Management Of Patients Admitted To The Hospital: Wards And Icu Care
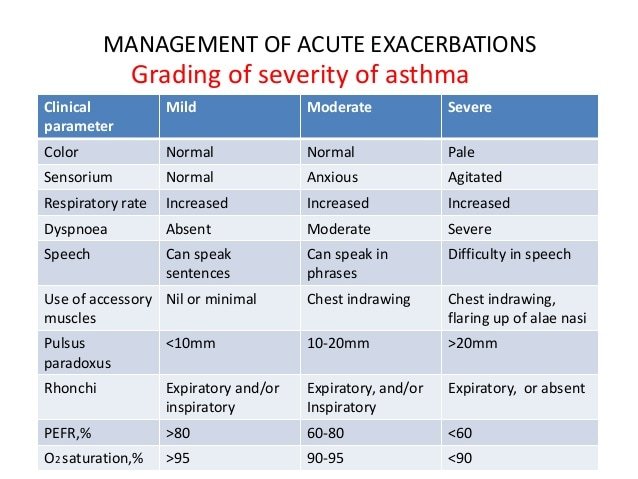
Careful consideration must be given to the level of care required when a patient with an exacerbation of asthma is admitted to the hospital. In general, guidelines suggest that patients should be admitted for observation and further treatment if the pretreatment FEV1 or PEF is < 25% of predicted or of personal best or if the post-treatment values are < 40% after emergency department treatment. Typically, patients who demonstrate a poor response to therapy , persistent or unresponsive hypercapnia, altered mental status, hypotension, or have significant comorbid conditions should be admitted to the ICU.
Although many patients maintain good oxygen saturations despite severe airway obstruction, some patients develop small airway mucus plugging even after the PEF/FEV1 normalize. Guidelines suggest that oxygen should be administered via nasal cannula or oronasal mask to maintain an arterial oxygen saturation of 9395% in adults and 9498% in children. In severe exacerbations, low-flow oxygen therapy by titrating the saturation to 9395% was associated with better physiological outcomes than with high-flow 100% oxygen therapy.
Management Of Acute Asthma Exacerbations
SUSAN M. POLLART, MD, MS; REBEKAH M. COMPTON, MSN, FNP-C; and KURTIS S. ELWARD, MD, MPH, University of Virginia Health System, Charlottesville, Virginia
Am Fam Physician.;2011;Jul;1;84:40-47.
;Patient information: See related handout on how to treat an asthma attack, written by the authors of this article.
In 2005, the prevalence of asthma in the United States was nearly 8 percent , and approximately 4 percent of Americans experienced an asthma attack.1,2 There have been many advances in medical therapy to prevent the worsening of asthma symptoms, including an improved understanding of asthma etiology, identification of risk factors for asthma exacerbations, and evidence supporting the benefits of written asthma action plans.
In persons older than two years with asthma, neither the injectable nor the intranasal influenza vaccine increases the likelihood of an asthma exacerbation in the period immediately following vaccination. However, one study of infants found an increase in wheezing and hospital admissions after intranasal influenza vaccination.7 Seasonal influenza vaccine does not reduce the risk of developing an asthma exacerbation. Influenza vaccination appears to improve asthma-related quality-of-life in children during influenza season.7
Testing For Severe Asthma
Before you can be tested for severe asthma, you will need a referral from your primary healthcare asthma provider to either an asthma specialist or allergy specialist . The specialist will review your medical history, your current asthma treatment plan and do a physical exam to assess your symptoms. If the specialist thinks you may have severe asthma, they will discuss additional testing with you to determine your specific type. This often starts with testing to identify a biomarker.
Biomarkers help determine what is causing the inflammation in your airways. Taking a blood sample, analyzing a mucus sample or taking a breathing test that measure substances in your breath droplets are all common tests doctors use. These tests are performed in a doctors office or an outpatient clinic setting. Your specialist will recommend one or more of these tests based on your medical history and current symptoms. Once the biomarkers are identified, your doctor can determine the type of severe asthma and the different treatment options that are available to treat that specific type.
