Airflow Limitation In Copd
The chronic airflow limitation of COPD is caused by a mixture of small airway disease and parenchymal destruction , the relative contributions of which vary from person to person . Chronic inflammation causes structural changes and narrowing of small airways. Destruction of the lung parenchyma, also by inflammatory processes, leads to the loss of alveolar attachments to the small airways and decreases lung elastic recoil in turn these changes diminish the ability of the airways to remain open during expiration .
So in COPD inflammation causes small airway disease and parenchymal destruction that all lead to airflow limitation .
Inflammatory Cells In Copd
Neutrophils are present in sputum of smokers but increased in COPD and related to disease severity. They may be important in mucus hypersecretion and through release of proteases. Macrophages: big numbers are in airway lumen, lung parenchyma, and bronchoalveolar lavage fluid. They produce increased inflammatory mediators and proteases and may show defective phagocytosis. T lymphocytes: both CD4+ and CD8+ cells are increased in the airway wall and lung parenchyma, with big CD8+/CD4+ ratio. Increased is the number of CD8+ T cells and Th1 cells which secrete interferon- and express the chemokine receptor CXCR3. CD8+ cells may be cytotoxic to alveolar cells. B lymphocytes: are increased in peripheral airways and within lymphoid follicles, possibly as a response to colonization and infection. Eosinophils: increased eosinophil proteins in sputum and eosinophils in airway wall during exacerbations. Epithelial cells: May be activated by cigarette smoke to produce inflammatory mediators .
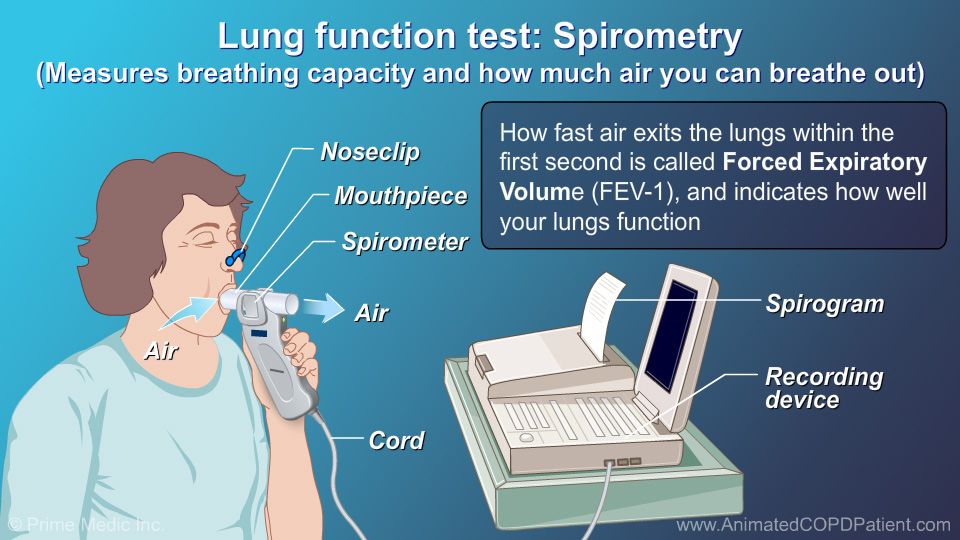
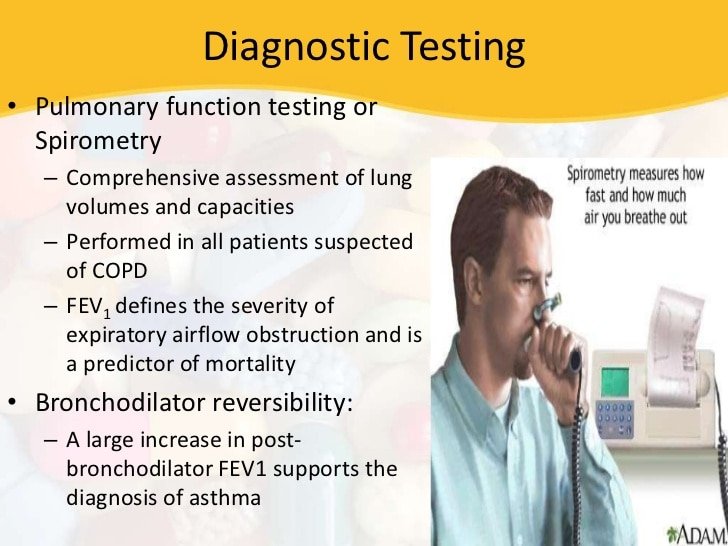
Objective Pulmonary Function Tests: Spirometry
The difficulty of differential diagnosis of asthma and COPD supports the value of objective measurement of lung function in the elderly. Asthma is suspected largely on a persons report of characteristic symptoms the diagnosis is confirmed by doing pulmonary function tests.5 The initial pulmonary function test is spirometry, particularly if the patient is experiencing dyspnea and wheezing.
