How Is Asthma Classified
Asthma is classified into four categories based upon frequency of symptoms and objective measures, such as peak flow measurements and/or spirometry results. These categories are: mild intermittent mild persistent moderate persistent and severe persistent. Your physician will determine the severity and control of your asthma based on how frequently you have symptoms and on lung function tests. It is important to note that a person’s asthma symptoms can change from one category to another.
Mild Persistent Asthma: Step 2
People can treat mild asthma that persists over long periods with long-term control medications. These can reduce symptoms when used on a daily basis.
Doctors prefer to prescribe a low-dose ICS as a controller medication for mild persistent asthma.
In addition, a person can use a SABA inhaler when needed to relieve symptoms.
Asthma Severity Among Adults With Current Asthma
Asthma severity determines type and duration of treatment
Percentage with Persistent Severity
Asthma severity* is the inherent intensity of the disease process. Disease progression and symptoms vary among individuals and within an individuals experience over time. The population-based asthma severity prevalence estimate depends on whether the individual is treated or not and how well the individual responds to the treatment. Intermittent severity includes people who are well-controlled without long-term control medication. Persistent severity includes people who are on long-term control medications and people with uncontrolled asthma who are not on long-term control medication. Nearly 65% of adults with current asthma have persistent asthma 35% have intermittent asthma.
Intermittent and persistent asthma prevalence among adults varied by state during the years 2006-2010, but did not follow a specific geographic pattern. Intermittent asthma prevalence ranged from 23.6% in Alabama to 43.5% in Utah . Persistent asthma prevalence ranged from 56.5% in Utah to 76.4% in Alabama .
*National Asthma Education and Prevention Program Expert panel report 3: Guidelines for the Diagnosis and Management of Asthma, 2007. Available at: . Includes persons who answered yes to the questions: Have you ever been told by a doctor, nurse, or other health professional that you had asthma? and Do you still have asthma?
Read Also: Does Weight Gain Make Asthma Worse
This Article Has A Correction Please See:
Mild persistent asthmatic patients constitute a significant proportion of patients . These patients might be considered the silent majority of asthmatics. This is because they rarely visit their primary care physician with symptoms of asthma, and are even more rarely seen in a secondary or tertiary healthcare setting, where physicians with a focused interest in asthma management tend to work. It is partly for this reason that, until recently, very little attention has been paid to the morbidity associated with mild persistent asthma and very few studies have evaluated the responses of this patient population to treatment.
Asthma management guidelines typically describe mild persistent asthma as patients having: asthma symptoms more than weekly, but less than daily, and nocturnal symptoms less than weekly, with normal lung function or peak expiratory flow > 80%) between asthma episodes . However, most studies that claim to have studied patients with mild-to-moderate asthma have not included many patients with mild asthma, as reflected by the mean FEV1, which was usually in the range of 70% predicted normal and/or rescue 2-agonist use of 23puffs·day1. This makes these studies of little or no value in deciding on treatment strategies for patients with mild persistent asthma. However, there has been an increase in the number of studies focusing on the optimal management of mild persistent asthma, some of which have been published very recently.
Control As A Guide To Medication Adjustment

After targeted, step-based initiation of pharmacologic therapy, the classification of asthma control is used to adjust medication, stepping up or down depending on the level of control. Patients whose asthma can be classified as well controlled can be maintained on their current medications and, if stable for at least three months, a step down in therapy can be considered . Patients whose asthma is classified as not well controlled on their initial therapy are advised to step up one step and be reevaluated in two to six weeks for patients with very poorly controlled asthma, consider short-term oral systemic corticosteroid use and stepping up one or two steps, then reassessing in another two to four weeks.
ACQ = Asthma Control Questionnaire ACT = Asthma Control Test ATAQ = Asthma Therapy Assessment Questionnaire FEV1 = forced expiratory volume in one second.
note:The stepwise approach is meant to assist, not replace, the clinical decision making required to meet individual patient needs. Before step-up therapy: review adherence to medication, inhaler technique, environmental control, and comorbid conditions and, if an alternative treatment option was used in a step, discontinue and use the preferred treatment for that step.
ACQ values of 0.76 to 1.4 are indeterminate regarding well-controlled asthma.
Don’t Miss: Can Asthma Start Later In Life
Moderate Persistent Asthma: Step 3
Doctors also use long-term daily medication to treat moderate asthma that persists over long periods. These medications are often different from those that treat milder forms of asthma.
