The 2019 Gina Guidelines For Asthma Treatment In Adults
Emily L. Fedor, BS Pharmacy Studies, PharmD Candidate 2021Western New England University College of Pharmacy & Health SciencesWestern New England University College of Pharmacy & Health SciencesVictoria L. Freniere, BS Pharmacy Studies, PharmD Candidate 2021Western New England University College of Pharmacy & Health SciencesJared Ostroff, PharmD, BCACP, BCGPAmbulatory Pharmacy Anticoagulation CoordinatorClinical Associate ProfessorWestern New England University College of Pharmacy & Health SciencesSpringfield, Massachusetts
US Pharm. 2020 45:18-24.
ABSTRACT: Establishing asthma symptom control using pharmacologic and nonpharmacologic interventions improves quality of life and prevents exacerbations in patients with asthma. The Global Initiative for Asthma 2019 guidelines provide recommendations for asthma treatment organized into five steps that correlate with disease severity. Medication options include inhaled corticosteroids , long-acting beta2 agonists, short-acting beta2 agonists , leukotriene receptor antagonists, and oral corticosteroids. Recent data show unfavorable outcomes for SABAs used alone for as-needed treatment of symptoms of mild asthma. Guideline changes include the use of a low-dose ICS with formoterol for as-needed treatment in adults with mild asthma, or for use whenever a SABA would be used. Appropriate, effective medication regimens combined with counseling on proper inhaler technique will help patients achieve asthma-management goals.
Articles To Date In This Series
-
Subbarao P, Mandhane PJ, Sears MR. Asthma: epidemiology, etiology and risk factors. CMAJ 2009. DOI:10.1503/cmaj.080612.
-
Kaplan AG, Balter MS, Bell AD, et al. Diagnosis of asthma in adults. CMAJ 2009. DOI:10.1503/cmaj.080006.
-
Balter MS, Bell AD, Kaplan AG, et al. Management of asthma in adults. CMAJ 2009. DOI:10.1503/cmaj.080007.
-
Chapman KR, McIvor RA. Asthma unresponsive to usual care. CMAJ 2009. DOI:10.1503/cmaj.090089.
Aims Of The Guidelines
The most recent guidelines by the Société de réanimation de langue française for severe acute asthma in adults date from 2002. In view of therapeutic advances in noninvasive ventilation and high-flow oxygen therapy, recent international guidelines and the need to optimize practices , it seemed necessary to summarize current data. In this context, the Société française de médecine durgence and the SRLF propose these expert guidelines on the management of severe asthma exacerbation.
Read Also: What Happens If You Smoke Weed With Asthma
Inhaled Corticosteroids And Long
In patients with poorly controlled asthma and a history of prior asthma exacerbations, the combination of budesonide and formoterol significantly reduces asthma exacerbations compared with ICS alone. ICS/LABA have consistently been shown to prevent exacerbations., , The benefit of ICS/LABA to prevent exacerbations versus ICS alone is primarily seen in patients requiring higher doses of ICS, thus suggesting that combination therapy to prevent exacerbations should be reserved for patients with more severe disease.
Asthma control can vary even in the face of ongoing ICS/LABA treatment. Consequently, the use of ICS/LABA combinations both for maintenance and symptom relief has been investigated and shown to reduce exacerbations., , These benefits are also seen in children with a prior history of severe asthma exacerbations and poorly controlled moderate-to-severe persistent asthma despite the use of moderate doses of ICS. The use of ICS/LABA as maintenance and reliever treatment should be restricted to formoterol because of its quick onset of action, safety profile, and dose-response effect.
The Treatment Of Asthma: Where Are We Evolution Of A Concept
Asthma control medications reduce airway inflammation and help to prevent asthma symptoms among these, inhaled corticosteroids are the mainstay in the treatment of asthma, whereas quick-relief or rescue medicines quickly ease symptoms that may arise acutely. Among these, short-acting beta-agonists rapidly reduce airway bronchoconstriction .
National and international guidelines have recommended SABAs as first-line treatment for patients with mild asthma, since the Global Initiative for Asthma guidelines were first published in 1995, adopting an approach aimed to control the symptoms rather than the underlying condition a SABA has been the recommended rescue medication for rapid symptom relief. This approach stems from the dated idea that asthma symptoms are related to bronchial smooth muscle contraction rather than a condition concomitantly caused by airway inflammation. In 2019, the GINA guidelines review introduced substantial changes overcoming some of the limitations and weaknesses of the previously proposed stepwise approach to adjusting asthma treatment for individual patients. The concept of an anti-inflammatory reliever has been adopted at all degrees of severity as a crucial component in the management of the disease, increasing the efficacy of the treatment while lowering SABA risks associated with patients tendency to rely or over-rely on the as-needed medication.
