What Are The Treatments For Asthma
If you have asthma, you will work with your health care provider to create a treatment plan. The plan will include ways to manage your asthma symptoms and prevent asthma attacks. It will include
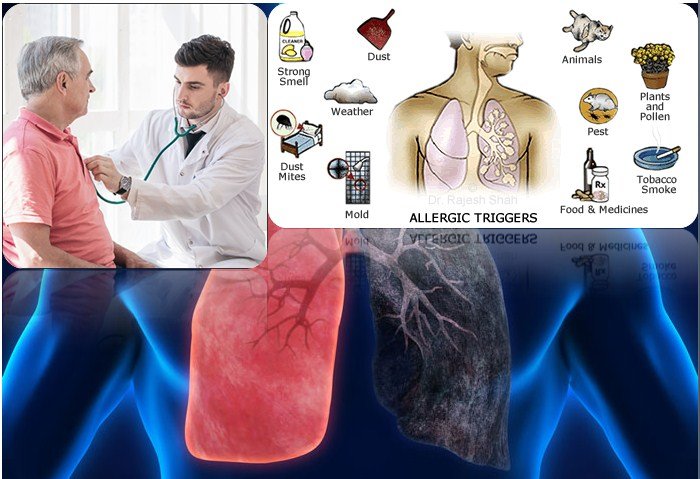
- Strategies to avoid triggers. For example, if tobacco smoke is a trigger for you, you should not smoke or allow other people to smoke in your home or car.
- Short-term relief medicines, also called quick-relief medicines. They help prevent symptoms or relieve symptoms during an asthma attack. They include an inhaler to carry with you all the time. It may also include other types of medicines which work quickly to help open your airways.
- Control medicines. You take them every day to help prevent symptoms. They work by reducing airway inflammation and preventing narrowing of the airways.
If you have a severe attack and the short-term relief medicines do not work, you will need emergency care.
Your provider may adjust your treatment until asthma symptoms are controlled.
Sometimes asthma is severe and cannot be controlled with other treatments. If you are an adult with uncontrolled asthma, in some cases your provider might suggest bronchial thermoplasty. This is a procedure that uses heat to shrink the smooth muscle in the lungs. Shrinking the muscle reduces your airway’s ability to tighten and allows you to breathe more easily. The procedure has some risks, so it’s important to discuss them with your provider.
Whats An Asthma Attack
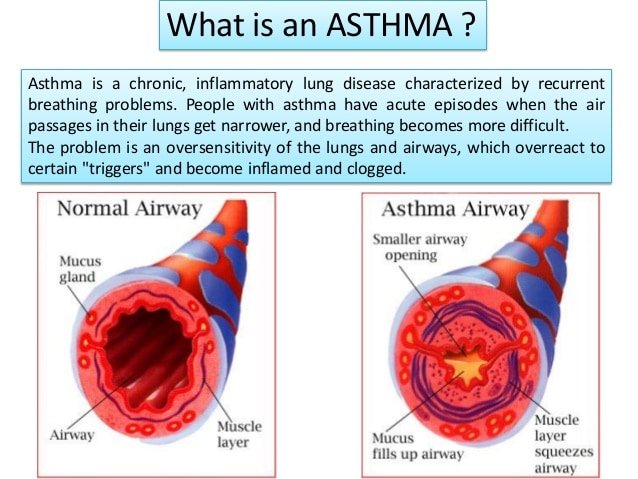
When you breathe normally, muscles around your airways are relaxed, letting air move easily. During an asthma attack, three things can happen:
- Bronchospasm: The muscles around the airways constrict . When they tighten, it makes the airways narrow. Air cannot flow freely through constricted airways.
- Inflammation: The airway linings become swollen. Swollen airways dont let as much air in or out of the lungs.
- Mucus production: During the attack, your body creates more mucus. This thick mucus clogs airways.
Testing And Diagnosis Of Asthma
Your child’s asthma specialists will first look for classic asthma symptoms. It’s important to know that not everyone with asthma will have wheezing. This is a common reason for failure to diagnose asthma. Also, when the airways get very narrow and tight, wheezing may stop. When this happens, the patient is worse, not better. Using “wheeze” alone to diagnose and follow asthma attacks can be unreliable and tricky.
