between vitamin D deficiency and poor bone health. Scientists believe vitamin D may impact other areas of health, including asthma. According to research, vitamin D has antibacterial, antiviral and anti-inflammatory activity which might lower the risk of asthma attacks caused by respiratory infections.2
Here is a recent analysis of multiple studies that support the link between vitamin D and asthma:
Vitamin D for the Management of Asthma3
Researchers compared the results of nine studies. Seven included 435 children and two included 658 adults. They concluded that vitamin D is:
- Likely to reduce both the risk of asthma attack and health care use. But these findings were generally limited to only those with mild or moderate asthma. It also only looked at those with lower baseline vitamin D levels.
- Children and people with frequent severe asthma attacks were under-represented. More primary trials are needed to see if vitamin D can reduce the risk of severe asthma attacks in these groups.
Don’t Miss: What To Do When Having An Asthma Attack
Bronchoalveolar Lavage Fluid Preparation And Cytokines Analysis
Owning to the invasive pulmonary function test, the rats’ tracheas were cannulated, and their chests were opened. BALF was performed three times through the tracheal cannula . The recycling lavage aliquots about 1ml were pooled and centrifuged. The supernatant was stored at 20°C for cytokine detection. The levels of interleukin -2, IL-5, IL-6, IL-10, IL-13, granulocyte-macrophage colony-stimulating factor , and interferon- in BALF were detected using Bio-Plex Suspension Array System .
Vitamins That May Impact Your Asthma
Some scientists believe that asthma and vitamin deficiency are integrally linked. Researchers have looked into the role that certain vitaminslike vitamin D, vitamin C, and vitamin Eplay in the occurrence and severity of the disease. While it is clear that diet does influence the incidence and prevalence of asthma, what is less clear is whether vitamin supplementation can prevent asthma or improve its symptoms.
Don’t Miss: Are Allergies And Asthma Related
Objective Or Subjective: Is There A Link
Interestingly, while there are a plethora of results on Google on this subject, as well as people contemplating their personally correlated experiences, the writing seems to be based on the findings of just a handful of research articles . The most prominent include, “Is Iron Deficiency Anemia a Risk Factor in Asthmatic Children?” , “The impact of anemia and hemoglobin level as a risk factor for asthma and allergic diseases” , “Iron deficiency anemia as a risk factor in childhood asthma” , and “Iron Status is Associated with Asthma and Lung Function in US Women” .
The first three articles above focus on children and the last focuses on women. This is, presumably, due to the fact that men are less predisposed to iron deficiency anemia. This may be the reason they are excluded from the most easily accessed selection of the research.
The Connection Between Vitamin Deficiency And Asthma
While researching the possible causes of asthma, scientists have discovered that a lack of specific vitamins can be associated with the occurrence and severity of asthma. The following vitamins are found to be linked to asthma:
- A 2017 study published on Cureus revealed that lower than average vitamin D levels are linked to higher rates of asthma attacks.
- In another study, the deficiency of vitamin C was also identified as causing asthma. People who consume a typical western diet lacking in fresh food may suffer from vitamin C deficiency and respond poorly to inflammatory lung response in respiratory viral infections.
- A scientific review published in the American Journal of Respiratory and Critical Care Medicine found that consuming baby formula fortified with vitamin E may lower the risk of having childhood asthma in small children.
Itâs important to note that vitamin deficiency cannot be recognized as one of the primary causes of asthma. However, the lack of these vitamins reflects the general well-being of an individual. A person suffering from vitamin deficiency is more likely to have a weaker immune system and is more prone to suffer from infections, allergies, and conditions directly associated with asthma.