Recommended Reading: Diy Nasal Inhaler
Whats The Outlook For People With Asthma
Most people with asthma are able to manage symptoms and maintain a good quality of life.
An acute exacerbation of asthma can be a life-threatening event. However, you should be able to resume your normal activities once its under control. Of course, youll want to avoid known triggers and follow your doctors advice for management of your asthma.
If you have asthma, you should have an action plan in place. Work with your doctor to come up with a plan so youll know what to do when symptoms flare up.
Exacerbations And Accelerated Loss Of Lung Function
A cycle of exacerbations and accelerated loss of lung function in asthma: Acute severe exacerbations in susceptible asthmatics activate pathways of inflammation and remodelling resulting in deterioration of lung function. Accelerated loss of lung function in turn puts these patients at increased risk of recurrent exacerbation resulting in a vicious cycle that may promote the exacerbationprone phenotype.
Read Also: Marines Asthma
What Types Of Asthma Are There
Healthcare providers identify asthma as intermittent or persistent . Persistent asthma can be mild, moderate or severe. Healthcare providers base asthma severity on how often you have attacks. They also consider how well you can do things during an attack.
Asthma can be:
- Allergic: Some peoples allergies can cause an asthma attack. Molds, pollens and other allergens can cause an attack.
- Non-allergic: Outside factors can cause asthma to flare up. Exercise, stress, illness and weather may cause a flare.
Read Also: Pediatric Spirometry Normal Values
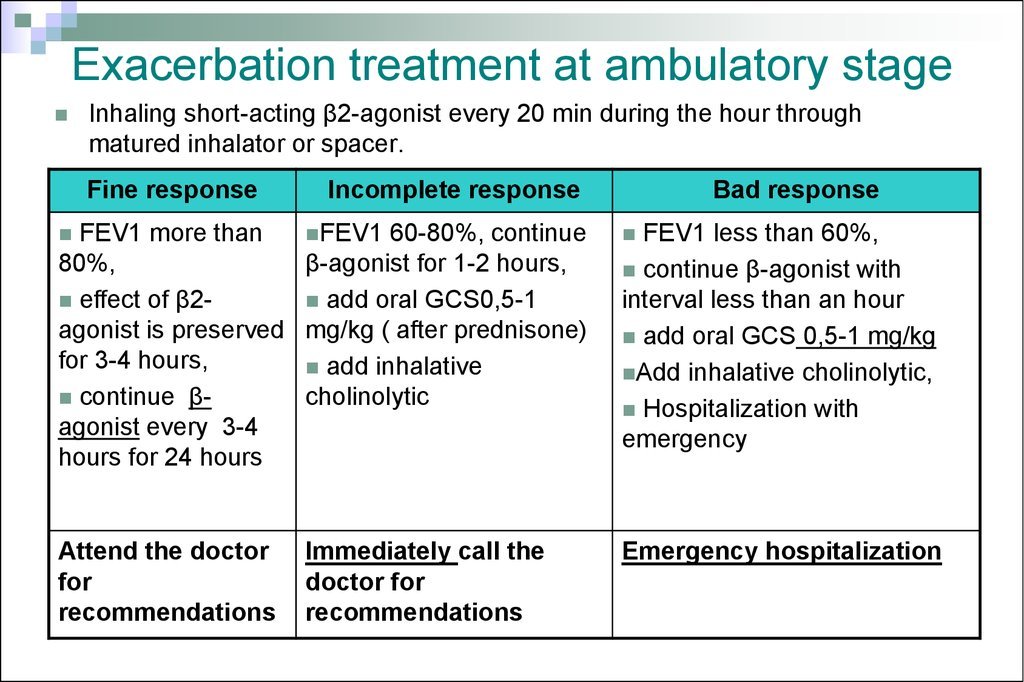
Initial Therapy Of Asthma Exacerbation In Children Older Than 2 Years
- The first-line therapy: age-related doses of salbutamol through the aerosol metered dose inhaler with a spacer or nebulizer. The inhalation therapy is immediately started with 2-4 doses of the short-acting 2-agonist with aerosol metered dose inhaler with a spacer or nebulizer ;
- In mild and moderate aggravation, the effectiveness of short-acting beta2-agonists therapy in the form of aerosol metered dose inhaler with a spacer is similar to that of a nebulizer ;
- If the symptoms are not amenable to treatment with salbutamol, then use Berodual;
- Double the dose of basic therapy for 5-7-10-14 days . If exacerbation is severe, you can go a step higher in the treatment for at least 3 months;
- If bronchodilators are inefficient , at the time of exacerbation you can add budesonide suspension through the nebulizer;
- In children with exacerbation of asthma which is not controlled by inhalation of Berodual through aerosol metered dose inhaler with a spacer to 6-8 doses/day, it is necessary to call an ambulance. Additional doses of bronchodilators are given as needed while waiting for the doctor;
- At the time of delivery of a child with a severe asthma attack in the emergency department, a bronchodilator + suspension of budesonide through a nebulizer, inhalation with oxygen are prescribed;