Your asthma specialist will also look at how your child’s symptoms cause a typical pattern of problems. Do they come in cycles or attacks? Do asthma medicines help relieve the symptoms? Sometimes this provides your asthma provider with enough information to make the diagnosis.
We will also check for other conditions that might look like asthma. For example, we will evaluate your child for cystic fibrosis, disorders of the immune system and others if your child’s history and lung function tests hint that other problems might be present.
Don’t Miss: How To Make A Homemade Inhaler For Asthma
Continue Learning About Asthma
Important: This content reflects information from various individuals and organizations and may offer alternative or opposing points of view. It should not be used for medical advice, diagnosis or treatment. As always, you should consult with your healthcare provider about your specific health needs.
What Is Niehs Doing
NIEHS conducts and supports asthma research from basic studies in laboratories to human clinical trials. This research focuses on complex relationships among the environment and peoples genetics and immune system. Projects include:
- Development of sensors that measure personal environmental triggers of asthma.
- Clinical trials that examine if reduced indoor air pollution can improve asthma symptoms.
- Data science methods that combine environmental data gathered across the United States.
Join an asthma study!
The goal of the Natural History of Asthma with Longitudinal Environmental Sampling study is to help scientists understand how bacteria and other factors in the environment affect people who have moderate to severe asthma.
Who can participate?
- Moderate to severe asthmatics.
- Males and females, aged 18-60.
- Females should not be pregnant or breastfeeding at the start of the study, but may still participate if they become pregnant during the study.
- Nonsmokers who are also not around significant amounts of secondhand smoke.
- No history of chronic obstructive pulmonary disease, emphysema, cystic fibrosis , pulmonary fibrosis, non-CF bronchiectasis, sarcoidosis, unstable angina, or pulmonary hypertension.
- Not allergic to methacholine.
- Able to provide your own transportation to clinic visits on the NIEHS campus in North Carolina. For more information about this study:
- NHALES: Asthma Study
You May Like: What Happens If You Smoke Weed With Asthma
What Is An Asthma Action Plan
Your healthcare provider will work with you to develop an asthma action plan. This plan tells you how and when to use your medicines. It also tells you what to do if your asthma gets worse and when to seek emergency care. Understand the plan and ask your healthcare provider about anything you dont understand.
People With Depression Are At Higher Risk For Other Medical Conditions
It may come as no surprise that adults with a medical illness are more likely to experience depression. The reverse is also true: People of all ages with depression are at higher risk of developing certain physical illnesses.
People with depression have an increased risk of cardiovascular disease, diabetes, stroke, pain, and Alzheimer’s disease, for example. Research also suggests that people with depression may be at higher risk for osteoporosis. The reasons are not yet clear. One factor with some of these illnesses is that many people with depression may have less access to good medical care. They may have a more challenging time caring for their healthfor example, seeking care, taking prescribed medication, eating well, and exercising.
Scientists also are exploring whether physiological changes seen in depression may play a role in increasing the risk of physical illness. In people with depression, scientists have found changes in the way several different systems in the body function that could have an impact on physical health, including:
- Increased inflammation
- Changes in the control of heart rate and blood circulation
- Abnormalities in stress hormones
- Metabolic changes such as those seen in people at risk for diabetes
There is some evidence that these changes, seen in depression, may raise the risk of other medical illnesses. It also is clear that depression has a negative effect on mental health and everyday life.
Also Check: Influenza Asthma Exacerbation
Asthma And Copd: Whats The Difference And Is There A Link
Asthma and chronic obstructive pulmonary disease are lung diseases. Both cause swelling in your airways that makes it hard to breathe.
With asthma, the swelling is often triggered by something youâre allergic to, like pollen or mold, or by physical activity. COPD is the name given to a group of lung diseases that include emphysema and chronic bronchitis.
Emphysema happens when the tiny sacs in your lungs are damaged. Chronic bronchitis is when the tubes that carry air to your lungs get inflamed. Smoking is the most common cause of those conditions .
Asthma gets better. Symptoms can come and go, and you may be symptom-free for a long time. With COPD, symptoms are constant and get worse over time, even with treatment.
