Expanding Access To Intensive Self
Teaching people how to manage asthma on their own is one of the most important parts of controlling the disease nationwide. Everyone with asthma should develop an individualized asthma action plan with a doctor. In general, people with asthma arent getting action plans from their doctors. Intensive asthma self-management education can improve asthma symptom control for individuals whose asthma is not well-controlled with medical management based upon the NAEPP Guidelines.
Dont Miss: Nasal Inhaler Recipes
How Different Lung Diseases Affect The Lung
An analysis of how different lung diseases affect the lungs functionsThe lungs are essential respiratory organs in humans which enable us to breathe. Our lungs are specialised structures that allow us to exchange gases. We require oxygen from the air to enter our blood, as all cells need it to function. We also need to get rid of carbon dioxide which is a product of many metabolic reactions within our cells. Our lungs allow this gas exchange so we can get rid of carbon dioxide and acquire oxygen
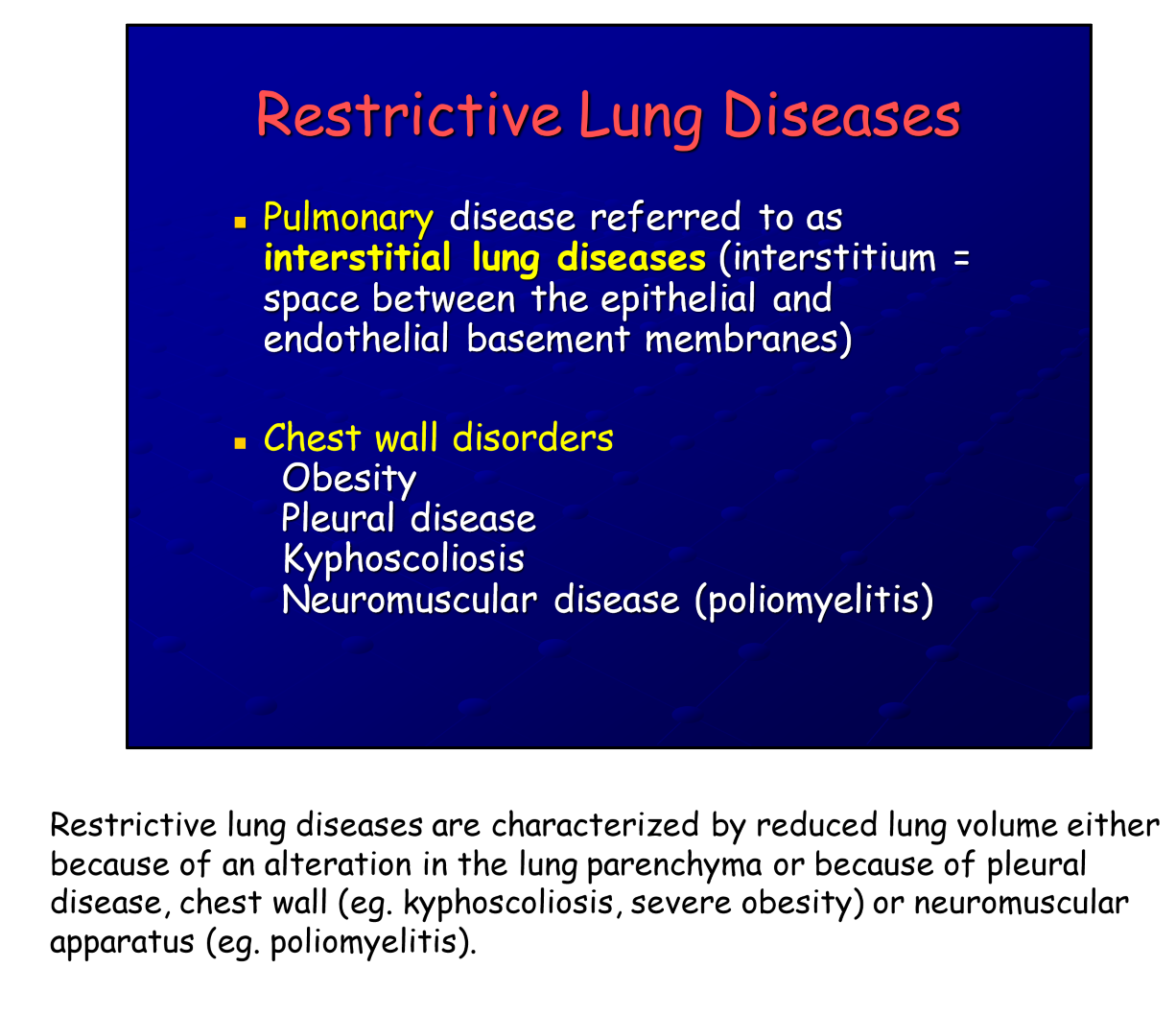
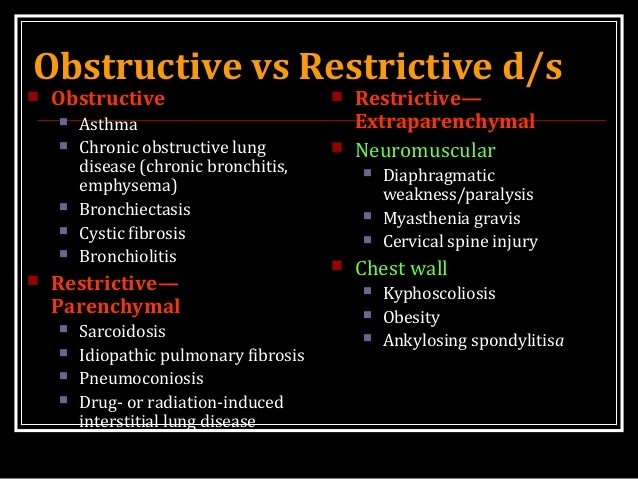
Restrictive Vs Obstructive Lung Diseases
You may be familiar with a common, but serious lung problem known as chronic obstructive pulmonary disease . Instead of making it difficult to breathe in, obstructive lung disease makes it difficult to exhale all the air thats in your lungs. In a way, obstructive and restrictive lung diseases are opposites.
There are four main categories of restrictive lung disease:
- pulmonary: relates to the health and functioning of the lungs
- thoracoskeletal: relates to the bones that make up the ribs and the sternum
- neurologic/neuromuscular: relates to the nervous system, including how the nerves affect muscle function
- abdominal: relates to organs, such as the diaphragm, and other parts that make up your midsection
Some medications, such as corticosteroids and expectorants, are used for both obstructive and restrictive lung diseases. People with either condition can use oxygen therapy.