Read Also: Can You Take Aspirin If Allergic To Ibuprofen
About The Feno Project
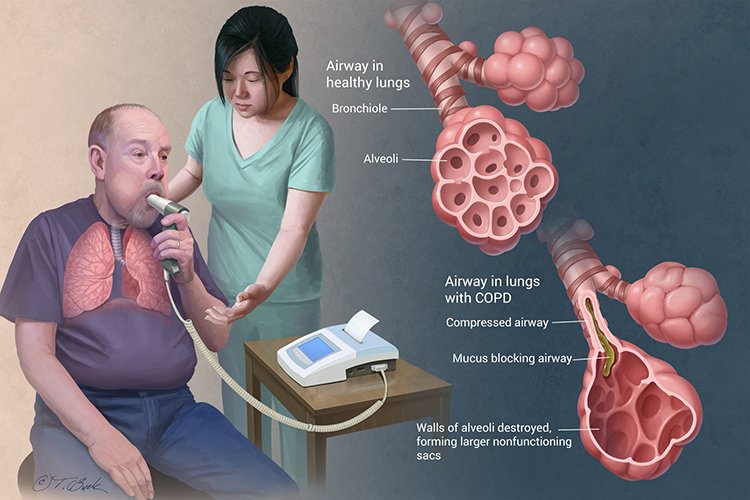
A Fractional Exhaled Nitric Oxide test is performed in order to test the levels of nitric oxide in the inflamed airways of asthma patients. While this test cannot diagnose asthma, it does measure one of asthmas primary symptoms. Earlier research found a positive correlation between residual volume and post-bronchodilator response . The purpose of the FeNO project is to investigate the connections between the measurements found in FeNO tests and asthma biomarkers like RV and BDR.
This project included measuring patients FeNO data and developing a retrospective chart review, which included patients pulmonary function tests and regression analysis. This project confirmed previous research and found a significant positive correlation between the FeNO data and RV and BDR. Researchers hope that this data will lead to the rise of FeNO testing at other airways clinics.
Analysis Of Hptoa And S/p Nerve System Function
To determine the function of HPOTA and S/P nerve system due to modeling, we analyzed plasma hormones and second messengers like c AMP and c GMP. showed the levels of CORT, T4, TSH, LH, and FSH that notably increased in plasma in the KYDS and KYDSA groups , but the level of ACTH significantly decreased compared to the NC group, which demonstrated that those groups had the dysfunction of HPTOA. Moreover, the ASS and ASSA groups activated the three HPTOA. Although the level of CORT went down and ACTH dropped up in the AC group, there was no significant difference with the NC group. illustrated that the ratio between c AMP and c GMP was remarkably reduced in the other five groups compared with the NC group , which indicated that those groups had a dysfunction of the S/P nerve system.
Function of HPTOA was evaluated by the analysis of plasma hormones. Data are expressed as mean ± SD, n = 10 rats per group. : **P< 0.01, *P< 0.05, versus the NC group. : **P< 0.01, *P< 0.05, versus the NC group or the AC group. : *P< 0.05, versus the KYDS group or the ASS group. : **P< 0.01, *P< 0.05, versus the NC group; #P< 0.05, versus the KYDS group. : **P< 0.01, *P< 0.05, versus the NC group. : *P< 0.05, versus the ASS group. : **P< 0.01, versus the NC group. : **P< 0.01, *P< 0.05, versus the NC group. : *P< 0.05, versus the ASS group.
Read Also: How To Help Asthma Without Inhaler
What Is Autoimmunity
Your immune systems job is to fight off foreign invaders in your body that cause disease and infection. Autoimmunity is a response that happens when your immune system antibodies malfunction and attack your healthy cells and tissues. These antibodies are called autoantibodies.2
Any disease that is caused by an autoimmunity response is called an autoimmune condition. Some examples are:2
- Rheumatoid arthritis
- Graves disease
How Is Pidd Treated
PIDD treatment will depend on which disease you have. Once diagnosed, you can manage the disease by working with your doctor to develop a treatment plan.
Treatment often starts with preventing and treating infections and boosting the immune system. Any infection should be treated promptly and aggressively. Patients may need mucus thinners, cough syrup or decongestants to relieve symptoms caused by infections. If the infection doesnt respond to oral antibiotics, then hospitalization and IV antibiotics may be necessary.
Some PIDD patients may be prescribed long-term antibiotics to prevent infections and avoid potential damage to the lungs or ears .
Another option for some is a stem cell transplant, which offers a permanent cure for several forms of PIDD. With this treatment, healthy stem cells are transferred to the person with immunodeficiency, offering anormally functioning immune system.
Gene therapy is an option for severe PIDD patients. Most PIDDs are caused by errors in specific genes, and with gene therapy its hoped that fixing these mutations can help to correct the PIDD.
Patients can boost their immune system with therapies designed to fight bacterial and viral infections by antibody replacement. The most common is IV or subcutaneous immunoglobulin infusions; these are mostlyprescribed for antibody deficiency.
