Examination Of The Respiratory System
Wheezing occurs from air moving through narrowed, obstructed airways. Thus exhalation results in turbulent airflow and produces wheezes. Although asthma is the most common cause of wheezing, anything that causes airway obstruction and narrowing that results in turbulent airflow may generate wheezes. Therefore, not all wheezing is asthma.
Auscultation often reveals bilateral expiratory and possibly inspiratory wheezes and crackles. Air entry may or may not be diminished or absent, depending on severity. Remember, the silent chest may herald impending respiratory failure in a patient too obstructed or fatigued to generate wheezing.
If tension pneumothorax develops, signs of tracheal deviation to the opposite side, decreased or absent air entry on the affected side, shift of the location of heart sounds, and hypotension may be evident. Air leaks may also result in pneumomediastinum and subcutaneous emphysema.
In moderate to severe status asthmaticus, abdominal muscle use can cause symptoms of abdominal pain.
Pulsus paradoxus results from a decrease in cardiac stroke volume with inspiration due to greatly increased left-ventricular afterload. This increase is generated by the dramatic increase in negative intrapleural and transmural pressure in a patient struggling to breathe against significant airways obstruction. Pulsus paradoxus of greater than 20 mm Hg correlates well with the presence of severe airways obstruction .
References
Hypoxemia Hypercapnia And Lactic Acidosis
Intrapulmonary shunt appears to be practically absent in the majority of patients because of the collateral ventilation, the effectiveness of the hypoxic pulmonary vasoconstriction, and the fact that the airway obstruction can never be functionally complete . Hypoxemia is therefore common in every asthmatic crisis of some severity mild hypoxia is easily corrected with the administration of relatively low concentrations of supplemental oxygen . More severe hypoxemia and the need for higher concentrations of supplemental oxygen may relate to some contribution of shunt physiology.
Analysis of arterial blood gases is important in the management of patients with acute, severe asthma, but it is not predictive of outcome. In the early stages of acute, severe asthma, analysis of arterial blood gases usually reveals mild hypoxemia, hypocapnia and respiratory alkalosis. If the deterioration in the patient’s clinical status lasts for a few days there may be some compensatory renal bicarbonate secretion, which manifests as a non-anion-gap metabolic acidosis. As the severity of airflow obstruction increases, arterial carbon dioxide first normalizes and subsequently increases because of patient’s exhaustion, inadequate alveolar ventilation and/or an increase in physiologic death space.
Management Of Respiratory Failure In Severe Asthma
Intubation and mechanical ventilation can be life-saving for patients with severe asthma exacerbations complicated by respiratory failure. The severe airways obstruction and associated dynamic hyperinflation seen in such patients makes these procedures fraught with risks including hypotension, aspiration, barotrauma, hospital-acquired infection, and myopathy.
Patients presenting with respiratory arrest or severe hypopnea should be intubated immediately. Similarly, those in whom the level of consciousness is inadequate to enable inhaled therapies or to ensure airway protection should be intubated. Other indications for immediate intubation include a paO2 of < 60 mm Hg despite high-flow oxygen delivered by a non-rebreathing face mask and signs of exhaustion such as paradoxical thoraco-abdominal motion and a silent chest. If the patients status is borderline, however, it may be reasonable to begin a trial of aggressive interventions while at the same time preparing for the possibility of intubation should the patient show signs of worsening respiratory acidosis or any of the above signs of respiratory failure.
Rapid-sequence intubation is the standard approach for patients who are obtunded or who are in respiratory arrest. The largest diameter tube possible should be chosen to minimize resistance to airflow and to facilitate suctioning and bronchoscopy.
Recommended Reading: How Can You Treat Asthma
Treatment Of Mild And Moderate Asthma Exacerbations
Most patients with mild exacerbations of asthma are managed at home or in the outpatient clinic. If a patient presents to the ED with the features of a mild exacerbation, the first-line medication is albuterol typically administered by MDI with a holding chamber . Nebulized albuterol is an alternative for patients who have difficulty using an MDI. A mild attack is confirmed when the patient experiences a prompt and complete response to initial treatment with SABA with resolution of wheezing, cough, and/or shortness of breath. These patients can often be discharged after education and scheduled follow-up but with no additional medical therapy. Patients and family members should be given specific instruction in the proper use of inhalers and spacer.