Don’t Miss: Join The Military With Asthma
Basis And Quality Of Data
Irritant-induced obstructive airways diseases cannot usually be diagnosed in one clinical visit and, instead, follow-up and/or detailed clinical investigations are necessary. The diagnostic gold standard for OA is SIC using a specific occupational agent in an exposure chamber. SIC is particularly indicated in the clinical setting where new causative substances with still unknown adverse respiratory sensitization potential are suspected. This gold standard is not applicable for large studies so, it was used mainly in case series or reports.The evidence levels to confirm irritant-induced work-relaated asthma or occupational COPD for the listed irritant agents, professions or worksites are frequently low with the major reasons being that high quality studies were missing and the quality of the available studies was low. Nevertheless, this knowledge is the best available and may help physicians to identify a suspected irritant agent as causative in irritant-induced work-related asthma and / or occupational COPD. As also recently stressed by Quint et al., implementing an evidence-based identification and regulatory process for OA will help to ensure primary prevention of OA. In cases of low evidence level of an agent that does not exclude a causative role, caution should be exercised and a more detailed diagnostic testing of relevant exposure should be performed.
You May Like: How To Get Rid Of Asthma Without Inhaler
Pulmonary And Respiratory Muscle Function
Restrictive lung disease may be seen in patients with AS. Mild reductions in TLC and VC may be related to disease activity and duration, to spinal and rib cage immobility, or to concomitant kyphosis.100,105 Kyphosis may develop in up to 50% of patients with long-standing AS due to either advanced disease or osteoporosis.106 Kyphosis may be worsened and respiratory function further impaired by fractures involving the rigid spine .107 Patients with AS are also at risk for respiratory failure if cervical spine fractures cause tetraplegia.