For moderate persistent asthma, doctors prefer to use either:
- a combination of a low-dose ICS and a long-acting beta agonist
- a medium-dose ICS
Alternative therapies include a low-dose ICS along with an LTRA or, less commonly, theophylline.
In addition, a person can use a SABA inhaler when needed to relieve symptoms.
What Are The Classification Guidelines Of Asthma
The 2007 NAEPP guidelines and the 2009 VA/DoD asthma management guidelines use the severity of asthma classification below, with features of asthma severity divided into three charts to reflect classification in different age groups . Classification includes intermittent asthma, mild persistent asthma, moderate persistent asthma, and severe persistent asthma.
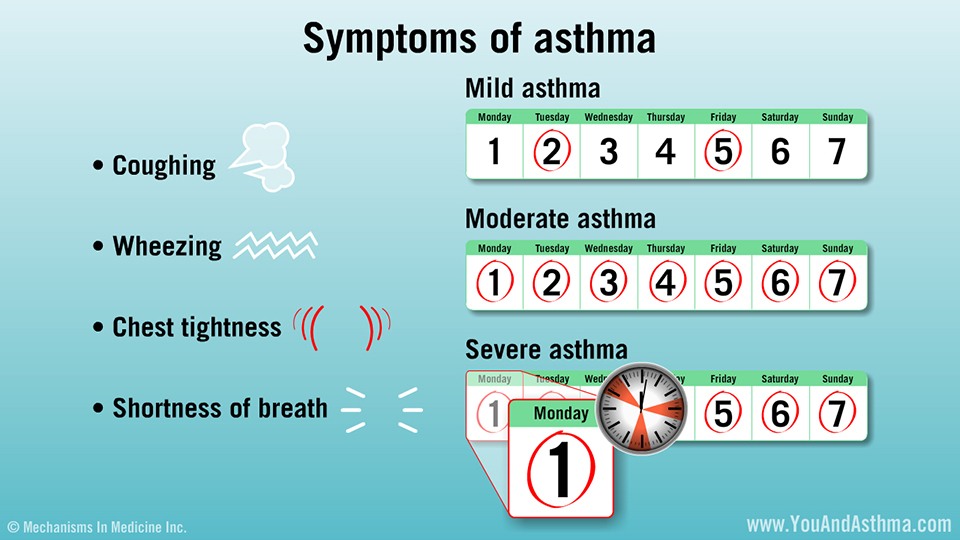
Intermittent asthma is characterized as follows:
- Symptoms of cough, wheezing, chest tightness, or difficulty breathing less than twice a week
- Flare-ups are brief, but intensity may vary
- Nighttime symptoms less than twice a month
- No symptoms between flare-ups
- Lung function test FEV1 is 80% or more above normal values
- Peak flow has less than 20% variability am-to-am or am-to-pm, day-to-day
Mild persistent asthma is characterized as follows:
- Symptoms of cough, wheezing, chest tightness, or difficulty breathing 3-6 times a week
- Flare-ups may affect activity level
- Nighttime symptoms 3-4 times a month
- Lung function test FEV1 is 80% or more above normal values
- Peak flow has less than 20-30% variability
Moderate persistent asthma is characterized as follows:
- Symptoms of cough, wheezing, chest tightness, or difficulty breathing daily
- Flare-ups may affect activity level
- Nighttime symptoms 5 or more times a month
- Lung function test FEV1 is above 60% but below 80% of normal values
- Peak flow has more than 30% variability
Severe persistent asthma is characterized as follows:
Read Also: Joining Army With Asthma
Classification Of Asthma Severity
Ideally, asthma severity is determined before initiating therapy. The EPR-3 guideline classification divides asthma severity into four groups: intermittent, persistent-mild, persistent-moderate, and persistent-severe. Mild-intermittent, a classification in previous reports, has been eliminated. This term really only applies to mild disease, and not to patients with periods of moderate or severe exacerbation.