Fig. 1
Recommended Reading: How To Treat Asthma Without Inhaler
What Are The Peak Flow Zones
Once you know your personal best peak flow number, your doctor will give you a range of numbers that tell you what to do. The peak flow numbers are put into a chart with zones that are set up like a traffic light. It is easiest if these target zones are added to your Asthma Action Plan. This will help you know what to do when your peak flow number changes. For example:
Green Zone signals all clear. No asthma symptoms are present. Take your daily controller medicines , as usual.
Yellow Zone signals caution. You should take a quick-relief medicine and check to see if your peak flow returns to the green zone. You may be having an asthma episode that requires an increase in your medicines or the addition of new medicines. Or your overall asthma may not be under control. Your doctor may need to change your Asthma Action Plan. Follow your Asthma Action Plan and seek additional medical care as indicated.
Red Zone signals a medical emergency. You must take your quick-relief medicine right away. Call your doctor immediately if your peak flow number does not return to the yellow or green zone and stay in that zone. If you cannot reach your doctor and your peak flow stays in the red zone, go directly to the emergency room. Your Asthma Action Plan should provide clear instructions.
Patients At Risk For Severe Asthma Exacerbations
Careful consideration should be carried out in patients with risk factors for severe asthma exacerbations. Patients with exacerbations that led to endotracheal intubation, previous admissions to the ICU, a history of multiple hospitalizations in the past year or multiple emergency department visits in the past month, the need of chronic oral corticosteroids use, poor access to health care, and frequent use of rescue inhalers are considered to have increased risk of severe asthma exacerbations and death. Patients with asthma and with these characteristics should be evaluated promptly and treated expeditiously. In addition, a minority of patients with asthma may experience a significant decline in lung function without a change in symptoms. These under-perceivers are at higher risk for near-fatal exacerbations. This article focuses on the approach to manage exacerbations of asthma.
Also Check: Can Weed Cure Asthma
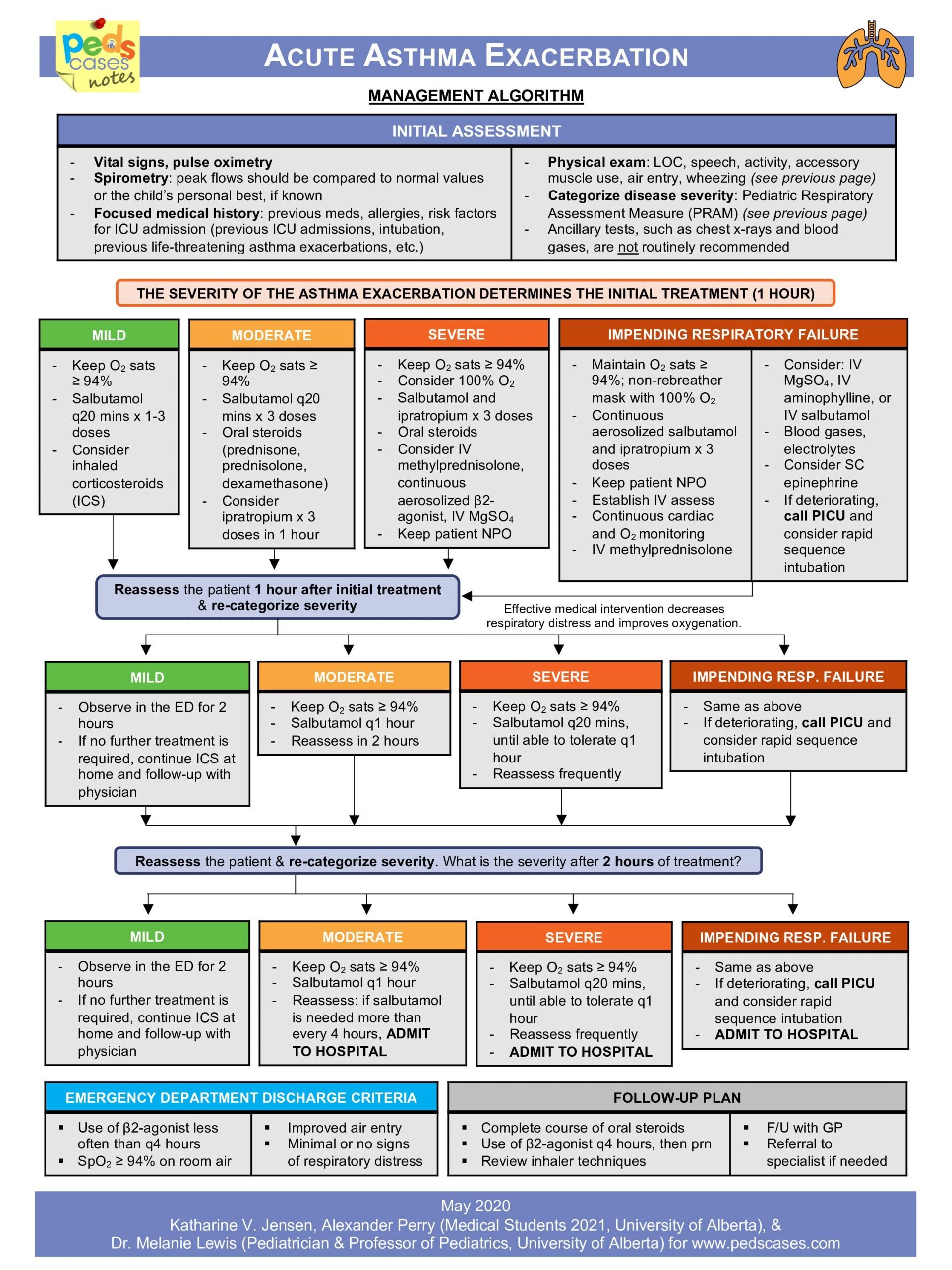
Therapy In The Emergency Department