Respiratory muscle strength and endurance may be reduced in AS. Pimax and Pemax may be mildly reduced and respiratory muscle endurance may be impaired even in individuals with normal respiratory muscle strength.100,108,109 Mild reductions in strength and endurance may be related to intercostal muscle atrophy secondary to decreased rib cage mobility101 or to poor coordination of the respiratory muscles.110
Scott E. Evans, … Bruce H. Culver, in, 2008
Don’t Miss: Does Allergies Cause Asthma
Causes Of Restrictive Lung Disease
This condition often results from disorders that cause lung stiffness. In other cases, weak muscles, stiffness of the chest wall or damaged nerves could be causing the lung expansion restriction.
You can categorize restrictive lung diseases as intrinsic or extrinsic.
Intrinsic disorders come from an issue within the lungs themselves. They might include:
- Pulmonary fibrosis
- Pleural Effusion
Q: How Is Acos Treated
Your provider can begin treatment if you have COPD or asthma alone. But if you have ACOS, you may want to see a pulmonologista specialist in lung health. People with ACOS often experience more severe symptoms than those with a single lung disease, but working with a specialist can help you feel better. Treatment for ACOS usually includes medicine.
Don’t Miss: What Can Cause Asthma Exacerbation
Staging And Treatment Of Asthma
The goals of long-term management of asthma should include the following: 1) achievement and maintenance of control of symptoms 2) prevention of asthma exacerbations 3) maintenance of pulmonary function as close to normal levels as possible 4) maintenance of normal activity levels, including exercise 5) avoidance of adverse effects from asthma medications 6) prevention of the development of irreversible airflow limitation and 7) prevention of asthma mortality.
The recommended GINA treatment algorithm, together with the clinical features and staging of severity of asthma, are available on the GINA website . It is important to note that the forced expiratory volume in one second levels are before treatment, i.e. in the unmedicated state.
Until the advent of anti-inflammatory drugs, asthma was treated on an as-needed basis and treated as an acute disease rather than a chronic disease. With the recognition that asthma is a chronic inflammatory disease, there has been a gradual move towards treating it more aggressively and earlier in the hope that this may change the natural history of asthma and prevent some of the remodelling that sometimes occurs.
How To Diagnose Restrictive Lung Disease
A pulmonary function test is typically ordered to evaluate total lung capacity or how much air a person’s lungs take in when they inhale. The TLC is typically reduced in patients with restrictive lung disease.
Other testing might be needed for a complete diagnosis and to effectively tailor a proper treatment plan. Additional pulmonary function tests are used for determining if the restrictive lung disease is extrinsic or intrinsic.
Read Also: Inflammatory Mediators In Asthma
Confirm The Restrictive Pattern
If the patient’s initial PFT results indicate a restrictive pattern or a mixed pattern that is not corrected with bronchodilators, the patient should be referred for full PFTs with DLCO testing. DLCO is a quantitative measurement of gas transfer in the lungs. Diseases that decrease blood flow to the lungs or damage alveoli will cause less efficient gas exchange, resulting in a lower DLCO measurement.
During the DLCO test, patients inhale a mixture of helium , carbon monoxide , oxygen , and nitrogen 12 then hold their breath for 10 seconds before exhaling. The amounts of exhaled helium and carbon monoxide are used to calculate the DLCO. Carbon monoxide is used to estimate gas transfer instead of oxygen due to its much higher affinity for hemoglobin. A baseline hemoglobin level should be obtained before DLCO testing because results are adjusted for the hemoglobin level.
Full PFTs provide the patient’s total lung capacity. The restrictive pattern is confirmed as a true restrictive defect if the total lung capacity is less than 80% of predicted in patients five to 18 years of age, or less than the LLN in adults. If full PFTs cannot be obtained, the FVC can be used to infer a restrictive defect however, FVC has a poor positive predictive value.13,14
Common Tests To Diagnose Obstructive And Restrictive Lung Disease Include:
- Forced vital capacity testing. This involves inhalation and filling the patient’s lungs with as much air as they can, then having them exhale with force. The FVC for patients with restrictive lung diseases is usually reduced. An 80% or less FVC value of what’s expected can indicate a restrictive disease.
- Forced expiratory volume in 1 second testing. This testing measures how much air is exhaled during the initial FVC testing.
