Implications For Research And Practice
This study suggests that overdiagnosis of asthma in patients with COPD is more likely than overdiagnosis of COPD in patients with asthma. COPD is possibly more conservatively diagnosed as it is considered a more severe disease, whereas asthma can be more liberally diagnosed. In addition, a patient with COPD can be diagnosed with asthma in the years before first COPD diagnosis, after which no further recording of asthma is made, suggesting that the asthma diagnosis was likely to be false. In patients with presumed concomitant diagnosis of asthma and COPD, reversibility testing can be used to verify the asthma diagnosis.
The findings from the present study have implications for further research into concomitant asthma and COPD. Identifying potential concomitant asthma and COPD using electronic health records should be done cautiously. If only a single code for both diseases is required for the identification algorithm, the prevalence of concomitant diagnosis of asthma and COPD is likely to be overestimated.
Difference Between Asthma And Chronic Obstructive Pulmonary Disease
July 21, 2017 by Rachna C
The respiratory disease which is diagnosed during childhood, resulting in shortness of breathing, dryness of a cough, chest tightening is called asthma. On the other hand, COPD also known as Chronic Obstructive Pulmonary Disease;is also one of the respiratory disease, which occurs after the age of 4o, and the condition gets progressively worse with age.
The cells of our body need oxygen to work and grow, and this oxygen is taken by the lungs through the simple process of breathing. Usually, in a day, we breathe 25,000 times a day. But people suffering from any lungs infection experience the problem in breathing.
Lung diseases are one of the most common medical conditions existing in the world. There are many kinds of lungs infections like bronchitis, cystic fibrosis, emphysema, COPD, asthma, pneumonia, tuberculosis, etc. pollutions, infections, allergens, smoking or genetics can be the major cause of all these problems.
In this article, we will mark the vital difference between the two common respiratory disease asthma and the COPD. We will also discuss their causes, symptoms, and treatment.
Airflow Restriction: Reversible Or Permanent
- Asthma treatment generally returns lung function to normal or near-normal and you should not have many asthma symptoms between asthma exacerbations. Airflow restriction in asthma is generally considered reversible, though some people who have severe asthma develop irreversible damage.
- Even with COPD treatment, airflow restriction and lung function will likely not return to normal or may only partially improveeven with smoking cessation and bronchodilator usage.
Also Check: Acid Reflux Causing Asthma
Understanding The Difference Between Copd And Asthma
When you develop a lung disease or infection such as asthma or chronic obstructive pulmonary disease , you are often required to make significant lifestyle modifications to make breathing easier. After diagnosis, its normal to have questions. For many people, the big question is: How can I breathe easier?
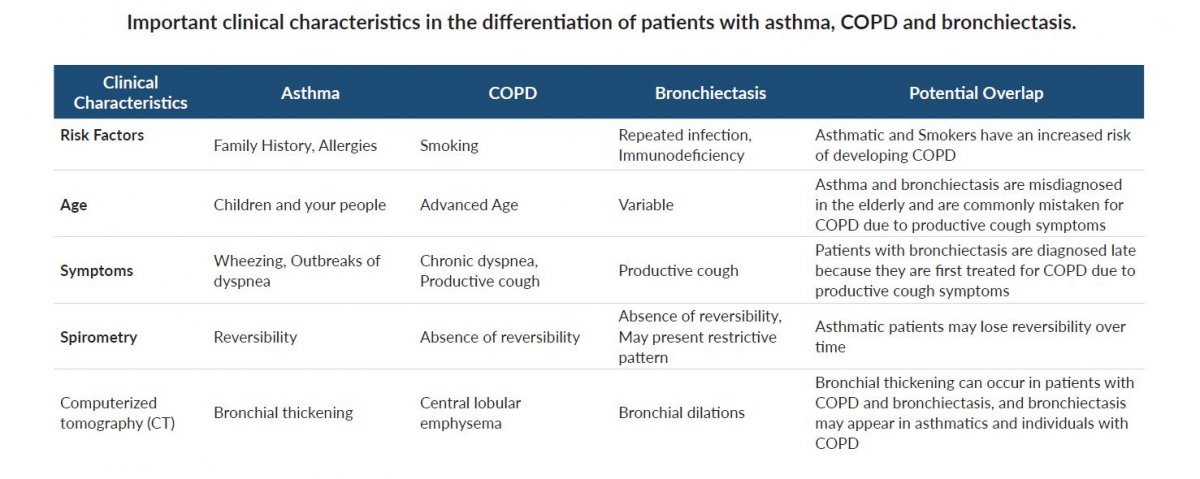
The first step is getting the diagnosis straight. A sufferers prognosis and treatment options are very dependent on the actual condition. When it comes to chronic lung conditions, it can be difficult to tell symptoms apart, and on occasion, it can result in an incorrect diagnosis. For example, asthma and COPD differences are subtle, and theres even a third possibility: asthma-COPD overlap syndrome. Knowing the difference can be difficult but essential to a good treatment plan.