Patients with mild-to-moderate asthma exacerbations may present to the emergency department to seek medical care. These patients should be treated as an out-patient when following the recommendation detailed above. Patients with severe or life-threatening asthma should always be managed in the emergency department. A focused, expedited history and physical examination should be carried out in all patients. It is critical to rule out other conditions that may mimic a severe asthma exacerbation, such as pneumonia, congestive heart failure, pneumothorax, and myocardial infarction. In patients with a severe exacerbation, careful attention should be placed on the level of consciousness, oxygen saturation, breathing frequency, resting pulse, and blood pressure, and on the use of accessory respiratory muscles. Patients with severe asthma may have a fast deterioration of their clinical presentation, so continuous monitoring of these patients is warranted. In the advanced stages of an asthma exacerbation, the pulmonary physical examination may reveal a silent chest, which may herald impending respiratory failure. Patients with severe asthma should also be monitored for potential complications of asthma, such as pneumothorax, pneumomediastinum, and anaphylaxis.
Discuss Nursing Strategies And Evidence
Your concept map must contain Definition: of the disease, aetiology, pathogenesis, clinical manifestation, diagnosis, course of disease, prognosis, treatment and prevention. Have a look at the attached pathophysiology template for stroke. You must make the concept map using computer, it must be attractive and clear, you can write up to 500 for the map. Please read carefully the assessment details which have the three questions you have to answer. You also have to look at the marking criteria sheet and stick to it. The assessment details also tell you how to make the concept map.
Assessment 2: Concept Map and Guided Question Response
Aim of assessment
The purpose of this assessment is to enable students to:
Explain in visual format the causes, pathogenesis, clinical manifestations, diagnostic procedures, management, course, prognosis and prevention of a severe acute
exacerbation of childhood asthma.
Discuss nursing strategies and evidence-based rationales to manage a child with a severe acute exacerbation of asthma.
Describe the nursing role and responsibilities in the use of pharmacological interventions related to a severe acute exacerbation of asthma.
Details
You are to develop a concept map for the topic severe acute exacerbation of childhood asthma
and answer three questions related to a severe acute exacerbation of asthma. References are to
include at least three recent, relevant journal articles as well as textbook material and evidence based
resources.
Concept map.