- Berodual is canceled if inhalation of short-acting 2-agonists is required more than 4 hours later. In this case, youd better use salbutamol.
Also Check: Do Chihuahuas Help With Allergies
Inhaled Corticosteroids And Long
In patients with poorly controlled asthma and a history of prior asthma exacerbations, the combination of budesonide and formoterol significantly reduces asthma exacerbations compared with ICS alone. ICS/LABA have consistently been shown to prevent exacerbations., , The benefit of ICS/LABA to prevent exacerbations versus ICS alone is primarily seen in patients requiring higher doses of ICS, thus suggesting that combination therapy to prevent exacerbations should be reserved for patients with more severe disease.
Asthma control can vary even in the face of ongoing ICS/LABA treatment. Consequently, the use of ICS/LABA combinations both for maintenance and symptom relief has been investigated and shown to reduce exacerbations., , These benefits are also seen in children with a prior history of severe asthma exacerbations and poorly controlled moderate-to-severe persistent asthma despite the use of moderate doses of ICS. The use of ICS/LABA as maintenance and reliever treatment should be restricted to formoterol because of its quick onset of action, safety profile, and dose-response effect.
What You Need To Know About Your Childs Asthma
There are many things to think about and plan for when your child has asthma. It is important to learn as much as you can about the condition. Your doctor and pharmacist are there to help you. Talk to them about any concerns you may have about your childs asthma.;To manage your childs asthma effectively, it is important to know:;
- the pattern of their asthma;
- their;asthma medications what they do and how to help your child take them properly;
- what to do if they have an asthma attack know and follow;asthma first aid.;
Make sure you have an updated written;asthma;action;plan and understand how to use it.;
Don’t Miss: What To Do When Someone Has An Asthma Attack
Asthma Peak Week: How To Exercise Safely With Asthma
The third week of September is known as Asthma Peak Week, the week with the highest numbers of asthma attacks and hospitalizations every year. Allergen levels are at their highest this week, particularly common allergens like ragweed pollen, dust, and mold, and this can make any activity difficult. You might be reluctant to work out, but regular exercise can improve asthma symptoms by increasing lung capacity and reducing inflammation. A well-considered exercise plan guided by a medical professional is vital to ensuring you can exercise safely with asthma, so read on to learn what to discuss with your doctor about creating an exercise plan for you!
You May Like: Asthma Weight Gain
Can I Get A Blue Badge If I Have Asthma
If youve previously been refused a blue badge you can appeal or re-apply using the same procedure, however, blue badges are issued based on symptoms of mobility rather than on diagnosis of a specific condition. For example, a diagnosis of asthma, multiple sclerosis or incontinence may not automatically qualify you.
