Setting Your Browser To Accept Cookies
There are many reasons why a cookie could not be set correctly. Below are the most common reasons:
- You have cookies disabled in your browser. You need to reset your browser to accept cookies or to ask you if you want to accept cookies.
- Your browser asks you whether you want to accept cookies and you declined. To accept cookies from this site, use the Back button and accept the cookie.
- Your browser does not support cookies. Try a different browser if you suspect this.
- The date on your computer is in the past. If your computer’s clock shows a date before 1 Jan 1970, the browser will automatically forget the cookie. To fix this, set the correct time and date on your computer.
- You have installed an application that monitors or blocks cookies from being set. You must disable the application while logging in or check with your system administrator.
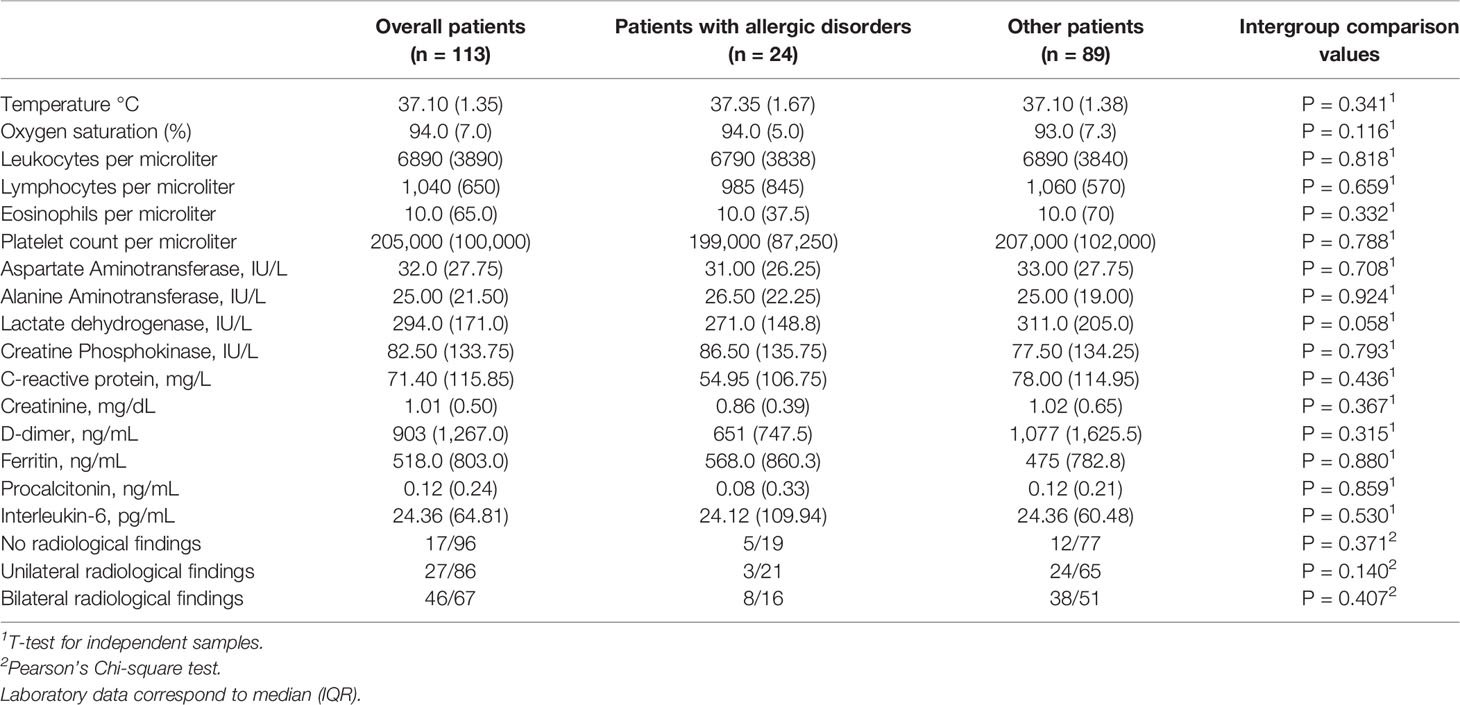
What Laboratory Studies Should You Order To Help Make The Diagnosis And How Should You Interpret The Results
No blood tests define the presence or absence of asthma, and no blood tests are available to stratify asthma by severity. However, a complete blood count , including white blood cell differential analysis, is important in screening for eosinophilia, which can be seen in severe or atypical forms of disorders associated with asthma (e.g., allergic bronchopulmonary aspergillosis or chronic eosinophilic pneumonia. Use of the CBC in screening for anemia also may be helpful in certain cases.