Don’t Miss: What Happens If You Smoke Weed With Asthma
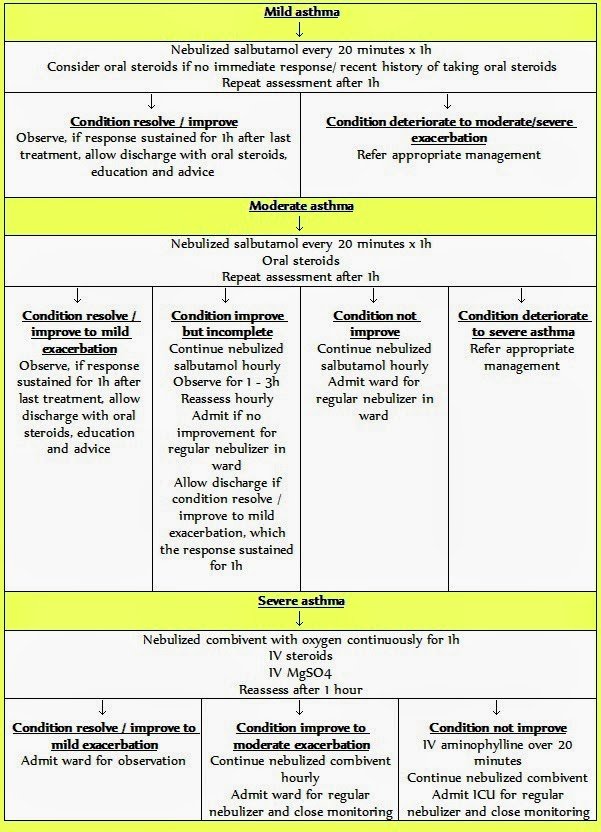
Treatment Of Acute Asthma Exacerbations
, DO, Wake Forest School of Medicine
The goal of asthma exacerbation treatment is to relieve symptoms and return patients to their best lung function. Treatment includes
Corticosteroids Leukotriene modifiers Mast cell… read more .)
Patients having an asthma exacerbation are instructed to self-administer 2 to 4 puffs of inhaled albuterol or a similar short-acting beta-2 agonist up to 3 times spaced 20 minutes apart for an acute exacerbation and to measure peak expiratory flow if possible. When these short-acting rescue drugs are effective , the acute exacerbation may be managed in the outpatient setting. Patients who do not respond, have severe symptoms, or have a PEF persistently < 80% should follow a treatment management program outlined by the physician or should go to the emergency department … read more ).
Complete Blood Cell Count
Cell counts and differentials are commonly requested in the emergency department in the majority of cases of asthma exacerbation. Leukocytosis is common but neutrophilia should be interpreted with caution because beta-agonists and corticosteroids may result in the demargination of white cells and an increase in the peripheral white cell count with a predominant left shift . Recommendations:CBC should not be performed routinely in cases of asthma exacerbation and leukocytosis could be a result of dermargination.
Viral study: It well known that viruses are the main trigger of asthma exacerbation .
Recommendations: Screening for viral illness should be limited to moderate or severe exacerbations or admitted cases, and it may aid in the discontinuation of unnecessary antibiotics .
Read Also: Do Chihuahuas Take Away Asthma
Acute Exacerbation Of Asthma
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Heres our process.
What happens during an acute exacerbation of asthma?
Asthma is a chronic lung disease. It causes inflammation and narrowing of your airways. This can affect your airflow.
The symptoms of asthma come and go. When symptoms flare up and get progressively worse, it can be called:
- an exacerbation
- an episode
- a flare-up
Your airways become swollen during an acute exacerbation. Your muscles contract and your bronchial tubes narrow. Breathing normally becomes more and more difficult.
Even if youve had exacerbations before and know what to do, its still a good idea to contact your doctor. An acute exacerbation of asthma is serious and can even become life-threatening. Thats why its important to recognize the symptoms early and to take appropriate action.
Its important to develop an asthma plan for how to treat your symptoms. Work with your doctor to come up with a method for what to do when your symptoms flare up.
Definition And Importance Of Asthma Exacerbations
The long-term goals for management of asthma are to achieve good control of symptoms, maintain normal activity, and minimize the risk of asthma exacerbation. However, even with optimal care, approximately 10% of patients with asthma will experience a major exacerbation that requires oral corticosteroids, an emergency department visit, or hospitalization once a year.
Exacerbations of asthma are defined as a progressive increase in symptoms of shortness of breath, cough, or wheezing sufficient to require a change in therapy. Usually exacerbations occur in patients with preexisting asthma but can be the first presentation of asthma. Most often, asthma flares or asthma attacks occur as the result of a viral upper respiratory infection, exposure to an allergy, or the result of poor adherence to controller medications.
You May Like: What Happens If You Smoke Weed With Asthma
Fourth Area: Transfer Of Patients
What are the criteria allowing hospital discharge of patients with SAE?
R4.1 adultThe experts suggest that the decision to send patients with SAE home should be based on an assessment taking into account the patients characteristics, the frequency of exacerbations, the severity of the initial clinical presentation, the response to treatment, including the progression of PEF, and the patients ability to be managed at home .