Classification of a patient’s disease also depends on current impairment and future risk. Impairment is determined by patient symptoms and objective measurement of lung function. The guideline recommends that, at a minimum, assessments of the patient’s symptoms include daytime symptoms, nighttime awakenings, frequency of short-acting beta agonist use for symptom relief, and inability to do normal activities because of symptoms . Spirometry is recommended as a component of the determination of current impairment. As mentioned previously, future risk is categorized by the frequency of oral systemic corticosteroid use.
|
2 per year |
2 per year |
|
Consider severity and interval since last exacerbation frequency and severity may fluctuate over time for patients in any severity category relative annual risk of exacerbations may be related to FEV1 |
FEV1 = forced expiratory volume in one second FVC = forced vital capacity.
Personal Asthma Action Plan
As part of your initial assessment, you should be encouraged to draw up a personal asthma action plan with your GP or asthma nurse.
If youve been admitted to hospital because of an asthma attack, you should be offered an action plan before you go home.
The action plan should include information about your asthma medicines, and will help you recognise when your symptoms are getting worse and what steps to take. You should also be given information about what to do if you have an asthma attack.
Your personal asthma action plan should be reviewed with your GP or asthma nurse at least once a year, or more frequently if your symptoms are severe.
As part of your asthma plan, you may be given a peak flow meter. This will give you another way of monitoring your asthma, rather than relying only on symptoms, so you can recognise deterioration earlier and take appropriate steps.
Want to know more?
Don’t Miss: What Does A Nebulizer Do For Asthma
What Is Considered Moderate Asthma
ModerateAsthmaAsthmamoderatemoderateasthma
Also question is, what are the 4 categories of asthma?
The EPR-3 guideline classification divides asthma severity into four groups: intermittent, persistent-mild, persistent-moderate, and persistent-severe.
Likewise, what are the 3 types of asthma? There are many different types of asthma, brought on by many different triggers.
- Adult-Onset Asthma. Can you get asthma as an adult?
- Allergic Asthma.
- Occupational Asthma.
Keeping this in consideration, what is considered mild asthma?
Asthma is considered mild persistent if without treatment any of the following are true: Symptoms occur on more than 2 days a week but do not occur every day. Attacks interfere with daily activities. Nighttime symptoms occur 3 to 4 times a month.
What is considered asthma?
Asthma is a chronic, or long-term, condition that intermittently inflames and narrows the airways in the lungs. The inflammation makes the airways swell. Asthma causes periods of wheezing, chest tightness, shortness of breath, and coughing. Asthma affects people of all ages and often starts during childhood.
Side Effects Of Relievers And Preventers
Relievers are a safe and effective medicine, and have few side effects as long as they are not used too much. The main side effects include a mild shaking of the hands , headaches and muscle cramps. These usually only happen with high doses of reliever inhaler and usually only last for a few minutes.
Preventers are very safe at usual doses, although they can cause a range of side effects at high doses, especially with long-term use.
The main side effect of preventer inhalers is a fungal infection of the mouth or throat . You may also develop a hoarse voice and sore throat.
Using a spacer can help prevent these side effects, as can rinsing your mouth or cleaning your teeth after using your preventer inhaler.
Your doctor or nurse will discuss with you the need to balance control of your asthma with the risk of side effects, and how to keep side effects to a minimum.
Read Also: Can Allergies Cause Asthma Attacks
Follow The Recommendations Below To Reduce Your Chance Of An Asthma Attack While Cleaning Follow Recommendations For Cleaning Your Home And In Your Facility
- If you have asthma:
- Ask an adult without asthma to clean and disinfect surfaces and objects for you.
- Stay in another room when cleaners or disinfectants are being used and right after their use.
- Use cleaning agents and disinfectant only when necessary. In routine situations, high-touch surfaces and objects might be cleaned effectively with soap and water.
- Make a list of the urgent care or health facilities near you that provides nebulizer/asthma treatments and keep it close to your phone.
- If you have an asthma attack, move away from the trigger, such as the cleaning agent or disinfectant or the area that was disinfected. Follow your Asthma Action Plan. Call 911 for medical emergencies.
Current Treatment Recommendations For Mild Persistent Asthma
Asthma treatment guidelines have been consistent in describing the goals and objectives of asthma treatment. These are to: 1) minimise or eliminate asthma symptoms 2) achieve the best possible lung function 3) prevent asthma exacerbations 4) do the above with the least possible medications 5) minimise short- and long-term adverse effects and 6) educate the patient about the disease and the goals of management . In addition to these goals and objectives, each of these documents has described what is meant by the term asthma control. This includes the objectives above but also includes minimising the need for rescue medications, such as inhaled 2-agonists to less than daily use, minimising the variability of flow rates that is characteristic of asthma, as well as having normal activities of daily living. Some of these outcomes can be regarded as patient centred, which are outcomes that the patient would regard as obvious benefits of treatment, such as eliminating asthma symptoms, preventing severe exacerbations, normal activities of daily living and minimising medication adverse effects. Other outcomes can be considered as physician centred, particularly measurements of lung function, which are very important in establishing asthma control but changes in which are often not recognised by the patient. This distinction is particularly important in studies of mild asthma, where lung function is already normal.