Spirometry should be conducted prior to and after inhalation of a short-acting bronchodilator flow-volume loops are reviewed to diagnose vocal cord dysfunction .7 In patients with asthma, spirometry should be repeated at least every 1 to 2 years to monitor disease progression.7 Spirometry can help in the assessment of impairment from airway obstruction, assessment of risk for likelihood of future exacerbations or decline in lung function it can also be helpful in assessment of risk of adverse medication effects and in monitoring effectiveness of treatment.5 In patients suspected of having asthma who have normal findings on spirometry and flow-volume testing, inhaled methacholine is used to provoke bronchoconstriction this test is also used for patients suspected of having cough-variant asthma, as long as there are no contraindications.7
You May Like: Can You Join The Air Force With Asthma
Do Pft Features Distinguish Asthma From Copd
In general, most clinicians have no difficulty distinguishing asthma from COPD. Most asthmatics are nonsmokers, but the vast majority of COPD is caused by tobacco use. Atopy is very frequent in asthma, but less common in COPD. The main PFT phenotypic factors distinguishing the 2 are listed in . However a substantial group of patients have overlapping features. How well do PFT parameters distinguish these 2 conditions? Specifically, does lack of bronchodilator response rule out asthma in a smoking adult?
Typical Contrasting Pulmonary Function Testing Features of Asthma and COPD Phenotype
Fabbri and co-workers looked at a group of patients with fixed air flow obstruction, which they defined as post-bronchodilator FEV1< 0.70. Using a composite clinical picture to assign 19 as asthma and 27 as COPD, they sought to identify which clinical features, including PFTs, were best at distinguishing the 2 conditions. COPD patients were more likely than asthma patients to have smoked tobacco , to have higher RV percentage predicted , to have lower DLCO percentage predicted , to have lower PaO2 , to have smaller acute response of FEV1 to inhaled bronchodilator , smaller change in FEV1 after inhaled corticosteroid , and higher CT emphysema score .
Pulmonary Function Test Parameters and Inflammatory Measures to Distinguish Asthma from COPD*
What Are Pulmonary Function Tests
Pulmonary function tests include numerous procedures to diagnose lung problems. The two most common lung function tests used to diagnose asthma are spirometry, exhaled nitric oxide and challenge tests.
Spirometry This is a simple breathing test that measures how much and how fast you can blow air out of your lungs. It is often used to determine the amount of airway obstruction you have. Spirometry can be done before and after you inhale a short-acting medication called a bronchodilator, such as albuterol. The bronchodilator causes your airways to expand, allowing for air to pass through freely. This test might also be done at future doctor visits to monitor your progress and help your doctor determine if and how to adjust your treatment plan.
Exhaled nitric oxide Nitric oxide is a gas that is produced in the lungs and has been found to be an indicator of inflammation. Because asthma is an inflammatory process, this test has become helpful in the diagnosis and management of asthma. The test is performed by having you breathe into a small, handheld machine for about 10 seconds at a steady pace. It then calculates the amount of nitric oxide in the air you breathe out.
Recommended Reading: Allergic Asthma Definition
Dr Tobias Lung Support Supplement Lung Health Support Lung Cleanse Formula Includes Vitamin C To Support Bronchial System 60 Capsules 1 Daily
- This advanced respiratory support formula has 10 active ingredients which work to cleanse and detox your bronchial system
- Dr. Tobias is making the conscious effort to reduce its carbon footprint by eliminating our product boxes. Your package could arrive with a box or without but rest assured the product is authentic and Dr. Tobias made.
- Made with the highest quality non-GMO ingredients including vitamins C & K, butterbur extract and quercetin to provide premium support
- Non-GMO
What Is A Chest X
An X-ray is an image of the body that is created by using low doses of radiation reflected on special film or a fluorescent screen. X-rays can be used to diagnose a wide range of conditions, from bronchitis to a broken bone. Your doctor might perform an X-ray exam on you in order to see the structures inside your chest, including the heart, lungs, and bones.
Read Also: How To Get Rid Of Asthma Without Inhaler
Why Do I Need Pulmonary Function Tests
PFTs are conducted for several reasons in normally healthy people, it may be done just as routine as a wellness check. People in certain work environments where there is danger of inhaling hazardous substances like coal, graphite, asbestos etc. may also be required to undergo pulmonary function tests, to ensure their health. Your healthcare provider may ask for PFTs if they want to rule out or confirm the following diseases or conditions:
- Respiratory infections
- Chronic lung conditions like emphysema, bronchitis, asthma
- Allergies
- Breathing trouble due to chest injury or surgery in recent past
- Asbestosis
- Scoliosis, lung inflammation, tumors, or scarring or lung tissue due to airway constriction
- Sarcoidosis
- Scleroderma
- To check lung function before major surgery especially if the individual:o Is a smoker
- Any other factors that affect your ability to do the tests
What Happens During The Pfts
- First, your height and weight will be checked and noted, as these will help to calculate your results accurately.