Who Is At Risk For Asthma
Asthma affects people of all ages, but it often starts during childhood. Certain factors can raise your risk of having asthma:
- Being exposed to secondhand smoke when your mother is pregnant with you or when you are a small child
- Being exposed to certain substances at work, such as chemical irritants or industrial dusts
- Genetics and family history. You are more likely to have asthma if one of your parents has it, especially if it’s your mother.
- Race or ethnicity. Black and African Americans and Puerto Ricans are at higher risk of asthma than people of other races or ethnicities.
- Having other medical conditions such as allergies and obesity
- Often having viral respiratory infections as a young child
- Sex. In children, asthma is more common in boys. In teens and adults, it is more common in women.
Also Check: Does Weight Gain Make Asthma Worse
How Is Asthma Diagnosed
Your health care provider may use many tools to diagnose asthma:
- Physical exam
- Medical history
- Lung function tests, including spirometry, to test how well your lungs work
- Tests to measure how your airways react to specific exposures. During this test, you inhale different concentrations of allergens or medicines that may tighten the muscles in your airways. Spirometry is done before and after the test.
- Peak expiratory flow tests to measure how fast you can blow air out using maximum effort
- Fractional exhaled nitric oxide tests to measure levels of nitric oxide in your breath when you breathe out. High levels of nitric oxide may mean that your lungs are inflamed.
- Allergy skin or blood tests, if you have a history of allergies. These tests check which allergens cause a reaction from your immune system.
Managing Your Chronic Asthma Condition
No one should be in denial about having asthma. Ignoring the condition can mean living with uncontrolled symptoms, frequent asthma attacks, and complications. Controlling asthma may reduce the need for certain asthma medications. The following steps can be taken to help you cope better with living with asthma:
Don’t Miss: How To Get Rid Of Asthma Without Inhaler
Chronic Lung Diseases Including Copd Asthma Interstitial Lung Disease Cystic Fibrosis And Pulmonary Hypertension
Chronic lung diseases can make you more likely to get severely ill from COVID-19. These diseases may include:
- Asthma, if its moderate to severe
- Chronic obstructive pulmonary disease , including emphysema and chronic bronchitis
- Having damaged or scarred lung tissue such as interstitial lung disease
- Cystic fibrosis, with or without lung or other solid organ transplant
- Pulmonary hypertension
Get more information:
Having HIV can make you more likely to get severely ill from COVID-19.
Get more information:
Therapeutic Responses In Asthma Copd And Overlap Syndrome
A comprehensive review of the available treatments for obstructive airway diseases is beyond the scope of this article however, it is important to appreciate that the nature of the underlying inflammation differs between asthma and COPD, as does the response to different classes of medications. Although specific interventions vary by disease, the treatment goals of asthma and COPD are similar and driven primarily by patient-centered outcomes such as controlling symptoms, optimizing health status and quality of life, and preventing exacerbations .
In general, therapies for COPD have a much more limited effect compared with those for asthma. While inhaled corticosteroids are the cornerstone of the pharmacologic management of patients with persistent asthma, inhaled bronchodilators are the therapeutic mainstay for patients with COPD. There are no disease-modifying medications currently available that can alter the progression of AO in either asthma or COPD. Smoking cessation, however, is an essential component of the successful management of any obstructive airway disease.
Recommended Reading: Can Allergies Cause Asthma Attacks
You May Like: Asthma In Military
Cdcs National Asthma Control Program
NACP was created in 1999 to help the millions of people with asthma in the United States gain control over their disease. The programs goals include reducing the number of deaths, hospitalizations, emergency department visits, school days or workdays missed, and limitations on activity due to asthma. The NACP collects data on state-specific levels to focus efforts and resources where they are needed.
The NACP leads national initiatives and provides state funding for a variety of activities focuses on surveillance, intervention, partnerships and evaluation. The NACP funds states, cities, school programs, and non-government organizations to help them improve surveillance of asthma, train health professionals, educate individuals with asthma and their families, and explain asthma to the public. The program has improved asthma treatment, management, and control in the U.S.
