Types Of Beta Blockers And The Different Brands
There are different types of beta blockers, depending upon the type of beta receptors they block. These include:
- Non-selective
This blocks the beta1 and beta2 receptors. They affect the heart, blood vessels and the air passages of the lungs.
- Selective
These primarily block beta1 receptors. They mostly affect the heart but not the air passages of the lungs.
Some beta-blockers have intrinsic sympathomimetic activities , meaning they can mimic the effects of epinephrine and epinephrine. Epinephrine is a hormone associated with adrenaline and has the same effects of increasing blood pressure, heartbeat rate, and the like. Beta blockers with ISA have small effects on heart rate than other agents without it. Mainly, beta-blockers can either be non-selective or selective. The selective type mostly affects the heart and the non-selective can affect any part of a persons body. Here are the most widely-used brands and types of beta-blockers:
- Acebutolol
- Propranolol
- Timolol Ophthalmic Solution
What If I Forget To Take It
If you forget to take a dose of your beta blocker, take it as soon as you remember, unless it is nearly time for your next dose. In this case, just leave out the missed dose and take your next dose as normal.
Never take 2 doses at the same time. Never take an extra dose to make up for a forgotten one.
If you often forget doses, it may help to set an alarm to remind you. You could also ask your pharmacist for advice on other ways to help you remember to take your medicine.
Beta Blocker And Ventolin
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
HealthTap doctors are based in the U.S., board certified, and available by text or video.
Recommended Reading: Control Asthma Without Inhaler
Beta Blockers: Are They Safe To Use If You Have Asthma
- Reactions 0 reactions
Traditionally, people with asthma who were on a type of medicine called a beta agonist were cautioned against using a type of heart medicine called a beta blocker. The concern was that these two types of medicine might interact in a way that was harmful to the patient. In this post, I’ll give you the facts about both types of medicine and whether they truly do pose a risk when used together.
Will Aspirin And Other Pain Relievers Make My Asthma Worse
Aspirin and other drugs called nonsteroidal anti-inflammatory drugs may be harmful for people who have asthma. Ibuprofen and naproxen are a few examples of NSAIDs. If you are allergic to aspirin, ask your doctor or pharmacist to make sure any new medicine you might take is not related to aspirin.
People who have asthma can usually take acetaminophen safely. This medicine is typically used to relieve fever and pain. Very rarely, even acetaminophen may make asthma worse, which has prompted further studies to explore the link between acetaminophen and asthma. If acetaminophen makes your asthma worse, tell your doctor. He or she can help you find another type of pain reliever.
Don’t Miss: What’s An Asthma Attack Feel Like
Implications For Clinical Practice
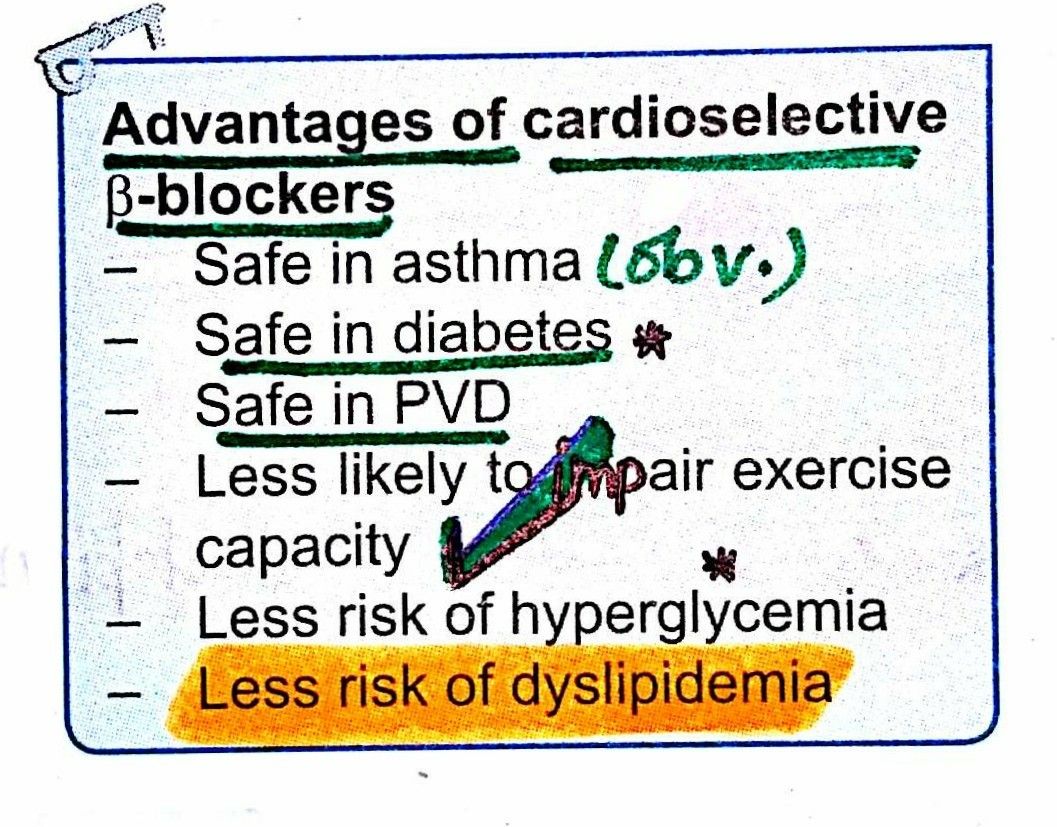
Guidelines have shifted from previously stating that all -blockers are contraindicated in asthma to recommending that prescription of cardioselective 1-blockers should be done under specialist supervision on a case-by-case basis . Nevertheless, concerns over the safety of cardioselective 1-blockers in asthma persist, and this remains a difficult area for prescribers, resulting in underutilisation of -blockers in people with asthma . Clinically there must be a balance of risk and benefit behind each decision to treat a person with asthma with a -blocker as outlined in the recent report from the Global Initiative for Asthma . If there is a clinical indication and perceived clinical benefit from a -blocker for a person with asthma, this review suggests that using highly selective 1-blockers, such as bisoprolol, at the lowest effective dose, is likely to minimise the risk of problematic 2-blocking bronchospasm.