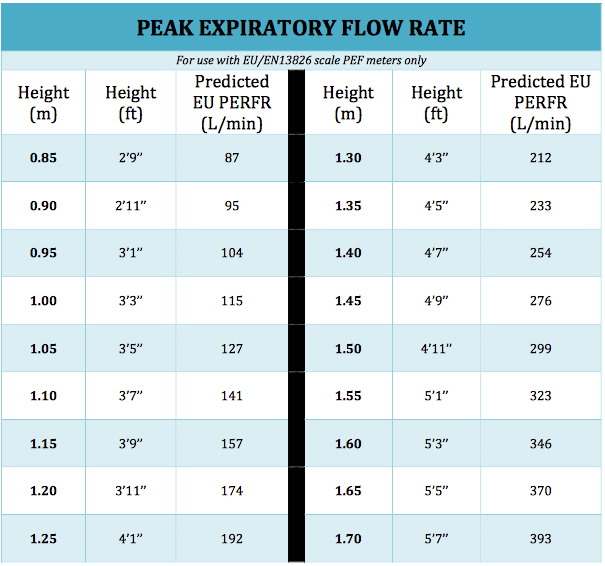
Patients with mild exacerbations who do not have a complete and immediate response to initial therapy with albuterol, and those presenting with features of a moderate exacerbation, should be treated similarly according to the 2007 NAEPP EPR3 guidelines. All patients should have initial and serial measurement of PEFR and all should immediately receive oxygen, a short-acting beta agonist, and systemic CS usually by the oral route.
Supplemental oxygen delivered by nasal cannula or mask should be provided as needed to ensure a peripheral oxygen saturation of at least 90% in most patients. Oxygen saturation should be maintained above 95% in pregnant patients or those with active cardiovascular disease.
Intubation: Risks And Indications
Intubation can exacerbate bronchospasms, making breathing even more difficult and triggering laryngospasms. Historically, intubation has been linked with a 13-16 percent risk of mortality. This may be due to the dangers of intubation itself, but may also be because asthmatics who require intubation are already at a high risk of dying. First responders should try less invasive measures first, particularly if the patient is breathing on their own and not crashing.
Some indications for intubation include:
- Respiratory or cardiac arrest
- Leukotriene inhibitors
Following a severe asthma attack, a patient may need to continue using inhaled anticholinergics for 24-36 hours.
Read Also: How To Solve Asthma Without Inhaler
Adverse Asthma Responses To Nonasthma Medications
The practitioner must be aware that certain medications are contraindicated or relatively contraindicated in patients with acute asthma exacerbations. Beta-blockers are in this category. Although cardioselective beta-blockers have been shown to be safe in short-term use in patients with mildmoderate reversible airways obstruction , their use is not well studied in acute exacerbation. As such, their use in patients with acute exacerbation should be avoided unless a strong indication exists and no alternative is available. Noncardioselective beta blockers such as propranolol, labetalol, and carvedilol should be avoided in acute asthma exacerbation.
Patients with aspirin allergy or with the syndrome of asthma, nasal polyposis, and aspirin sensitivity should not be given aspirin. There is an approximately 20% cross-reactivity with nonsteroidal anti-inflammatory drugs . For such patients presenting with acute coronary syndrome or ischemic cerebrovascular accident, an ADP receptor antagonist such as clopidogrel should be considered as an alternative.
Advanced Multimodal Wireless Vital Signs Monitoring For Patients With Asthma And Anaphylaxis
| The safety and scientific validity of this study is the responsibility of the study sponsor and investigators. Listing a study does not mean it has been evaluated by the U.S. Federal Government. Read our disclaimer for details. |
| Recruitment Status : Enrolling by invitationFirst Posted : April 24, 2020Last Update Posted : July 8, 2022 |
The primary objective of this study is to assess the function and reliability of a non-invasive, skin-like electronic sensor.
We hypothesize that this skin sensor will address an unmet need to wirelessly, noninvasively, and rapidly assess critical vital signs and other measures essential to healthcare monitoring for patients with asthma and anaphylaxis.
| Device: Advanced multimodal wireless vital signs monitor |
The wearable sensors offer a new, non-invasive and easy to use way to monitor vital signs of patients with asthma and anaphylaxis. Our previous experience testing our wearable vital sign sensors in multiple pediatric and neonatal studies since 2016, have shown a strong correlation to existing standard of care monitor data outputs. Additionally, the sensors have received positive feedback from patients and physicians, on their comfort, ease of use, and application.
| Non-Probability Sample |
Inclusion Criteria:
Exclusion Criteria
Also Check: Will Asthma Get You Discharged From The Military
Learn What You Can Do To Help Control Asthma
Help spread the word about Asthma Awareness Month. This Digital Outreach Toolkit offers ideas and activities for you to use on your Web site, blog, or social media pages.
If you or your child has asthma you should:
- Receive ongoing appropriate medical care.
- Be empowered through education to manage asthma and asthma attacks.