Role Of Eosinophil In Pathogenesis
Eosinophils are granulocytes in blood produced in the bone marrow with other white blood cells making about 13% of white blood cells. Eosinophil plays multiple functions and is an important component of allergic and asthmatic type 2 immune responses. Allergens on exposure starts a group of processes by Th2 cytokine-producing cells, resulting in eosinophils attraction to the airway through the action of IL-5, and eotaxin research reported that Clara cells of the airway epithelium are the main source of eotaxin in the lung .
During asthma attack, eosinophils are stimulated to release proteins from granules including major basic protein, eosinophil peroxidase, eosinophil cationic protein, and eosinophil-derived neurotoxin, all of which are toxic to the epithelial cells of airway. Furthermore, eosinophils secrete plenty of inflammatory mediators like cytokines , platelet-activating factor, growth factors , leukotrienes, thromboxane, and prostaglandins. The secretion of all these mediators results in enhancement of the inflammatory process, airways epithelium cell injury, airway hyperresponsiveness, mucus hypersecretion, and airway remodeling and bronchospasm . Eosinophils control the allergen-dependent Th2 pulmonary immune responses activated by dendritic cells and T cells as well as decrease Th1 responses .
Recommended Reading: Can Asthma Make You Cough
What Imaging Studies Will Be Helpful In Making Or Excluding The Diagnosis Of Asthma
Although the chest radiograph is usually of little specific diagnostic value in asthma, all patients with dyspnea or suspected asthma should have a chest radiograph performed on initial evaluation. The presence of infiltrates, consolidation, pleural effusions, or lung nodules should prompt consideration of alternative diagnoses. The chest radiograph can also be helpful in evaluating patients with severe or atypical forms of asthma, such as ABPA or chronic eosinophilic pneumonia.
Disruption Of Homeostatic Maintenance And Repair System
This hypothesis suggests that there is an intrinsic balance between apoptosis and cell proliferation in the lung, and that vascular endothelial growth factor is central to the stability of this system as a survival signal. The hypothesis suggests that cigarette smoke activation of caspase, ceramide, and oxidative stress acts to induce apoptosis and will ultimately produce emphysema through induction of senescence. This results in cellular dropout and loss of alveolar wall integrity.
This theory also includes speculation as to the role of autoimmunity in induction of both centriacinar and panacinar emphysema. Certainly, there are data that imply that an adaptive immune response is involved in either or both of the genesis and perpetuation of emphysema. Exposure of recognition domains, membrane lipid alteration, and dendritic cell activation can all lead to activation of T cells targeted toward the lung endothelium and/or epithelium.
The lung microbiome appears to be important in the host immune response in COPD. Recently, Sze and colleagues; have found not only that analysis of the microbiome can be used to discriminate between control and severe COPD lung tissue, but they also demonstrated that a decline in microbial diversity correlated with emphysematous lung destruction, airway remodeling, and CD4 T-cell lymphocyte accumulation within the lung.
Read Also: How To Make Asthma Go Away
Role Of Ilcs In Pathogenesis
Innate lymphoid cells are newly discovered immune cells that have lymphoid morphology but deficient in antigen receptor. Type 2 innate lymphoid cells are non-B/non-T cells that release IL-5 and IL-13 on activation by IL-25 and IL-33 and expressed MHC class II high and CD11cdull on their surface. Several studies reported that ILC2 originates from common lymphoid progenitor cells and not from either myeloid or erythroid progenitors, confirming that these cells are of lymphoid origin. ILCs have three different types, ILC1s, ILC2s, and ILC3s, on the basis of identical cytokine profile associated with the helper T subsets Th1, Th2, and Th17, respectively . ILC2s are known to produce type 2 cytokines including IL-4, IL-5, and IL-13 on exposure to allergen, IL-25 and IL-33, and are therefore probable new member in Th2 cell-independent innate type 2 responses. ILC2s can be stimulated by several cytokines especially epithelial cell-derived cytokines IL-25, IL-33, prostaglandin, and leukotriene which have been observed to start ILC2 reaction in both animals and humans .