- FVC to FEVI ratio testing. The FVC to FEV1 ratio measures how much air you can exhale in one second forcefully, relative to the total amount you can exhale. In obstructive lung diseases, this measure is reduced, but in restrictive lung diseases, it’s normal. In adults, normal means a 70% to 80% FEV1/FVC ratio and in children normal means 85% or greater.
- X-rays. Chest X-rays create images of the patient’s lung area and chest for evaluation.
- Computed tomography scans. These scans generate more detailed images of the patient’s lung area and chest than X-rays, improving diagnostic utility.
- Bronchoscopy. This entails using a flexible tube with an attached camera to view the lungs and airways.
Waiting for test results can make people anxious and cause frustration. But, there are often several steps involved in making an accurate diagnosis, since a lung disease could be either restrictive or obstructive. Obtaining an official diagnosis is essential since the distinction between these two forms of disease will ensure the patient receives the right treatment.
Read Also: How To Improve Your Lungs With Asthma
Difference Between Asthma And Chronic Obstructive Pulmonary Disease
July 21, 2017 by Rachna C
The respiratory disease which is diagnosed during childhood, resulting in shortness of breathing, dryness of a cough, chest tightening is called asthma. On the other hand, COPD also known as Chronic Obstructive Pulmonary Disease is also one of the respiratory disease, which occurs after the age of 4o, and the condition gets progressively worse with age.
The cells of our body need oxygen to work and grow, and this oxygen is taken by the lungs through the simple process of breathing. Usually, in a day, we breathe 25,000 times a day. But people suffering from any lungs infection experience the problem in breathing.
Lung diseases are one of the most common medical conditions existing in the world. There are many kinds of lungs infections like bronchitis, cystic fibrosis, emphysema, COPD, asthma, pneumonia, tuberculosis, etc. pollutions, infections, allergens, smoking or genetics can be the major cause of all these problems.
In this article, we will mark the vital difference between the two common respiratory disease asthma and the COPD. We will also discuss their causes, symptoms, and treatment.
Recommended Reading: How To Stop An Asthma Attack Without Medication
Enhancing Healthcare Team Outcomes
The management of restrictive lung diseases can often be complex and challenging due to the many diseases that can result in the condition. For a primary care provider, knowing when to refer a patient to a pulmonologist can be extremely beneficial to the patient. Because of the long list of differential diagnoses and the complications of different conditions, a multidisciplinary approach is always recommended. Besides the primary care provider and pulmonologist, the team would also include nurses who would periodically assess the patients as well as internists and intensivists who would provide care in the inpatient setting according to the severity of the patient’s condition.
Cardiology evaluation should be obtained, especially if pulmonary restriction leads to signs of heart strain as it can potentially result in heart failure. Pharmacists are to be part of the team whenever specialty medications, including the newer anti-fibrotic agents, are used. Nutritionists should also be included in cases of obesity, and Neurologists should be involved in cases of neuromuscular disease. Transplant surgeons ought to assess end-stage patients who are candidates for transplant. Palliative and hospice care specialists should also be involved in cases where there is a terminal disease.
Recommended Reading: Is Asthma A Small Airway Disease
What Are Restrictive Diseases
These are diseases that occur outside your airways. The best example I can think of here is pregnancy. Its not a disease, but it certainly does restrict your airways. You have a baby inside you. It grows larger and larger. At some point, it begins to push up on your diaphragm.
It acts to squeeze or restrict your lungs. This makes it so your lungs are less compliant. This means they are unable to fully expand because of the baby taking up space. So, thats the most basic form of a restriction.
Obstructive diseases make it hard to exhale. Restrictive diseases make it hard to inhale. They cause less lung compliance. Another good example is kyphoscoliosis. People with this have deformed chest walls. This acts to limit the ability of the lungs to expand. Rheumatoid arthritis may also qualify.1,4,5
Neuromuscular diseases like ALS may impact inspiratory muscles. So, this can make it hard to inhale. Drug overdoses qualify here. They relax you so you weaken your drive to inhale.1,3
Pneumonia is inflammation of your alveoli. So, it takes up space making it hard to inhale. Obesity certainly may cause less room for lungs to expand, so it qualifies. Lung cancer takes up space outside airways, so it qualifies. 5
Chronic Obstructive Pulmonary Disease
COPD occurs when the airflow in the lung is obstructed, thus interfering with normal breathing. Modern medicine includes chronic bronchitis and emphysema as sub-types of COPD.