Read Also: What To Do If You Have Asthma And No Inhaler
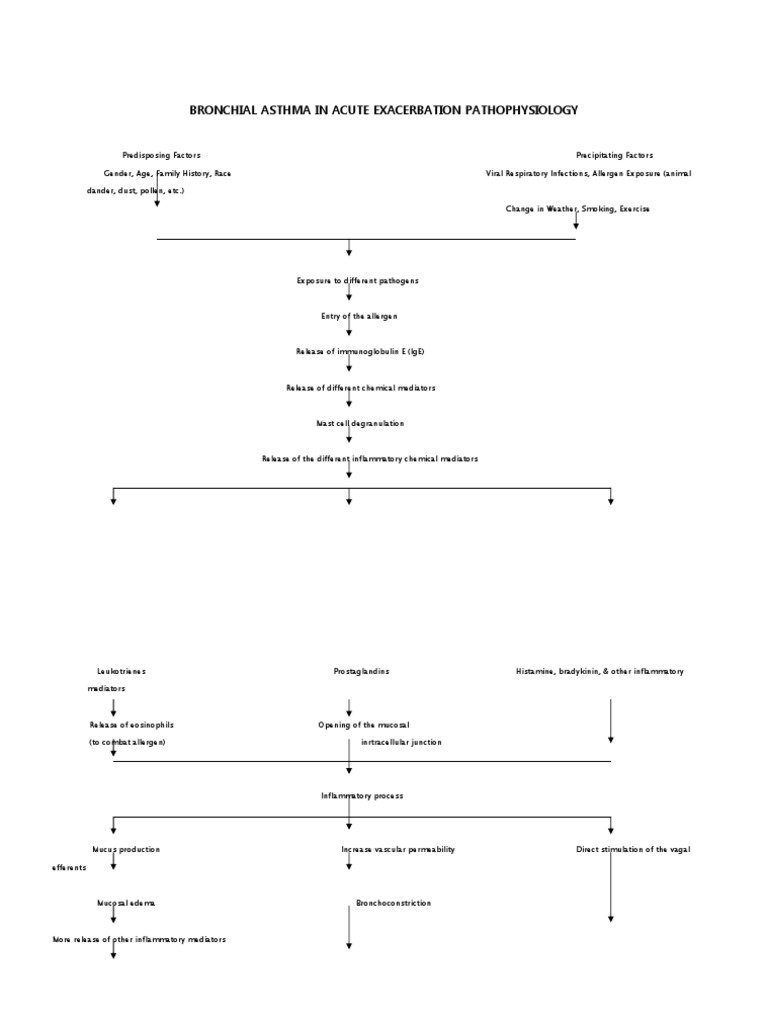
Fungal Infections And Acute Exacerbations Of Bronchial Asthma
The role of fungi and mold in AEBA is much less clear than viral and bacterial infections. It has been shown that fungal sensitization increases the risk of having more severe asthma and the risk of dying in asthma patients increases with increased spore exposure . Additionally, fungal sensitivity to Aspergillus and Clasdosporium species increases the risk of adult-onset asthma . The term severe asthma associated with fungal sensitization has been previously coined to describe patients with fungal sensitivity and persistent severe asthma who have some improvement with antifungal therapy . Denning et al. demonstrated a significant improvement in quality of life in patients with SAFS who were treated with oral itraconazole for 8;months . More specifically, sensitivity to Aspergillus fumigatus has been directly linked to severe persistent asthma in adults and is the cause of allergic bronchopulmonary aspergillosis . Both oral corticosteroids and antifungal therapies have been shown to be partially successful in controlling symptoms of ABPA including improving asthma related symptoms.
What Is Asthma Attack
Asthma can flare-ups are when asthma symptoms get worse. They happen when airways get more irritated and inflamed than usual.
During an asthma attack , you might have:
- trouble breathing
- a whistling sound while breathing
- a cough
- a fast heartbeat
Some flare-ups are serious, but others are mild. Flare-ups can happen suddenly or build up over time, especially if people dont take their asthma medicines as directed.