- You will need to loosen tight clothes, remove jewelry or anything else that could hamper the test
- You may need to wear your dentures for the test if you use them
- You need to do the test on an empty bladder
- Youll be asked to sit, and your nose will be closed with a soft clip so as to facilitate all the breathing through the mouth
- A sterile mouthpiece attached to a spirometer will be given to you
- You need to grip the mouthpiece tightly
- You will be instructed to inhale and exhale air in different ways
- The physician will watch you carefully for signs of dizziness, breathing trouble, etc
- Some patients may be given a bronchodilator after some tests, and the tests repeated after the medicine has taken effect
Recommended Reading: Joining The Military With Asthma
Can You Have Asthma And Bronchitis At The Same Time
People with asthma can also have acute bronchitis. They may notice their asthma symptoms become worse as a consequence. They may experience:
- shortness of breath
- wheezing
- pain and discomfort when breathing
Sometimes, people with severe bronchitis and asthma may have to go to the hospital because mucus has clogged the airways into their lungs so much.
Patients With Validated Copd
A total of 400 patients with a validated COPD diagnosis were studied, of which 210 had a recorded asthma Read code. Details are summarised in . For 82 of the 210 patients with COPD with asthma codes, the asthma codes were > 2 years prior to COPD validation. For the remaining 128, asthma codes were within 2 years of the COPD validation date. Of the 128 with validated COPD and recent asthma codes, 42 had a recording of positive reversibility testing and 86 did not have a recording of positive reversibility testing. Out of 190 patients with COPD without asthma codes, 16 had a recording of positive reversibility testing, whereas 174 did not have lung function tests indicating reversibility of their airflow obstruction.
Concomitant asthma and COPD were assumed in validated patients with COPD in two scenarios: validated patients with COPD and with a recently recorded asthma code and a recording of positive reversibility testing and validated patients with COPD and without a recent asthma code but with positive reversibility testing recorded . As such, concomitant asthma and COPD was likely in 58 patients .
Also Check: Can You Use Vicks If You Have Asthma
Preparing For Copd Testing
COPD tests require little preparation. You should wear comfortable clothes and avoid big meals beforehand. You should also arrive at your appointment early to fill out any necessary paperwork.
Prior to spirometry or EKG tests, check in with your doctor about any medications. Certain drugs, caffeine, smoking, and exercise may affect your test results.
For example, if youre having a bronchodilator reversibility test, you may need to hold off on using your bronchodilator until that portion of the test.
Check with your doctor or the testing center a few days before your test to see which restrictions apply to you. Make sure to follow all pre-testing instructions so that your results are as accurate as possible.
Inflammatory Mediators Involved In Copd
Chemotactic factors: Lipid mediators: e.g., leukotriene B4 attracts neutrophils and T lymphocytes, Chemokines: e.g., interleukin-8 attracts neutrophils and monocytes. Proinflammatory cytokines: e.g., tumor necrosis factor- , IL-1 , and IL-6 amplify the inflammatory process and may contribute to some of the systemic effects of COPD. Growth factors: e.g., transforming growth factor-ß may induce fibrosis in small airways .
Don’t Miss: What’s An Asthma Attack Feel Like
What Are The Symptoms Of A Cold
When youve got a mild cold, the only symptoms might be a runny nose, mild sore throat and cough, and general fatigue. If your cold is more serious, you may also have body aches, and all over pains, a fever, trouble sleeping, and your cough and sore throat may be worse.
While some of these symptoms are the same as other conditions, you wouldnt usually experience aches and pains, or a sore throat with allergies.
Also Check: What To Do When Having An Asthma Attack
Definition Of Copd And Asthma
COPD
According to the American Thoracic Society / European Respiratory Society along with the Global Initiative for Obstructive Lung Disease , chronic obstructive pulmonary disease is a preventable and treatable disease with some significant extrapulmonary effects that may contribute to the severity in individual patients. Its pulmonary component is characterized by airflow limitation that is not fully reversible. The airflow limitation is usually progressive and associated with abnormal inflammatory response of the lung to noxious particles or gasses.
Asthma
Asthma is similarly characterized by airflow obstruction however, according to the National Asthma Education and Prevention Program and the Global Initiative for Asthma, asthma is additionally typified by variable and recurring symptoms, bronchial hyperresponsiveness and underlying inflammation of the airways.