Here are a few major differences between COPD and asthma:
What Is The Difference Between Asthma And Copd
Asthma is a chronic lung disease that makes breathing difficult. With asthma, air passages are inflamed,;which results in the narrowing of the airways that is responsible for carrying the oxygen to the lungs. As a result, symptoms of asthma arise that include wheezing, coughing, shortness of breath, and tightness of chest.
COPD or chronic obstructive pulmonary disease,;on the other hand, is an obstructive pulmonary disease which also makes breathing increasingly more difficult,;however,;this condition develops over many years. Most people with COPD would only notice the symptoms when they reach their late 40s and 50s.;Though these conditions may cause a lot of similar symptoms, asthma and COPD are far from the same condition.
1.;Cause and Triggers
Asthma ;
Theres really no clear explanation why;people have asthma and some dont, but its high likely due to a combination of genetic and environmental factors.
Signs and symptoms of asthma can be triggered by exposure to several substances and irritants that trigger allergies. Though triggers vary from person to person, below;are amongst the reported asthma irritants and triggers:
Your chances of developing asthma would also greatly increase if you are:
- Being a smoker and overweight
- Have a family member or blood relative that has asthma
- Being exposed to secondhand smoke, exhaust fumes and other type of pollutions
- Being exposed to occupational triggers such as chemicals used in hairdressing, farming and manufacturing.
COPD ;
Asthma
Recommended Reading: Relieving Asthma Without Inhaler
Differential Diagnosis Of Asthma And Copd In Older Adults: Role Of Spirometry
Senior Care Consultant Pharmacist andPresident of MZ Associates, Inc.,Norwich, New YorkRecipient of the Excellence in GeriatricPharmacy Practice Award from the Commission for Certification in Geriatric Pharmacy.;
US Pharm
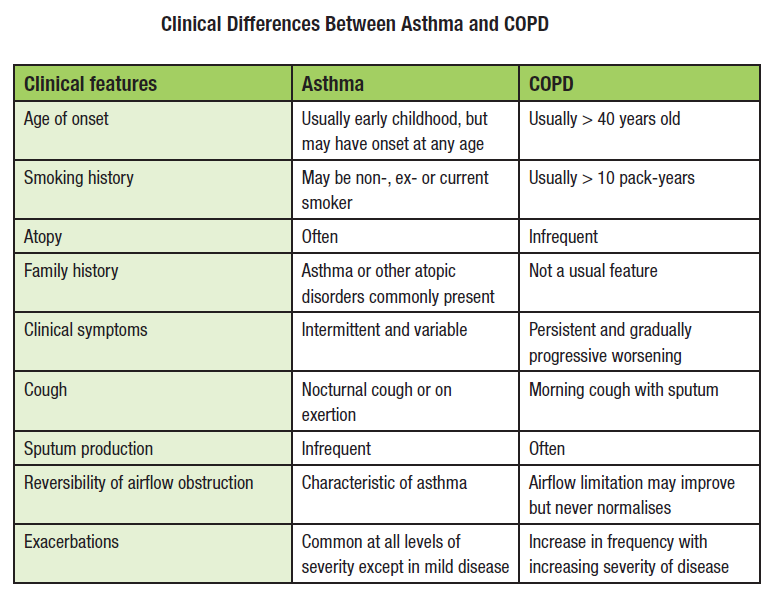
Asthma and chronic obstructive pulmonary disease are common disorders associated with significant morbidity and mortality in the elderly. COPD, diagnosed in the sixth decade in most patients, continues to be underrecognized despite its status as an important chronic disease and a leading cause of disability in seniors.1 Whether asthma or COPD, a number of studies have shown that symptoms of obstructive lung disease are underreported by the elderly and under- or misdiagnosed by physicians.2
Today, the prevalence of COPD is greater in women, and since the year 2000, the mortality rate of this disease has been higher in women than in men.2 Experts estimate that worldwide, by the year 2020, COPD will rank as the third-leading cause of death and as the fifth-leading cause of disabilityeven though it is largely a preventable disease.1,2 Almost all patients with COPD are current or former smokers.3 The smoking epidemic of the twentieth century has greatly contributed to COPD and cardiovascular disease, both of which may cause symptoms that mimic asthma.1,4 Cardiovascular disease and cancer are considered significant comorbidities associated with COPD.