- Avoid asthma triggers at school, work, home, outdoors, and elsewhere. Triggers for asthma can include mold, tobacco smoke, outdoor air pollution, and infections linked to influenza, colds, and other viruses.
- Use inhaled corticosteroids and other medicines correctly.
Watch a new CDC video on preventing asthma attacks while traveling with expert commentary by David B. Callahan, MD.
We can all work with our local school systems and school nurses to:
- Encourage students with asthma to use inhaled corticosteroids and other medicines correctly and to avoid asthma triggers.
- Ensure that students inhalers are readily available for them to use at school as needed.
- Take steps to fix indoor air quality problems like mold and outdoor air quality problems such as idling school buses.
If you are an employer or an insurer you can:
How Do Vital Signs Change During A Severe Asthma Attack
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
HealthTap doctors are based in the U.S., board certified, and available by text or video.
You May Like: How To Get Over Asthma Attack
There Are Two Easy Ways To Check Your Asthma Control:
- Do you have asthma symptoms or use your quick-relief inhaler more than two times per week?
- Do you awaken at night with symptoms more than two times per month?
- Do you refill your quick-relief inhaler more than two times per year?
If you answer “yes” to one or more questions, your asthma may not be well controlled. Plan a visit with your healthcare provider and share your results.
Answer five questions about your asthma to determine if your asthma is well controlled. There is a test for children and adults. This assessment provides a score. Share the results with your healthcare provider.
Prognosis Of Patients In Status Asthmaticus
Status asthmaticus carries a significant mortality, ranging between 1 and 10% . Among patients in status asthmaticus admitted to an intensive care unit, between 10 and 30% required mechanical ventilation . In recent years the mortality rate of patients in status asthmaticus requiring mechanical ventilation has decreased significantly . This decrease may reflect earlier diagnosis, aggressive medical treatment, and improvements in mechanical ventilation . Death from asthma in mechanically ventilated patients appears to be further decreased after the application of the ‘permissive hypercapnia technique’.
Recommended Reading: Can Cold Air Cause Asthma
Treatments Not Recommended For Routine Use In Exacerbations
Antibiotics should not be given routinely to patients with asthma exacerbation unless there is a high clinical suspicion for concurrent acute bacterial infection such as pneumonia or sinusitis. Some studies suggest that chronic infection with M. pneumoniae or C. pneumoniae may play a role in acute exacerbations in some patients and research in nonasthmatic airways disease suggests a possible anti-inflammatory effect of macrolide antibiotics. Additional research is needed, however, to define the role of macrolides in asthma exacerbations before their routine use can be recommended.
Aggressive hydration should not be given as a matter of routine unless there is clinical history of poor oral intake, signs and symptoms of intravascular volume depletion, or hemodynamic instability. Careful clinical assessment of volume status should precede aggressive hydration.
Mucolytics should not be given as they have no demonstrable clinical efficacy in acute asthma and are known to induce bronchial irritation and bronchospasm. As mentioned above, methylxanthines are no longer recommended for routine use in acute asthma exacerbations but may be considered for use in severe, treatment refractory cases .
Ems Providers Test Their Knowledge Of Asthma Patients
2012 JEMS GamesIn March 2012, an acute asthma patient will be among the victims managed at the JEMS Games clinical competition at the EMS TODAY conference.This comprehensive clinical article will therefore assist participating teams and attendees in preparing for the JEMS Games, understanding this complex and frequently encountered medical event and obtaining CE credit on JEMSCE.com.In addition, JEMS Games founding sponsor, Laerdal Medical Corp., will provide a special Simulation Tool Kit to each person attending the JEMS Games finals on March 2, 2012. The tool kit will include access to the acute asthma simulation featured at the JEMS Games to allow services to replicate the simulation on their agency and training center simulator.
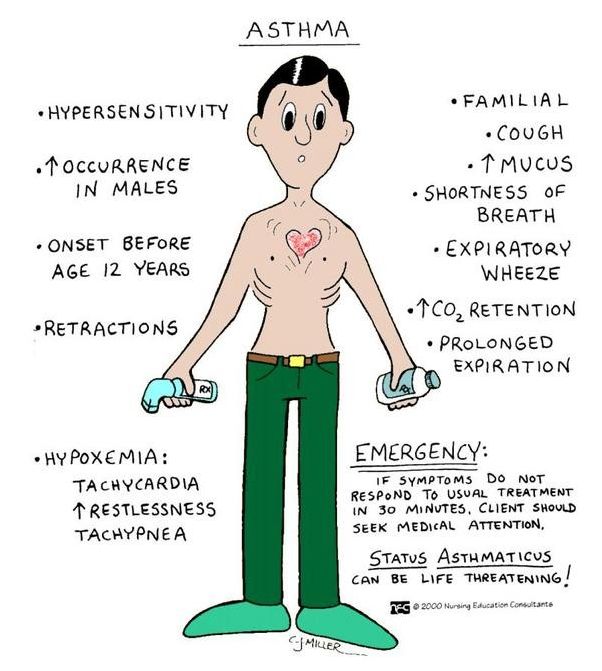
Learning Objectives> > Generalize the pathophysiology of asthma.> > Highlight the major clinical manifestations of asthma.> > Explain the key components of the Initial Visual Assessment Technique.> > Describe physical exam parameters to obtain in a patient with a severe asthma attack.> > Identify the indices that point to a severe asthma attack.> > Describe, sequence and justify the rationale for EMS interventions for an asthma attack.> > List warning signals of a potentially fatal asthma attack.