What Is A Beta Blocker
Beta blockers are a type of medicine developed in the 1960s that interfere with the body’s “fight or flight” response to stress.1 In response to stress or danger, your sympathetic nervous system releases adrenaline and noradrenaline. These are hormones that act as chemical messengers. Tiny proteins on the outer surface of many different types of cells called beta receptors sit and wait to latch on to these hormones. They then direct the body to respond in these ways:1,2
- The heart starts to beat faster
- Your blood vessels narrow and tighten
- The airways relax
- You sweat excessively
- Your blood pressure rises
All of those reactions can be useful in people who are in danger or who are responding to stress. But, in those with certain health conditions, such as angina or high blood pressure, those responses can be harmful. That’s where beta blocker medicines come in. They latch on to the beta receptors so that adrenaline and noradrenaline can’t bind to them.
As a result, this happens:2
- Your heart beats more slowly
- Electrical signals in the heart communicate better
- Your blood vessels throughout the body relax
- Blood pressure lowers
Recommended Reading: What Is The Blood Test For Eosinophilic Asthma
How Might The Two Types Of Medicines Interact
In years past, experts were concerned that beta blocker medicines would interfere with how well beta agonists worked. They also feared that beta blockers would cause further constriction of already tight and narrow airway muscles in people with asthma. As a result, doctors were often reluctant to prescribe a beta blocker to a patient with asthma. Obviously, if the patient also had other health conditions that could benefit from a beta blocker, this could be problematic.
Fortunately, there have been many studies that have looked at beta blocker use in people with asthma.3 However most of these studies involved the use of cardioselective beta blockers. Researchers have found that this type of beta blocker presents very limited risk to people with asthma, as long as the recommended doses are followed. This is true even if the person with asthma is on a beta agonist.
Nonselective beta blockers have been found to decrease the response to beta agonists and should not be prescribed for people with asthma, if at all possible.3
Do Not Suddenly Stop Taking Your Beta
Do not suddenly stop taking your beta-blocker without talking to your doctor first. This can be dangerous and make you feel unwell. You may get the feeling of changes in your heartbeat , an increase in blood pressure and a return of chest pains. If you do need to stop taking a beta-blocker then your doctor may advise a slow reduction in dose.
Don’t Miss: Role Of Eosinophils In Allergy
Availability Of Data And Materials
Clinical data, which belong to the Clinical Practice Research Datalink , cannot be made publicly available. Other researchers may extract the data from the CPRD database and replicate the analysis, provided they have appropriate governance procedures and ethical approvals. Interested researchers may contact the CPRD directly to inquire about access to the data.
Use With Respiratory Disease
Beta-blockers can be beneficial to those with lung disease for several reasons:
- They can help maintain optimal blood pressure and heart function, helping you avoid dyspnea .
- COPD is associated with an increased risk of heart failure, which beta-blockers can help treat.