Do Pft Features Distinguish Asthma From Copd
In general, most clinicians have no difficulty distinguishing asthma from COPD. Most asthmatics are nonsmokers, but the vast majority of COPD is caused by tobacco use. Atopy is very frequent in asthma, but less common in COPD. The main PFT phenotypic factors distinguishing the 2 are listed in . However a substantial group of patients have overlapping features. How well do PFT parameters distinguish these 2 conditions? Specifically, does lack of bronchodilator response rule out asthma in a smoking adult?
Typical Contrasting Pulmonary Function Testing Features of Asthma and COPD Phenotype
Fabbri and co-workers looked at a group of patients with fixed air flow obstruction, which they defined as post-bronchodilator FEV1< 0.70. Using a composite clinical picture to assign 19 as asthma and 27 as COPD, they sought to identify which clinical features, including PFTs, were best at distinguishing the 2 conditions. COPD patients were more likely than asthma patients to have smoked tobacco , to have higher RV percentage predicted , to have lower DLCO percentage predicted , to have lower PaO2 , to have smaller acute response of FEV1 to inhaled bronchodilator , smaller change in FEV1 after inhaled corticosteroid , and higher CT emphysema score .
Pulmonary Function Test Parameters and Inflammatory Measures to Distinguish Asthma from COPD*
Recommended Reading: What Part Of The Body Does Asthma Affect
Treatment Options For Copd And Asthma
Asthma diagnostic tests;include spirometry, which estimates the narrowing of your bronchial tubes, and peak flow, which measures how hard you breathe out. Additional tests include methacholine challenge, nitric oxide test, imaging tests, allergy testing, sputum eosinophils, and provocative testing for exercise and cold-induced asthma.
Treatment for asthma;is lifelong and often involves inhaled medications including inhaled corticosteroids. Other medications used to treat asthma include leukotriene modifiers, long-acting beta agonists, combination inhalers, and quick-relief medications for rapid, short-term relief of asthma symptoms.
Working closely with your doctor can help you develop an asthma control plan, which includes your triggers and medication dosages. Regular check-ups with your doctor can also see the progress of your asthma and make any required changes to your asthma control plan.
Common treatments for COPD include smoking cessation, medications like inhaled steroids, bronchodilators, combination inhalers, oral steroids, antibiotics, lung therapies, and surgery including lung column reduction surgery where damaged parts of the lungs are removed to create more space for healthy lung tissue to expand, and a lung transplant.
Is Air Flow Obstruction A Risk Factor For Lung Cancer
Cigarette smoking is the main risk factor for lung cancer, accounting for roughly 85% of cases. Multiple studies have suggested that air flow obstruction is a risk factor for lung cancer independent of smoking, but the role of radiographic evidence for emphysema is less clear. A recent study from the Mayo Clinic enrolled 1,520 patients who were followed for 4 years for the development of lung cancer . When analyzed as a continuous variable, reduced FEV1 and FEV1/FVC were associated with a subsequent diagnosis of lung cancer, with an odds ratio of 1.15 and 1.29 , respectively. When analyzed as a categorical variable, more severe air flow obstruction was associated with greater likelihood of lung cancer . There was no statistical association between percent volume of emphysema on chest CT scan and prevalent or incident lung cancer . Total lung volume measured on chest CT was significantly higher in patients with lung cancer than control subjects .