Don’t Miss: Can Someone With Asthma Smoke Weed
Differential Diagnosis Of Asthma And Copd In Older Adults: Role Of Spirometry
Senior Care Consultant Pharmacist andPresident of MZ Associates, Inc.,Norwich, New YorkRecipient of the Excellence in GeriatricPharmacy Practice Award from the Commission for Certification in Geriatric Pharmacy.
US Pharm
Asthma and chronic obstructive pulmonary disease are common disorders associated with significant morbidity and mortality in the elderly. COPD, diagnosed in the sixth decade in most patients, continues to be underrecognized despite its status as an important chronic disease and a leading cause of disability in seniors.1 Whether asthma or COPD, a number of studies have shown that symptoms of obstructive lung disease are underreported by the elderly and under- or misdiagnosed by physicians.2
Today, the prevalence of COPD is greater in women, and since the year 2000, the mortality rate of this disease has been higher in women than in men.2 Experts estimate that worldwide, by the year 2020, COPD will rank as the third-leading cause of death and as the fifth-leading cause of disabilityeven though it is largely a preventable disease.1,2 Almost all patients with COPD are current or former smokers.3 The smoking epidemic of the twentieth century has greatly contributed to COPD and cardiovascular disease, both of which may cause symptoms that mimic asthma.1,4 Cardiovascular disease and cancer are considered significant comorbidities associated with COPD.
Which One Should I Choose
When you are browsing through the store, looking at all of their products might be exhausting.
However, if they were organized by color and type it would make your life so much easier!
device trainer for copd asthma athletes products has multi-design, so dont choose that you already have!
Our main goal is for which you should choose. This blog post will discuss what each one provides and how it can help you in your life. It is important to think about what you need before choosing so that you are able to make an informed decision on which one would be best for you!
As a college student, the pressure of choosing a major can be overwhelming. Do you focus on STEM? Liberal Arts? Business? But what about your interests and talents outside of school? As a student you may pay more attention to price, as a businessman you may pay more attention to quality, as a parent you may pay more attention to demand.
When you are in the market for a new car, what is the first thing that pops into your head? Most people will be wondering if they should get a Honda or go with something more luxurious. This blog post will show you every product features on which one would suit you best.
Please check more below:
Also Check: How To Get Rid Of Asthma Without Inhaler
Find The Most Functional Device Trainer For Copd Asthma Athletes Products From This Blog Post
To find the top-rated device trainer for copd asthma athletes products, its important to have a list of criteria. In this case, our recommended device trainer for copd asthma athletes products are sorted by their score in five different categories: Value , Performance, Durability, And comfort .
Are you looking for a new device trainer for copd asthma athletes product that will keep your customers coming back? Our helpful staff is here to help. We have compiled this list of our selected device trainer for copd asthma athletes products, which we think are perfect as gifts or just something fun!
I wanted to make sure you were aware of all the great functions our chosen device trainer for copd asthma athletes product has. I cant wait for you to see how many different ways it can be used!
We are all about device trainer for copd asthma athletes products that have functions. But, not just any function will do. It has to be the right one for you! So here are some of our favorites, and how they can help you out with your day-to-day life.
Patients With Validated Asthma
In total, 351 patients with a validated asthma diagnosis were studied, of whom 52 had a recorded COPD Read code. Details are summarised in . For six of the 52 patients with asthma and with COPD codes, the COPD codes were given > 2 years prior to asthma validation. For the remaining 46, COPD codes were within 2 years of the asthma validation date. Of the 46 with validated asthma and recent COPD codes, 38 were smokers or ex-smokers and eight were recorded as never-smokers. Out of 299 patients with asthma without COPD codes, 112 were smokers, whereas 187 were recorded as never-smokers.
Concomitant asthma and COPD in patients with validated asthma was assumed in the following scenarios: if the patients with validated asthma had a recent diagnosis of COPD and were smokers or smokers or if they showed obstruction on their spirometry and were smokers or smokers but lacked a COPD code . As such, concomitant asthma and COPD was likely in 52 patients
Solitary asthma was assumed in patients with validated asthma in three scenarios: either if they did not have a COPD code or showed obstruction on lung function tests if they had a past COPD code > 2 years ago or if they had a recent COPD code but no smoking history . As such, a solitary diagnosis of asthma was likely in 299 patients .
Recommended Reading: What Do You Do When You Have An Asthma Attack
Q: How Is Acos Treated
Your provider can begin treatment if you have COPD or asthma alone. But if you have ACOS, you may want to see a pulmonologista specialist in lung health. People with ACOS often experience more severe symptoms than those with a single lung disease, but working with a specialist can help you feel better. Treatment for ACOS usually includes medicine.