Recommended Reading: How To Help Someone Having An Asthma Attack
How Is Asthma Connected To The Immune System
Scientists are still studying exactly how asthma is connected to the immune system. They think the immune system has a role in the asthma response and the development of asthma.1
Scientists do not know exactly why some people develop asthma. Some think asthma could be caused by an immune response to viruses. They believe standard viruses could cause the immune system to develop the behavior that leads to asthma in some people.5,6
The causes of intrinsic asthma are not well understood. This is because it can be triggered by so many things. But some scientists also think an autoimmune response may have a role in causing it. This potential link could help people with intrinsic asthma, who are sometimes more difficult to treat. It is possible that intrinsic asthma could respond to treatment with medicine used for autoimmune conditions.1
Characteristics Of The Nnips
The status of participants from the original NNIPS-1 subsample, aged 1423 yrs at follow-up, is summarised in . Out of 6,462 children who were alive at the end of the trial, 1,405 were no longer living in the study area and 303 had died. No information was available for 20 participants. 4,523 were eligible to participate and 3,879 responded to our respiratory survey. 3,345 attempted spirometry , and 3,075 performed spirometry according to standard criteria. We did not find differences between study groups in the proportion of participants who died , who moved out of the study area , who did not complete the respiratory survey or who refused to participate in the study . Participants who completed the respiratory survey were more likely to be of higher caste , to live in households that owned land , to own livestock and to have a father who was a farmer than the remaining 2,738 participants from the original substudy. We did not find important differences in demographic or socioeconomic status between study groups at follow-up .
Recommended Reading: Can You Join The Coast Guard With Asthma
Selective Polysaccharide Antibody Deficiencies
These individuals have normal quantitative immunoglobulin levels, however, they demonstrate a selective defect in their antibody response to polysaccharide vaccination . Functionally, SPAD patients have an increased incidence of infections . This disease can be demonstrated by a lack of response to unconjugated polysaccharide vaccine in patients with normal quantitative immunoglobulin levels. Patients with SPAD rarely require gamma globulin replacement.
Main Findings And Conclusions
Detection of PIDD as a potentially treatable underlying contributor to recurrent/acute exacerbations and morbidity of COPD, and provision of immunoglobulin G replacement therapy, when appropriate, may decrease the progression of COPD. Decreasing the severity and rate of exacerbations and admissions should improve the quality of life and longevity of an important subset of patients with COPD, while decreasing costs. Major steps toward achieving these goals include developing a high index of suspicion, more frequent use and appropriate interpretation of screening tests such as quantitative immunoglobulins and vaccine responses, and prompt institution of IgG replacement therapy when antibody deficiency has been diagnosed.
- Previous article in issue
You May Like: What Does Asthma Do To You
Does A Vitamin Deficiency Make Asthma Symptoms Worse
Asthma is the most common lung disease in the United States. In fact, the disease has affected around 8.3 percent of Americans. Though there are several causes of asthma, scientists have discovered a unique link between vitamin deficiency and asthma. Research has revealed that vitamin D, vitamin C, and vitamin E have some role in developing asthma and affecting its severity. This article reviews the possible impacts of vitamin deficiencies on asthma and whether vitamin supplementation has any role in preventing the disease or improving its symptoms.
Risks Of Pneumococcal Disease
Anyone can get pneumococcal disease but some people are at higher risk of infection or its complications. Every child under the age of 2 is at higher risk of IPD. Also, children with an immunocompromising condition or chronic illness such as: asthma, diabetes; HIV; chronic kidney, liver or heart disease; absent or poorly working spleen; nephrotic syndrome; chronic neurologic conditions causing difficulty with oral secretions; CSF leaks; transplants; immune deficiency ; sickle cell disease; and children with cochlear implants or on immunosuppressive therapy.
Adults with the following conditions are also at higher risk of IPD: asthma, HIV, diabetes, heart disease; and adults:
- who are smokers
- with alcoholism
- living in long-term care facilities
Invasive pneumococcal disease is most common in the very young and the elderly . You may also be at high risk for IPD if you:
- have certain chronic conditions
- have chronic organ disease
- have a non-functioning or missing spleen
- have a cochlear implant
- have a weakened immune system or are immune suppressed
Your risk for getting IPD can also be impacted by environmental or lifestyle factors.
You May Like: How Can Asthma Be Prevented