Presence of Air Flow Obstruction and Its Severity Predict Development of Lung Cancer Independent of Age, Smoking History, and Sex on Conditional Logistic Regression*
Read Also: What Do You Do When You Have An Asthma Attack
Primary Outcome And Measurements
The primary outcome for this study was the proportion of patients with either asthma or COPD who had the other disease in the validated asthma and COPD populations. The presence of a diagnostic asthma Read code and positive reversibility tests supported an asthma diagnosis in the COPD population. The presence of a diagnostic COPD Read code, smoking history, and fixed airflow obstruction supported a current COPD diagnosis in the population with validated asthma. Spirometry measurements with at least one airflow measurement with forced expiratory volume in 1 second to forced vital capacity ratio â¤70% were considered as evidence for an obstructive airflow limitation. The quality of the spirometry procedure undertaken in UK primary care to diagnose COPD is high, as determined in a previous validation study.
Conversely, if the last COPD code was given >2 years before the validation of an asthma diagnosis , the COPD might be misdiagnosed as the code was not repeated afterwards.
Know About Asthmatic Bronchitis
Asthma and bronchitis are defined as two inflammatory airway diseases. While they have distinct differences, as outlined above, asthma and acute bronchitis can occur together. This is known as asthmatic bronchitis.
A number of factors can contribute to asthmatic bronchitis. What triggers the symptoms in one person may be different than what causes a flare-up in another; however, the following are the most common factors:
- Pollution
- Weather
- Viral or bacterial infections
- Emotions
As you may have guessed, the symptoms of asthmatic bronchitis are a combination of asthma and bronchitis. They include shortness of breath, coughing, wheezing, tightness in chest and the production of phlegm.
Due to a virus or bacteria bronchitis can be contagious, however chronic asthmatic bronchitis is not contagious.
Respiratory diseases affect people of all ages- children, teens, adults and seniors. Most of these diseases, such as asthma, bronchitis and COPD, are chronic and all have a significant impact on the individual with the disease, as well as on family, the community and the health care system. Its in everyones interest to gain a better understanding of respiratory ailments, not only so current patients can breathe easier, but so that we can prevent future generations from suffering.
Related Reading:
Read Also: How To Prevent Asthma Attacks
Inflammatory Cells In Copd
Neutrophils are present in sputum of smokers but increased in COPD and related to disease severity. They may be important in mucus hypersecretion and through release of proteases. Macrophages: big numbers are in airway lumen, lung parenchyma, and bronchoalveolar lavage fluid. They produce increased inflammatory mediators and proteases and may show defective phagocytosis. T lymphocytes: both CD4+ and CD8+ cells are increased in the airway wall and lung parenchyma, with big CD8+/CD4+ ratio. Increased is the number of CD8+ T cells and Th1 cells which secrete interferon- and express the chemokine receptor CXCR3. CD8+ cells may be cytotoxic to alveolar cells. B lymphocytes: are increased in peripheral airways and within lymphoid follicles, possibly as a response to colonization and infection. Eosinophils: increased eosinophil proteins in sputum and eosinophils in airway wall during exacerbations. Epithelial cells: May be activated by cigarette smoke to produce inflammatory mediators .
Staging And Treatment Of Asthma
The goals of long-term management of asthma should include the following: 1) achievement and maintenance of control of symptoms; 2) prevention of asthma exacerbations; 3) maintenance of pulmonary function as close to normal levels as possible; 4) maintenance of normal activity levels, including exercise; 5) avoidance of adverse effects from asthma medications; 6) prevention of the development of irreversible airflow limitation; and 7) prevention of asthma mortality.
The recommended GINA treatment algorithm, together with the clinical features and staging of severity of asthma, are available on the GINA website . It is important to note that the forced expiratory volume in one second levels are before treatment, i.e. in the unmedicated state.
Until the advent of anti-inflammatory drugs, asthma was treated on an as-needed basis and treated as an acute disease rather than a chronic disease. With the recognition that asthma is a chronic inflammatory disease, there has been a gradual move towards treating it more aggressively and earlier in the hope that this may change the natural history of asthma and prevent some of the remodelling that sometimes occurs.