- Heart disease is a leading cause of death among people who have pulmonary disease, and these drugs can reduce that risk.
These benefits, however, must be carefully weighed against notable risks.
Also Check: Does Weight Gain Make Asthma Worse
Precautions One Must Look Out For Before Taking Beta Blockers
Before using beta-blockers, one will need to inform his doctor about your medical history and if you have had any of these conditions:
- Bronchospasm
- Severe peripheral arterial disease including Raynauds syndrome
- Uncontrolled heart failure
The medication can be used by people who have stable heart failures. Patients with blood level problems like diabetes and hypoglycemia should have to keep track of their levels of blood sugar regularly. This is especially important for hypoglycemics or those with low blood sugar levels because beta-blockers may hide the indications of low-blood sugar, such as a rapid heartbeat. Pregnant women can also use beta-blockers but only under their doctors recommendation.
The Benefits Of Taking Beta Blockers
Beta-blockers are primarily known to help the heart slow down in times of distress or lower the effects of adrenaline hormones, especially on those with heart problems. Aside from these, the drug also has some other health benefits. For instance, beta-blockers can protect the bones of the body by preventing the kidneys from eliminating calcium into the urine. The drug can also block stress hormones like adrenaline, which over time, can cause the thinning of the bones because of a deficiency of calcium. Also, beta-blockers are not the first line of defense against bone-thinning, stronger bones will be an extra benefit when taking the medication. Here are the other benefits of such medications:
Effectiveness. There is substantiated evidence which shows that taking beta-blockers after a heart attack can considerably lower the risk of a repeat attack that can lead to an early death. Also, the chances of living a better and longer life are much greater. Studies have also shown that various beta-blockers function better for various conditions.
Cost. This is good news for the millions of people who depend on beta-blockers. The drug is inexpensive and is available in low-priced generic pharmacies. The choice now depends on which beta-blocker a person needs. The choice will also consider the other medical and cardiovascular conditions as well as the side effects.
You May Like: Cure Asthma Naturally Permanently
Beta Blocker In Asthma
- beta blockers are generally contraindicated in chronic obstructive airways disease and asthma
- note however that there is evidence that cardioselective beta blockers are > 20 times more selective for ß1 than ß2 receptors and should carry less risk of bronchoconstriction in reactive airways disease
- there is evidence that, in patients with COPD, cardioselective beta blockers do not change FEV1 or increase respiratory symptoms
- in a small study on asthmatics, propranolol caused a reduction in lung function, but celiprolol was shown not only to improve spirometry readings, it also inhibits the bronchoconstrictor effects of propranolol
- in mice studies, initial therapy with beta blockers increased airway hyperresponsiveness, whereas longer therapy decreased hyperresponsiveness and seemed to have an anti-inflammatory effect
Notes:
The Risks That Come With Taking Beta Blockers
The only risk involved when taking beta-blockers is that one will be taking them for the rest of his life unless of course, one cannot tolerate them, but that is a rare case. For those with cardiovascular issues, beta-blockers are a blessing, the drug can make them feel better. For some, there may be side effects which are tolerable which can include dizziness, tiredness, and generally feeling down. Again, only a handful will experience these side effects. In case they do, the doctors need to do more because a heart problem generally can cause tiredness.
Recommended Reading: Nebulizer Breathing Treatment Side Effects
Data Source And Population For Pharmacoepidemiological Studies
Data were extracted from the UK Clinical Practice Research Datalink which contains electronic medical record data from > 5 million UK people , , . People with medically treated asthma and ocular hypertension were identified by Read Codes and prescriptions for asthma and ocular hypertension medicines. The cohort consisted of people 18 years of age present in the CPRD between 1 January 2000 and 31 December 2011. Subjects were eligible if they: were permanently registered with a general practice for 1 year were from hospital episode statistics linked practices were defined by the CPRD as being acceptable for use in research had a Read Code for asthma and were issued one or more prescriptions for ocular hypertension medicines.
Beta Blockers In Copd Or Asthma
Many patients with obstructive lung diseases have concomitant conditions such as hypertension, coronary artery disease, or congestive heart failure that necessitate the use of ß blockers. However, review articles and practice guidelines consistently list asthma and COPD as contraindications to ß-blocker use. Only a small proportion of patients with cardiac disease who would benefit from ß blockers currently receive this treatment, mainly due to unfounded fears about their adverse effects. Asthma and COPD have been found to be the comorbid conditions most commonly associated with the withholding of ß blockers in patients with myocardial infarction. Now, with the accumulation of data over the past several years, we can clearly track the transition from myth to evidence concerning the use of ß blockers in patients with obstructive airway disease.