If you are a smoker, we want you to remember that you are joining a high-risk group for this condition. Whether you are an avid cigarette smoker, or if you just have a few once in a while, smoking is still the prime cause of this disease.
Read Also: Is Asthma A Small Airway Disease
Occupational Copd An Underestimated Category
We identified only 20 out of 474 publications that referred to occupational COPD, with most of them implicating inorganic or organic dust or fumes, such as cement dust, construction work and diesel exhaust, as the causative agents.
As an example, the mixed agent cement dust was investigated in 14 studies but only four studies documented cement dust as the causative agent in occupational COPD . The remaining 10 studies described irritant-induced OA cases or identified significant asthma symptoms/ obstructive ventilation patterns without a clear diagnosis . It can be assumed that if it had been considered on the other 10 studies then occupational COPD caused by cement dust would have been frequently observed.
General acceptance of this statement does not exist, although evidence for an association between individual exposure levels and COPD is accumulating in the latest literature.
A Stepwise Approach To The Interpretation Of Pulmonary Function Tests
JEREMY D. JOHNSON, MD, MPH, Tripler Army Medical Center, Honolulu, Hawaii
WESLEY M. THEURER, DO, MPH, Madigan Army Medical Center, Fort Lewis, Washington
Am Fam Physician. 2014 Mar 1 89:359-366.
Pulmonary function tests are useful for diagnosing the cause of unexplained respiratory symptoms and monitoring patients with known respiratory disease. Many organizations, including the National Asthma Education and Prevention Program, Global Initiative for Chronic Obstructive Lung Disease , and American Thoracic Society , recommend using these tests.13 Office equipment required to perform PFTs includes a computer, PFT software, pneumotach, printer, disposable mouthpiece, disposable nosepiece, and a 3-L syringe for calibration. There is no difference between PFT measurements obtained in the office and those obtained in a pulmonary function laboratory, as long as trained personnel calibrate, administer, and interpret the results.
PFTs take approximately 15 minutes for adults, 15 to 30 minutes for children, 45 minutes for pre- and postbronchodilator testing, and one hour for full PFTs with diffusing capacity of the lung for carbon monoxide testing. Five years is usually the youngest age at which children are able to cooperate with PFT procedures.1 Some PFT software will interpret the patient’s results automatically, but these machines should be used with caution because they may not follow current guidelines.
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Figure 1.
Figure 1.
You May Like: What Happens If The Military Finds Out You Have Asthma
Treatment Options For Obstructive Vs Restrictive Lung Disease
Treatment options will be somewhat different for these two types of respiratory illness.1 With obstructive lung disease, the goal is to reduce inflammation and relax the airways. So, treatments might include bronchodilators and/or inhaled steroids. Some medications are long-acting and some are shorter-acting.1
In addition, with COPD, supplemental oxygen therapy might be helpful. This is not generally prescribed in people who have asthma. Changes in lifestyle may also be helpful. For example, with asthma, learning to avoid your triggers can help keep your asthma under control.1
With restrictive lung disease, the treatment options are often more limited. They may also vary greatly, depending on the specific type of restrictive disease. Steroids and bronchodilators are sometimes used. Medications that suppress the immune system may also be helpful.1 Other options might include supportive oxygen therapy and even lung transplants.1
Grade The Severity Of The Abnormality
If an obstructive defect, a restrictive pattern, or a mixed pattern is present, as defined by steps 1 and 2, the physician should grade the severity of the abnormality based on the FEV1 percentage of predicted. The ATS system for grading the severity of a PFT abnormality is summarized in Table 3.3
American Thoracic Society Grades for Severity of a Pulmonary Function Test Abnormality
| Severity |
|---|
|
< 35 |
FEV1 = forced expiratory volume in one second.
Adapted with permission from Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005 26:957.
American Thoracic Society Grades for Severity of a Pulmonary Function Test Abnormality
| Severity |
|---|
|
< 35 |
FEV1 = forced expiratory volume in one second.
Adapted with permission from Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005 26:957.
Read Also: Asthma And Essential Oils