Things that bring on a flare-up are called triggers. Triggers vary from person to person, but common ones include:
- allergies to things like pollen, mold, and pet dander
- irritants and pollutants in the air
- respiratory infections, like colds or flu
- weather conditions
- exercise
- gastroesophageal reflux
An important part of managing asthma is avoiding triggers. Your childs doctor will work with you to create a care plan that helps prevent flare-ups as much as possible.
You May Like: Asthma Relief Without Inhaler
Also Check: How To Treat Asthma Attack
How Do You Stop An Asthma Attack Without An Inhaler
If you are diagnosed with asthma, you should make sure you have an inhaler with you at all times. However, if a worst case scenario occurs and you experience when you dont have a reliever inhaler with you, there are practical steps you can take to ease your symptoms.
- Stay as calm as you can find a way to reduce any anxiety, such as holding someones hand or playing music
- Sit upright this will help keep your airways open
- Breathe slowly and deeply slowing down your breathing can reduce the risk of hyperventilating
- If something appears to have triggered your asthma, such as breathing in cold air or being exposed to smoke, move away from the trigger
- Try breathing exercises the pursed lip breathing technique can help you deal with shortness of breath
- Have a drink containing caffeine there is some evidence to suggest that caffeine can help improve airway function for up to four hours.
Asthma can be a life-threatening condition, so at the very least, aim to keep a spare reliever inhaler in your handbag, locker at work or coat pocket.
Strictly Follow Your Medication As Prescribed By Doctor
Either you feel your asthma symptoms or not, you have to strictly follow your asthma medication as prescribed by your healthcare provider. Many of us make this mistake by stopping the medications when we dont feel any symptoms.
Its a very bad practice that will worsen your asthma symptoms anytime when they get a trigger and youll have a sudden asthma attack. You should always remember that asthma is a chronic disease. Once you have asthma means youll have it all the time.
Also Check: Medical Marijuana And Asthma
Management Of Status Asthmaticus In The Icu
Patients admitted to the ICU include individuals who require ventilator support or those with severe asthma for whom therapy failed. Most often they have refractory hypercapnia, persisting or worsening hypoxemia, deteriorating PEF/FEV1, drowsiness, confusion, or impending signs of respiratory arrest. Elective intubation by an experienced clinician is always recommended as soon as signs of deterioration are present. Intubation and mechanical ventilation may lead to hypotension and barotrauma secondary to high positive intrathoracic pressures. Care must be taken to assure that intravascular volume is adequate before intubation, and a bolus of intravenous normal saline solution is often recommended before initiation of mechanical ventilation.
Although there are no studies that determined the optimal mode of mechanical ventilation, it seems prudent to use the mode with which one is most familiar. Most researchers have recommended an initial minute ventilation of 90130 mL/kg ideal body weight , with further adjustments based on pH and the plateau airway pressure. Based on studies by Tuxen and Lane and Peters et al, we usually use a tidal volume of 89 mL/kg with a breathing frequency of 1014 breaths/min, a flow of 100 L/s, and 0 PEEP. However, many institutions prefer to use tidal volumes of 68 mL/kg ideal body weight., We adjust the setting to maintain a plateau pressure of 30 cm H2O and judiciously adjust ventilator-applied PEEP based on its ability to lower intrinsic PEEP.
Asthma Symptoms In A Severe Allergic Reaction
People having a severe allergic reaction can also have asthma-like symptoms. If the person has an anaphylaxis action plan, follow the instructions. If they have known severe allergies and carry an adrenaline autoinjector , use that before using asthma reliever medication.In case of an emergency, call triple zero and ask for an ambulance.
Also Check: Does Ibuprofen Make Allergies Worse
Antibacterial And Antiviral Approach To A Patient With Severe Aeba Or Critical Asthma Syndrome
Early empiric therapy in both bacterial and viral pneumonia has been shown to reduce morality, especially when initiated within 12;h . Additionally, acute exacerbations of asthma predominately have an infectious trigger, most particularly viral, but their early treatment in AEBA does not correlate with the similar outcomes of community acquired pneumonia . However, given the immediate need for care, we recommend an approach of early empiric therapy with aggressive de-escalation.