The original evidence of a potential adverse effect of ß blockers in asthma and COPD was based on case reports of acute bronchospasm precipitated by high doses of noncardioselective ß blockers. Despite an absence of evidence beyond these case reports, the concept that ß blockers caused increased bronchospasm and severe asthma exacerbations became dogma. For that reason clinicians tend to avoid the use of ß blockers in patients with cardiac conditions if there was even a remote history of obstructive airway disease.
You May Like: How To Get Rid Of Asthma Without Inhaler
Sensitivity Analyses And Secondary Self
Sensitivity analyses were performed for the primary analysis, namely modelling ICS by dose, excluding cases not originally matched on age, people hospitalised within the risk period , people over the age of 40 years who smoked , and using a complete case analysis and a 30- and 90-day risk window . Furthermore, we evaluated the association between nitrate exposure and risk of asthma exacerbations in the form of a negative control.
As a secondary analysis a self-controlled case series with adjustment for time-varying confounders was performed to further measure the safety of acute cardioselective beta-blocker exposure and the risk of moderate asthma exacerbations . In contrast to the nested case control study, the self-controlled case series is a within-person design whereby the patient acts as their own control, controlling for all fixed-confounders. Incidence rate ratios were calculated using conditional Poisson regression. Full details of the self-controlled case series approach are contained in Additional file .
What Are Alternatives To Using Ace Inhibitors
ACE inhibitors do not cause lung function to decrease.1 Therefore, people with asthma may be able to take these medications if they are necessary. If one ACE inhibitor causes cough, others probably will too.1 Your health care provider may be able to recommend a different type of medication to treat your condition. You may also be able to take medications that reduce coughing.
Also Check: Eosinophil Cationic Protein
The Relationships Between Beta
There are two types of beta-blockers, one can favor, and one can hinder the treatment of asthma and its medications
Beta-blockers are not manufactured equally or with the same properties.
As we mentioned above, there are two types of beta receptors as beta-1 and beta-2 receptors. Some beta-blockers are designed to be selective, only for the beta-1 receptors, to provide a more focused treatment.
This beta-blocker is called cardioselective beta-blockers. They only block the beta-1 receptors, the ones that stimulate the enzymes in the heart. In simple terms, cardioselective beta-blockers will only affect the heart functions.
The other beta-blocker is non-cardio selective, meaning they block both the beta-1 and beta-2 receptors. Blocking the receptors located in the lungs has a potential impact on asthma patients who experience breathing problems.
The lung receptors are responsible for relaxing the airways to make breathing easier. This creates the dilemma of using beta-blockers for patients with asthma and is a topic to be discussed with your doctor.
How Asthma Is Treated

The only first-line treatment for asthma is beta-agonists. These medications are also used for other lung conditions.
These medications are known as bronchodilators because they relax airways that are contracted. The name bronchodilators come from the treatment that this medication provides, which is bronchodilation.
When you experience an asthma attack, it causes an involuntary and sudden contraction of the airways called bronchi and bronchioles, making it hard to breathe.
This is whats called bronchoconstriction. So, asthma patients use bronchodilators, which dilates or opens up airways, relaxing the constriction.
Beta-agonists focus on relaxing the airways, unlike beta-blockers, that focus on the heart and lung beta receptors.
You May Like: How To Get Rid Of Asthma Without Inhaler
Intrinsic Sympathomimetic Activity And Inverse Agonism
Unoccupied -adrenoceptors have a baseline level of activity. Most -blockers not only prevent the binding of catecholamines, but also influence the baseline level of activity of the adrenoceptor . -blockers that cause an increase in baseline receptor activity on binding are described as having intrinsic sympathomimetic activity , also sometimes called weak partial agonist activity . Examples of -blockers with ISA include labetalol and acebutolol . A meta-analysis of -blocker treatment after myocardial infarction found that -blockers with ISA were associated with a higher all-cause mortality compared to -blockers without ISA . Current guidelines suggest avoiding -blockers with ISA for treating cardiovascular disease .
Pictorial representation of -adrenoceptor activity in the presence of background catecholamines, -agonists and -blockers. ISA: intrinsic sympathomimetic activity.
-blockers that cause a decrease in baseline receptor activity are described as inverse agonists, also sometimes called negative intrinsic activity . Examples of inverse agonists include metoprolol, bisoprolol, atenolol, nebivolol, carvedilol, nadolol, propranolol and timolol.