EXPERT OPINION
Rationale
A return home can be envisaged when the symptoms improve after a few hours of treatment in the emergency room. After an hour of continuous treatment with short-acting beta-2 adrenergic agonists, a return home can be envisaged for patients with improved symptoms, no further need for nebulized beta-2 adrenergic agonists, PEF that is 60%80% of the patients theoretical maximum value, pulse oxygen saturation > 94% in ambient air, and a favorable home environment . No study has validated factors predicting readmission of SAE patients.
R4.1 pediatricThe experts are unable to establish pediatric guidelines regarding the decision to send home children admitted for SAE.
EXPERT OPINION
There are no pediatric data on the subject.
Management Of Status Asthmaticus In The Icu
Patients admitted to the ICU include individuals who require ventilator support or those with severe asthma for whom therapy failed. Most often they have refractory hypercapnia, persisting or worsening hypoxemia, deteriorating PEF/FEV1, drowsiness, confusion, or impending signs of respiratory arrest. Elective intubation by an experienced clinician is always recommended as soon as signs of deterioration are present. Intubation and mechanical ventilation may lead to hypotension and barotrauma secondary to high positive intrathoracic pressures. Care must be taken to assure that intravascular volume is adequate before intubation, and a bolus of intravenous normal saline solution is often recommended before initiation of mechanical ventilation.
Although there are no studies that determined the optimal mode of mechanical ventilation, it seems prudent to use the mode with which one is most familiar. Most researchers have recommended an initial minute ventilation of 90130 mL/kg ideal body weight , with further adjustments based on pH and the plateau airway pressure. Based on studies by Tuxen and Lane and Peters et al, we usually use a tidal volume of 89 mL/kg with a breathing frequency of 1014 breaths/min, a flow of 100 L/s, and 0 PEEP. However, many institutions prefer to use tidal volumes of 68 mL/kg ideal body weight., We adjust the setting to maintain a plateau pressure of 30 cm H2O and judiciously adjust ventilator-applied PEEP based on its ability to lower intrinsic PEEP.
Don’t Miss: Back Pain And Asthma
Whats The Outlook For People With Asthma
Most people with asthma are able to manage symptoms and maintain a good quality of life.
An acute exacerbation of asthma can be a life-threatening event. However, you should be able to resume your normal activities once its under control. Of course, youll want to avoid known triggers and follow your doctors advice for management of your asthma.
If you have asthma, you should have an action plan in place. Work with your doctor to come up with a plan so youll know what to do when symptoms flare up.
Initial Assessment And Severity
Acute asthma exacerbation is a medical emergency that should be diagnosed and managed immediately . The treatment of asthma exacerbation depends on the severity of the exacerbation. The assessment of an asthma exacerbation is a continuous process with two different stages: a static assessment to determine the severity of the attack, and frequent assessments to evaluate the response to treatment. Overall, the assessment process requires the analysis of several factors . Different scoring systems exist, such as the Asthma Scoring System or Pediatric Respiratory Assessment Measure . The SINA group adopted the PRAM scoring system as a valid and reliable scoring system for assessing the severity of exacerbation in children aged 217 years . The PRAM score is a 12-point score based on the oxygen saturation, suprasternal retractions, scalene muscle contractions, air entry, and wheezing . The PRAM clinical pathway for inpatient management has been shown to decrease the length of stay in the emergency department and with no adverse outcomes. The SINA expert panel recommends determining the PRAM score for asthmatic patients in the emergency department to categorize the risk of hospital admission .
- Total score of 13: Low risk of hospital admission.
- Total score of 47: Moderate risk of hospital admission.
- Total score of 812: High risk of hospital admission.
Also Check: Can Smoking Weed Cause Asthma Attacks
Second Area: Pharmacological Treatment
What are the methods of administration of beta-2 adrenergic agonists in patients with SAE?
R2.1Beta-2 adrenergic agonists should not be administered intravenously first line in adult or pediatric patients with SAE even in mechanically ventilated patients.
GRADE 1, STRONG AGREEMENT
R2.2Beta-2 adrenergic agonists should probably be administered by continuous rather than discontinuous nebulization during the first hour in adult and pediatric patients with SAE.
GRADE 2+, STRONG AGREEMENT
Rationale
There is no pediatric study that has rigorously compared the efficacy of continuous and intermittent nebulization of short-acting beta-2 adrenergic agonists in children with SAE. Several cohort studies have demonstrated that there is no increase in adverse effects with continuous versus intermittent nebulization .
How Do I Use A Peak Flow Meter
Recommended Reading: How To Make A Homemade Inhaler For Asthma