This article originally appeared in December 2011 JEMS as Fighting for Air: Recognize & treat the severe asthmatic patient.
Don’t Miss: Montana Allergy And Asthma Billings Mt
In Addition To Ics It Is Recommended To:
| Table 3. Inhaled daily dose of corticosteroids for asthma therapy in children is available as a supplementary file. |
Using A Peak Flow Meter
Some healthcare providers like to recommend a peak flow meter to anyone with a new diagnosis of asthma. It can be especially helpful in children. A peak flow meter may help them recognize the signs and symptoms of their asthma getting worse.
A peak flow meter is a portable, inexpensive, hand-held device used to measure how air flows from your lungs in one “fast blast.” In other words, the meter measures your ability to push air out of your lungs.
Patients age 5 years and older are usually able to use a peak flow meter to help manage their asthma. Not all healthcare providers recommend peak flow meters to help children and adults manage their asthma. Many healthcare providers believe a peak flow meter may be of most help for people with moderate and severe asthma. If your asthma is mild or you do not use daily medication, a peak flow meter may not be useful for your asthma management. A peak flow meter is a helpful tool for school health staff to monitor a child’s asthma during the school day.
Peak flow meter measurements can help your healthcare provider make decisions about your treatment and adjust your medicines, and the measurements also can alert you when your asthma symptoms are worsening.
A peak flow meter may help you and your healthcare provider identify causes of your asthma at work, home or play, and it can help parents to determine what might be triggering their child’s asthma.
Recommended Reading: Do Asthma Patients Live Long
Original Contributionvital Signs Including Pulsus Paradoxus In The Assessment Of Acute Bronchial Asthma
One hundred nine episodes of acute bronchial asthma were studied both before and after treatment in the emergency department, comparing the pulse rate, respiratory rate, and pulsus paradoxus to the one second forced expiratory volume . The purpose of this study was to assess the reliability of these clinical parameters in predicting the degree of airway obstruction in acute bronchial asthma. Pulse, respiratory rate, and pulsus paradoxus showed poor correlation to FEV1 both pre- and post-treatment. Further, of all patients presenting with a pre-treatment FEV1 less than or equal to 1.0 liter, 36% had a normal pulse , 17% had a respiratory rate less than or equal to 20/min, and 33% had no pulsus paradoxus. Following therapy, 44% of those patients with persistent severe airway obstruction had a normal pulse, 38% had a respiratory rate less than or equal to 20/min, and 71% had no pulsus paradoxus. Pulse rate, respiratory rate, and degree of pulsus paradoxus are unreliable indices of the degree of airway obstruction in the assessment of acute bronchial asthma, and abnormalities of these clinical parameters tend to disappear with minimal improvement in airway obstruction. Thus pulse rate, respiratory rate, and pulsus paradoxus cannot be substituted for pulmonary function measurements in assessing acute bronchial asthma.
Predicting Fatal Or Near
Near fatality has been viewed as the occurrence of respiratory arrest and/or coma necessitating emergency intubation and mechanical ventilation, and the condition is distinguished from those patients who are electively intubated because of fatigue. Despite research efforts, clinically reliable predictors of patients who are at risk for fatal or near-fatal episodes of asthma have not been conclusively identified. Patient characteristics associated with increased risk include lack of understanding or misinterpretation of the seriousness of symptoms, poor medical adherence, and coincident psychiatric illness and/or substance abuse. At risk patients are also likely to have had multiple ED visits, repeated hospitalizations, admission to the intensive care unit, and a history of respiratory failure. Histopathological findings suggest that the type of acute asthma that leads to death may be a unique entity. Until studies are better able to explain why some patients with asthma die of a potentially reversible disease, ED management needs to focus on rapid evaluation and institution of therapies guided by the best available evidence.
Don’t Miss: What Kind Of Doctor Do You See For Asthma