Symptoms Of An Asthma Attack
Asthma attacks occur most often in the early morning hours when the effects of protective drugs wear off and the body is least able to prevent airway narrowing.
An asthma attack may begin suddenly with wheezing, coughing, and shortness of breath. At other times, an asthma attack may come on slowly with gradually worsening symptoms. In either case, people with asthma usually first notice shortness of breath, coughing, or chest tightness. The attack may be over in minutes, or it may last for hours or days. Itching on the chest or neck may be an early symptom, especially in children. A dry cough at night or while exercising may be the only symptom.
During an asthma attack, shortness of breath may become severe, creating a feeling of severe anxiety. The person instinctively sits upright and leans forward, using the muscles in the neck and chest to help in breathing, but still struggles for air. Sweating is a common reaction to the effort and anxiety. The heart rate usually quickens, and the person may feel a pounding in the chest.
Read Also: What Does Asthma Do To The Body
Fraction Of Exhaled Nitric Oxide
Nitric oxide synthase helps in the synthesis of nitric oxide, a reactive molecule that is shown on cells in airway epithelium. In asthma, FeNO analysis by breath assays is usually treated as an aseptic sign of airway inflammation. FeNO analysis is simple, rapid, and noninvasive in contrast to the bronchoscopy and sputum induction. Significantly, it was shown that FeNO quantification perhaps is helpful as a clinical instrument for administering the asthma and managing the disease, but different findings result in some controversy about FeNO efficacy . In a study, more than 90 asthma patients were examined by Smith et;al., and they identified that FeNO acts as an effective tool for the withdrawal of inhaled corticosteroid treatment. Tseliou et;al. also studied that >19 parts per billion FeNO levels were due to sputum eosinophilia with 78% sensitivity and 73% reactivity in individuals who had mild to acute asthma, while few of them relied on prednisone. Differently, Nair et al. in a clinical trial performed with mepolizumab described that FeNO levels and sputum eosinophil percentages are not associated with asthmatics who relied on prednisone .
How And/or Why Did The Patient Develop Asthma
The etiology of asthma is unknown, but asthma likely results from complex interactions between multiple genetic and environmental variables. Studies of twins and families with asthmatic members have shown that, in many cases, asthma occurs in a pattern consistent with heritable factors. However, at present, the specific genes responsible for asthma have not been definitively identified. Furthermore, the variety of asthma phenotypes, as described previously, may have distinct etiologies, a focus of much ongoing research.
Recommended Reading: How Do You Know If A Child Has Asthma
Understanding Asthma Pathophysiology Diagnosis And Management
A chronic inflammatory airway disorder, asthma is marked by airway hyperresponsiveness with recurrent episodes of wheezing, coughing, tightness of the chest, and shortness of breath. Typically, these episodes are associated with airflow obstruction that may be reversed spontaneously or with treatment.
Asthma affects approximately 300 million people around the world. In children, males have a higher asthma risk; in adults, females have a higher prevalence.
Experts believe asthma results from various host factors, environmental factors, or a combination. Host factors include gender, obesity, and genetics. Genetic factors include atopy. Defined as a genetic tendency to develop allergic diseases, such as asthma and allergic rhinitis, atopy commonly is linked to an immunoglobulin E mediated response to allergens.
Histopathology And Localization Of Mast Cells
Tumor tissues from these patients were fixed with 10% buffered formalin, and after routine dehydration, were embedded in paraffin. Sections 5-μm thick were stained with hematoxylin and eosin and examined under a light microscope. To identify mast cells in each specimen, paraffin sections were stained with toluidine blue. The granules within mast cells contain heparin and sulfated glycosaminoglycan that stain metachromatically with toluidine blue. The 5-μm-thick tissue sections were stained for 30 min with a staining solution containing 0.05% toluidine blue O in a citric acid phosphate buffer and were then examined with light microscopy.
Also Check: How To Prevent Asthma Attacks
The Impact Of Asthma On Daily Life
Asthma is often under-diagnosed and under-treated, particularly in low- and middle-income countries.
People with under-treated asthma can suffer sleep disturbance, tiredness during the day, and poor concentration. Asthma sufferers and their families may miss school and work, with financial impact on the family and wider community. If symptoms are severe, people with asthma may need to receive emergency health care and they may be admitted to hospital for treatment and monitoring. In the most severe cases, asthma can lead to death.