Information On Children And Teens
While children have been less affected by COVID-19 compared with adults, children can be infected with the virus that causes COVID-19 and some children develop severe illness. Children with underlying medical conditions are at increased risk for severe illness compared to children without underlying medical conditions. Current evidence on which underlying medical conditions in children are associated with increased risk is limited. Current evidence suggests that children with medical complexity, with genetic, neurologic, metabolic conditions, or with congenital heart disease can be at increased risk for severe illness from COVID-19. Similar to adults, children with obesity, diabetes, asthma or chronic lung disease, sickle cell disease, or immunosuppression can also be at increased risk for severe illness from COVID-19. One way to protect the health of children is to ensure that all adults in a household are fully vaccinated against COVID-19.
Don’t Miss: What Do You Do When You Have An Asthma Attack
Children And Adolescents With Chronic Illnesses
Children and adolescents with chronic illnesses often face more challenges than their healthy peers in navigating adolescence. Chronic illnesses can affect physical, cognitive, social, and emotional development, and they can take a toll on parents and siblings. These limitations put children and adolescents at higher risk than their healthy peers of developing a mental illness.
Children and adolescents with chronic illnesses experience many forms of stress. Parents and health care providers should be on the lookout for signs of depression, anxiety, and adjustment disorders in young people and their families.
Strategies For Addressing Asthma In Schools
CDCs Strategies for Addressing Asthma in Schools guide provides a compilation of information and resources for implementing asthma programs in schools. Although it was designed for staff in state health departments, school systems with an interest in asthma friendly schools have found it to be useful.
Don’t Miss: Can You Join The Army If You Have Asthma
Tips For Wearing A Face Mask With Asthma
The Public Health Agency of Canada currently recommends that Canadians wear non-medical face masks while in public spaces where physical distancing cannot be maintained such as on public transit, or at the grocery store.
Be sure to check your provincial or territorial authority for up-to-date guidance.
Wearing a face mask is NOT a substitute for physical distancing or frequent handwashing. Wearing a non-medical face mask is an extra measure that can be taken to protect those around you. When worn properly, a person wearing a non-medical mask can reduce the spread of their own infectious respiratory droplets.
Make sure you wear your mask properly. It should cover both your nose and mouth. If your mask gets soiled or wet, be sure to wash and dry it before wearing it again. You can read information about appropriate use of non-medical masks, and how to properly place, remove and clean a non-medical mask from the Public Health Agency of Canada.
The vast majority of people with asthma can wear a non-medical mask safely. If you are unable to wear a non-medical mask without experiencing breathing issues, do not wear a mask. Instead, make sure you are practicing physical distancing by maintaining a 2-metre distance. Schedule an appointment with your healthcare provider as soon as possible to go over your Asthma Action Plan and review your asthma symptoms and control. Your healthcare provider may suggest or ask you to consider other options to protect yourself.
Identify And Manage Asthma Triggers
The change in seasons is a great time for clinicians and Vermonters with asthma to focus on identifying and reducing allergens and irritants that can lead to asthma attacks. Irritating triggers are unique to each person and can include tobacco smoke, outdoor and indoor air pollution like diesel exhaust, fireplace smoke, dust mites, pet dander, and more. The prevalence of asthma in Vermont and other New England states is among the highest in the nation. In 2017, 12% of Vermont adults had asthma, which was the fifth-highest rate in the U.S. In 2017, 7% of Vermont children had asthma. A childs asthma may be worsened by similar triggers as adults including cold air, exercise, dust, strong emotions, flu, and viral infections.
Also Check: Can Allergies Trigger Asthma
Medical Conditions In Adults
- This list is presented in alphabetical order and not in order of risk.
- CDC completed an evidence review process for each medical condition on this list to ensure they met criteria for inclusion on this webpage.
- We are learning more about COVID-19 every day, and this list may be updated as the science evolves.
Additional Demands Of Chronic Illness
As well as needing to find ways to deal with the stress involved with chronic illness, you also need to:
- understand the condition
- know about the treatment and therapy
- maintain trust and confidence in the doctors, especially when recovery isnt possible
- know how to control the symptoms
- maintain social relationships and a strong support network when faced with an uncertain medical future or when symptoms arise
- avoid social isolation.
You May Like: Does Weight Gain Make Asthma Worse