You May Like: Does Asthma Medication Cause Weight Gain
A Snapshot Of Obstructive Lung Disease
Asthma and chronic obstructive pulmonary disease are characterized by a reduced rate of pulmonary airflow resulting from increased inflammation. Airway obstruction is typically fully or nearly fully reversible in patients with asthma, whereas COPD is characterized by airway obstruction that is not fully reversible. Patients with either disease may develop acute exacerbations characterized by increased inflammation of the airway and worsening airway obstruction.
Asthma most often presents at a younger age as recurrent episodes of increased airway obstruction that may have varying frequency and intensity, which then become recognized as a chronic pattern of reversible airway obstruction. In a subset of patients with long-term disease, reversibility of airway obstruction is diminished , and a disease pattern similar to COPD may ensue. When the onset of asthma occurs in the sixth or seventh decade of life, recognition is more difficult because symptoms may be similar to those of cardiac disease and COPD, and patients often accept problems as secondary to aging rather than disease.
Is Dlco Helpful In Predicting Exercise Oxygen Desaturation
Studies from the 1980s indicated that DLCO was more useful for excluding exercise oxygen desaturation during exercise in COPD patients than in ruling it in., Owens and colleagues found that a DLCO of 55% predicted had 82% specificity and 100% sensitivity for excluding exercise-induced O2 desaturation in COPD. Ries and co-workers found that an FEV1/FVC 0.50 and DLCO 20 mL/min/mm Hg were 100% predictive in excluding a fall in exercise PO2 in 40 patients with COPD.
More recently, using a large database in patients with mixed pulmonary diseases, the ability of DLCO to predict exercise O2 desaturation 4% on a 3-min step-test was examined. Obstructive lung disease was present in 74% of subjects, and restrictive diseases in 5.6%. A low DLCO was present in 56% of patients with restriction, and 33% of patients with an obstructive pattern. If DLCO was low, the odds ratio was 34 for O2 desaturation in restrictive patients and 18 in the obstructive group. Overall, for all subjects, a cut point of 62% predicted was most useful. When DLCO was < 62% predicted, using the Miller et al reference equation, the sensitivity and specificity for O2 desaturation were both approximately 75%.
These studies suggest that a reduced DLCO is not sufficiently accurate to predict exercise O2 desaturation without directly measuring it. However, among patients with COPD, the presence of a low DLCO warrants measurement of exercise O2, often in conjunction with a 6-min walk distance test.
You May Like: How To Deal With Asthma Attack Without Inhaler
Knowing When To See A Professional
Clearly, there are numerous ways to effectively manage asthma and COPD, which means the prognosis for both diseases can be hopeful as long as each condition is caught early. While neither asthma nor COPD are considered curable, asthma is typically easier to control on a daily basis by avoiding triggers and taking the proper medication. As a progressive disease, COPD may get worse over time, but sticking with a physician-prescribed treatment plan can slow the disease’s progression and lessen symptoms.
The first step in successfully managing both conditions is to see a medical professional. Whether you suffer from difficulty breathing, coughing, wheezing or chest tightness or simply have a family history of the disease, you should consider seeking professional help. After consulting with a medical specialist, you will have a better idea of your condition and available treatment options.
It is especially important to receive medical attention specifically intended for your individual condition. Look for a rehabilitation center like Post Acute Medical that offers;cardiopulmonary health services;explicitly created to benefit asthma and COPD patients. At Post Acute Medical, there are precise treatment plans and therapies for a wide range of cardiopulmonary conditions, including COPD and asthma.
- Methods to maximize oxygen intake.
- Disease pathology.
- Infection control.
- Respiratory care.
Asthma Vs Copd: What’s The Difference
It is no surprise that asthma and chronic obstructive pulmonary disease are often mistaken for one another they are both conditions that affect the lungs and make breathing more difficult. Despite their many similarities, asthma and COPD are not the same. In honor of November being;National COPD Awareness Month, it is time to finally clear up the question of whether asthma and COPD are the same thing.
Below, we will look at the definitions of the two diseases, along with the symptoms, causes and treatments for each. We will also discuss when to see a medical professional for lung damage to help raise COPD awareness this month.
Read Also: Does Weight Gain Make Asthma Worse