Leicester Researchers Identify Common Biological Features Of Different Types Of Asthma
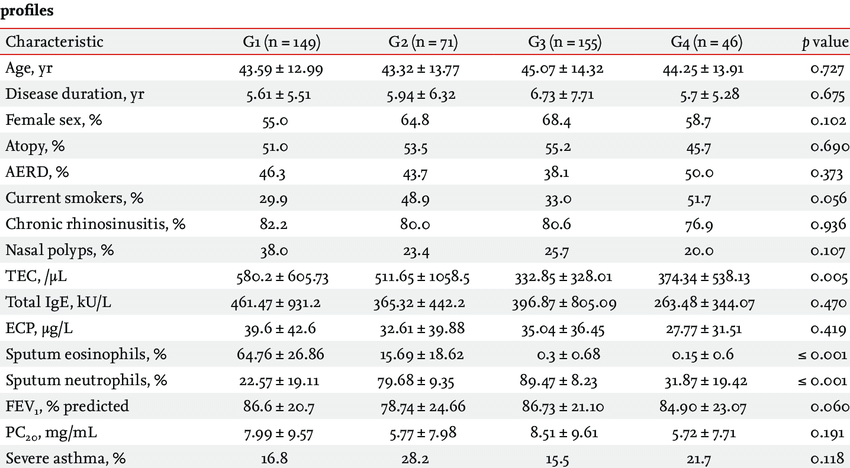
A team of researchers from the NIHR Leicester Biomedical Research Centre a partnership between Leicesters Hospitals, the University of Leicester and Loughborough University has identified biological variations in lung tissue samples that for the first time can help identify people with mild asthma from those with moderate or severe asthma.
The team led by Professors Salman Siddiqui and Peter Bradding used state-of-the-art statistical methods involving visualisation approaches, to perform the largest comprehensive analysis of common pathological features in the airways of people with asthma of different severities. They also investigated the clinical features of these subtypes and whether there is any association with changes in genes and decline in lung function.
Professor Siddiqui and his team identified multiple biological micro-clusters which means that there are different combinations of active genes in each of the reported subtypes of asthma.
Professor Siddiqui, Professor of Airway Diseases at the University of Leicester and Consultant Respiratory Physician at Leicesters Hospitals, added: Further research is now underway to understand how to use these statistical approaches to combine complex information in asthma patients and make personalised treatment decisions.
This research was supported by Ayasdi machine intelligence, a software platform that supports topological data analysis of high dimensional data.
Don’t Miss: How Do You Know When You Have An Asthma Attack
Monitoring Asthma At Home
Some people use a handheld peak flow meter to evaluate their breathing and determine when they need intervention, before their symptoms become severe. People who experience frequent, severe asthma attacks should know how to reach help quickly.
Peak expiratory flow can be measured using a small handheld device called a peak flow meter. This test can be used at home to monitor the severity of asthma. Usually, peak flow rates are lowest between 4 AM and 6 AM and highest at 4 PM. However, more than a 30% difference in rates at these times is considered evidence of moderate to severe asthma. People with moderate to severe asthma, particularly those who need daily treatment to control symptoms, often use a peak flow meter to take measurements and compare them to their personal best to help identify signs of worsening asthma or the onset of an asthma attack.
All people with asthma should have a written treatment action plan that was devised in collaboration with their doctor. Such a plan allows them to take control of their own treatment and has been shown to decrease the number of times people need to seek care for asthma in the emergency department.
Different Lung Compartments Involved In Asthma
Traditionally, asthma has been regarded as a disease characterised by chronic inflammation and remodelling, primarily of the large airways, which leads to airflow obstruction and asthma-specific symptoms. Over 100years ago, autopsy specimens revealed macroscopic pathology within the large airways . However, subsequent physiological, imaging and pathological studies demonstrated that the small airways and even the lung parenchyma could be important contributors to the functional impairment seen in certain severe asthma patients, as some reports suggest asthma severity increases in proportion to the involvement of this compartment . Small airways include all peripheral membranous bronchioles <2mm in diameter, whereas large airways contain smooth muscle and cartilage and have a luminal diameter >2mm . Numerous reviews on the importance of small airways in asthma and other airway diseases have been published in recent years, including the following .