Don’t Miss: Smoking Weed And Asthma
What Is Classed As Severe Asthma
4.9/5Severe asthmaasthmaasthmaasthmaSevere asthmaasthma
A severe asthma attack can cause symptoms such as:
Subsequently, question is, what is considered uncontrolled asthma? If your peak flow measurements are more than 15% below their normal levels, it may be a sign of nighttime asthma. Having nighttime asthma symptoms is a sign of uncontrolled asthma.
Similarly, what are the 3 types of asthma?
There are many different types of asthma, brought on by many different triggers.
- Adult-Onset Asthma. Can you get asthma as an adult?
- Allergic Asthma.
What asthmatics should not eat?
Foods To Avoid With Asthma
- Eggs.
The Reason Why It Is Difficult To Differentiate Asthma From Copd
In 1995, the American Thoracic Society stated:
it may be impossible to differentiate patients with asthma whose airflow obstruction does not remit completely from persons with chronic bronchitis and emphysema with partially reversible airflow obstruction and bronchial hyperresponsiveness.
The real issue is that both asthma and COPD are not single diseases, but rather syndromes consisting of several endotypes and phenotypes, which implies the possibility of a spectrum of different specific conditions that might also be relatively rare., Accordingly, the current definitions of asthma and COPD do not reflect the heterogeneity of disorders characterized by airway obstruction in the community, which may have differing pathophysiological processes, clinical features, or response to medical treatment. It is becoming increasingly obvious that these different endotypes and phenotypes must be recognized, in order to be properly treated with targeted therapy.
As elegantly pointed out by Reddel, even ACOS cannot be understood as a single disease or a single phenotype. In fact, it includes different phenotypes, such as patients with COPD and eosinophilic inflammation, patients with asthma and severe disease or who smoke in whom there is predominantly neutrophilic inflammation, and patients with asthma who have largely irreversible airway obstruction due to structural changes.
Don’t Miss: What Is The Blood Test For Eosinophilic Asthma
Ongoing Management Of Asthma
Ongoing management centers on controller medications. These include inhaled corticosteroids and leukotriene receptor antagonists. Theophylline and cromolyn are still listed, but these are not preferred agents, and they do not work as well as inhaled corticosteroids or leukotriene receptor antagonists. Inhaled corticosteroids are the fundamental and first-line therapy in ongoing management because of their proven effectiveness and, in recommended doses, few systemic adverse effects. Well-designed studies demonstrate that inhaled corticosteroids improve asthma control more effectively in children and adults than any other single long-term controller medication.15,16
Written action plans detailing medications and environmental control strategies tailored for each patient are recommended for all patients with asthma, and especially for patients with persistent asthma.1723 Examples of action plans are available at the National Heart, Lung, and Blood Institute Web site .24
Planned asthma-care visits are one of the key recommendations of the new guidelines. These visits are essential for adequate teaching and asthma control. Strategies for planned visits have been published.25 Patients with intermittent asthma may need to be evaluated only once yearly. Those on controller agents should be seen at least twice yearly, and as often as every four months.
Who Gets Severe Asthma
Severe asthma affects both adults and children. It can develop at any age. Most people who are diagnosed with severe asthma already have an asthma diagnosis: perhaps their asthma changed over time, or developed into severe asthma because of hormonal changes, or pneumonia for example.
Some people are diagnosed right away with severe asthma, but its likely that they had asthma for some time before without it being diagnosed as severe. And it can take time to get a diagnosis of severe asthma.
I was diagnosed with asthma at 35, but my GP said Ive probably always had it. I spent a lot of time in hospital with chest infections and croup as a child. In the lead-up to my severe asthma diagnosis, aged 40, I had pneumonia and started getting a lot of infections. My asthma changed and I could barely walk or move.
You May Like: Can You Join The Air Force With Asthma