All patients presenting with severe acute asthma exacerbation and at risk for critical asthma syndrome should have a microbiologic work up that consists of standard sputum culture and a viral respiratory panel, regardless of presenting symptoms or apparent triggers. Once microbiologic testing is performed, antibacterial therapy geared towards the agents of community-acquired pneumonia . A cephalosporin, e.g., ceftriaxone with a macrolide, e.g. azithromycin is the preferred therapy over a fluoroquninolone given its anti-inflammatory properties in asthma. However, there is no clinical data to support this choice over a fluoroquinolone. In the Fall and Winter months, anti-influenza therapy with oseltamivir should be administered at 150;mg twice daily. Antibacterial and antiviral agents should be continued for at least 48;h until an alternative trigger is determine and cultures return without a specific agent. If microbiologic studies return with an agent, therapy should be tailored to that agent only.
Acute Exacerbations Of Chronic Obstructive Pulmonary Disease
Similar to asthma exacerbations, most AECOPDs are caused by common respiratory viruses . Because vitamin D-mediated immune mechanisms appear to play a role in the prevention of viral ARI, vitamin D supplementation might be helpful against AECOPD. However, AECOPD is a more complicated phenomenon than asthma exacerbation. For starters, AECOPD often involve both viruses and bacteria . Moreover, the typical COPD patient is older and more likely to suffer from other relevant smoking-related comorbidities, such as cardiovascular disease . Nevertheless, the question remains: does vitamin D supplementation lower the risk of AECOPD?
In 2012, Kunisaki and colleagues analyzed data from an azithromycin trial of exacerbation-prone patients with COPD to examine the longitudinal association between baseline 25D levels and risk of AECOPD over 1 year . Contrary to their hypothesis, baseline 25D levels were unrelated to risk of AECOPD in their observational study of this high-risk population. Similarly null findings were reported in a 2014 study by Puhan and colleagues from the Netherlands and Switzerland and in the previously cited 2015 study by Persson and colleagues in Norway . Taken together, these observational studies do not support a role for vitamin D supplementation in the prevention of AECOPD.
Recommended Reading: How To Help Someone With Asthma Without An Inhaler
Table 1 Inflammatory Cells Involved In Asthma
National Heart, Lung, and Blood Institute. Expert panel report 3 : Guidelines for the diagnosis and management of asthma Full Report 2007; pg 16-18; Kraft M. N Engl J Med. 2011;365:1141-1144; Berger A. BMJ. 1999;319:90.
Medications that block interleukins are under investigation right now.10,11 These medications may be helpful for people with moderate to severe asthma and high eosinophil levels.
Recommended Reading: Athletically Induced Asthma
Role Of Chlamydia Pneumonia And M Pneumonia In Aeba
Both C. pneumonia and M. pneumonia have been shown to be the cause of URIs, pneumonia, and acute exacerbations of chronic bronchitis. Their role in AEBA and critical asthma syndrome has not been definitively established. Lieberman et al. demonstrated evidence of acute infection with M. pneumoniae in 18 patients hospitalized for AEBA compared with 3;% in control group. In 10 of these patients, however, there was evidence of infection with at least one additional pathogen , thus their impact is confounded by this co-infection .
Several other studies have implicated chlamydia infection in more serious AEBA. C. pneumoniae has been identified as a single agent in 19 of 58 patients with acute exacerbation of asthma and the presence of CP IgG or IgA titers was fourfold higher in patients with acute asthma when compared to controls . The severity of AEBA has also been shown to be much more severe with C. pneumoniae and M. pneumoniae. Functional impairment on hospital admission, persistent reduction in FEV1, and the proportion of patients with severe AEBA were greater in the group with atypical infections compared to groups without atypical infections . None of the patients in this study met criteria for critical asthma syndrome.
Read Also: What To Do For Asthma Attack Without Inhaler