These distal lung studies began to link distal airway inflammation with specific symptoms and disease severities. While these studies suggest that small airways and even alveolar tissue may be crucial compartments of the lung which determine disease severity, clinical symptoms and even phenotypes of asthma, their utility in guiding clinical management of patients is unclear. In addition, it remains unknown whether distal airway involvement is present in all asthma patients or whether a distal airway phenotype exists.
Read Also: How To Know If You Have Copd Or Asthma
Beware: There Are Other Diseases That Can Mimic Asthma:
The differential diagnosis of asthma is somewhat dependent on the age of the patient. Infants and small children have unique anatomical considerations that make the differential diagnosis different than that in adults. In adults, several common diseases must be considered, as it is important to recognize that these conditions may occur concurrently in patients with true asthma, significantly complicating its diagnosis and management. These diseases include:
-
Chronic obstructive pulmonary disease
-
Congestive heart failure
-
Medication side effects
-
Rhinitis/sinusitis
-
Vocal cord dysfunction
Vocal cord dysfunction warrants some additional consideration, as it is an increasingly recognized mimic and significant co-morbid condition in people with asthma. Symptoms are very similar to those of asthma but people with VCD often report failure of albuterol to help, inability to take a breath in, and inspiratory stridor. Stress is common but not always a co-factor, and VCD can also mimic exercise-induced asthma, particularly in teens. VCD is diagnosed by various methods, but direct visualization with some type of provocation that elicits symptoms appears to offer the highest yield for diagnosis. Treatment options, which have not been subjected to any randomized trials, primarily consist of speech therapy.
Diagnosing Asthma In Older People
Older people are more likely to have other lung diseases that also cause shortness of breath , so doctors have to determine how much of the person’s breathing difficulty is related to asthma and reversible with the appropriate anti-asthma therapy. Often, in these people diagnosis involves a brief trial of drugs that are used to treat asthma to see whether the person’s condition improves.
Also Check: How To Stop Allergy Induced Asthma
Who Is A Candidate For Lung Biopsy
Selection of patients for lung biopsy should address two points: 1) accurate diagnosis of the severe airway disease and/or 2) heterogeneity of severe asthma phenotypes to direct treatments. Therefore, patients with atypical features of severe, systemic corticosteroid-dependent asthma may be considered appropriate candidates for lung biopsies . Atypical features include findings suggestive of parenchymal disease, e.g. reduced DLCO or parenchymal alterations in the HRCT.
Preoperative evaluation including indications and risk factors
Similarly, patients with consistently high FeNO or blood eosinophils , despite high corticosteroid doses, represent a poorly understood group who might qualify for more invasive diagnostics, especially since EGPA is part of the differential. Patients with severe asthma and a background of autoimmune disease, e.g. personal autoimmune disease, positive autoantibodies or family history of autoimmune disease, with less allergic history might also be considered. Pathologically those patients seem to be characterised by a predominant lymphocytic inflammatory pattern and appear to respond to immunosuppressive drugs.
Less Common And Invasive Testing
Diagnostic bronchoscopy, complemented by bronchiolar lavage or biopsy, may be needed to clarify interstitial lung diseases, such as sarcoidosis or malignancy, and confirm atypical or fungal infectious processes. Right heart catheterization is required to confirm the diagnosis of pulmonary arterial hypertension, to assess the severity of the hemodynamic impairment, and to test the vasoreactivity of the pulmonary circulation.31 Gallium scanning occasionally may be used to identify inflammatory, neoplastic, or infectious processes.7
Data Sources: Literature searches were performed in Essential Evidence Plus, PubMed, Dynamed, and Database of Reviews of Effects . Search terms included dyspnea, chronic dyspnea, COPD, pulmonary arterial hypertension, interstitial lung disease, congestive heart failure, thromboembolic disease, pulmonary function testing, spirometry, and right heart catheterization. Guidelines of the American Thoracic Society, the American College of Radiology, and the American Heart Association also were reviewed. Search date: November 1, 2010.
Editor’s Note: Table 3 has been removed from this article due to the identification of multiple errors and inconsistencies with the cited references that were discovered during a subsequent review.
Read the full article.
- Get immediate access, anytime, anywhere.
- Choose a single article, issue, or full-access subscription.
- Earn up to 6 CME credits per issue.
You May Like: What Does A Nebulizer Do For Asthma
