When You Have Asthma
People with asthma have very sensitive airways. This means the airways react to certain things called triggers. Triggers can include pollen, dust, or smoke. Triggers cause inflammation. This makes the airways swell and become narrow. This is a long-lasting problem. Your airways may not always be narrow enough so that you notice breathing problems.
Symptoms of chronic inflammation include:
-
Coughing
-
A feeling of tightness in your chest
-
Feeling short of breath
-
Wheezing
-
Low energy or feeling tired
In some people, over time chronic mild inflammation can lead to lasting scarring of airways and loss of lung function.
The Contribution Of High V/q Units To Global Gas Exchange
That can be summarised by simply saying that they don’t contribute much of anything. Though the gas exchange in these high V/Q ratio segments is excellent, their total contribution to the gas exchange of the whole respiratory system is minimal, because blood flow to these segments is also minimal. A rabbit study by Lamm et al demonstrated that overall, only about 15% of the cardiac output goes to the “Zone 1” segments of the lung, with most of the ventilation there being in lung units with a V/Q ratio around 5.
The most important implication of this is that the high V/Q units cannot compensate for the failure of low V/Q units. Low V/Q units are responsible for most of the blood flow returning to the left atrium. Therefore, when they fail to oxygenate the blood , this 85% of the cardiac output ends up looking a lot like mixed venous blood. In this scenario, “good” V/Q units will not be able to contribute enough arterial-looking blood to compensate.
How Do My Airways React To Triggers
If you have asthma you have sensitive airways that are inflamed and ready to react when they come into contact with something they don’t like.
If you come into contact with one of your asthma triggers it causes your airways to react in three ways:
These reactions in the airways make it difficult to breathe and lead to asthma symptoms, such as chest tightness, wheezing, or coughing. It can also lead to an asthma attack.
You May Like: Does Weight Gain Make Asthma Worse
Baseline Pulmonary Function And Arterial Blood Gas Status During Exercise
Because of the potential for narrowed airways to alter the ventilation distribution and minimize the hyperventilation of heavy exercise, it is reasonable to hypothesize that the level of baseline airflow limitation might provide some prediction of arterial blood gas status during exercise in asthmatic subjects. However, for a given level of baseline airflow limitation in our subjects, exercise PaO2 and PaCO2 spanned a wide range of values. For example, for eight subjects, baseline FEV1.0/FVC was 0.650.70 , but PaO2 at end exercise was 7197 Torr, PaCO2 was 3347 Torr, and SaO2 was 9096%. Thus several subjects with compromised baseline lung function and significant EFL during exercise also hyperventilated normally and were able to maintain normal PaO2 during exercise.
How Do The Lungs Work
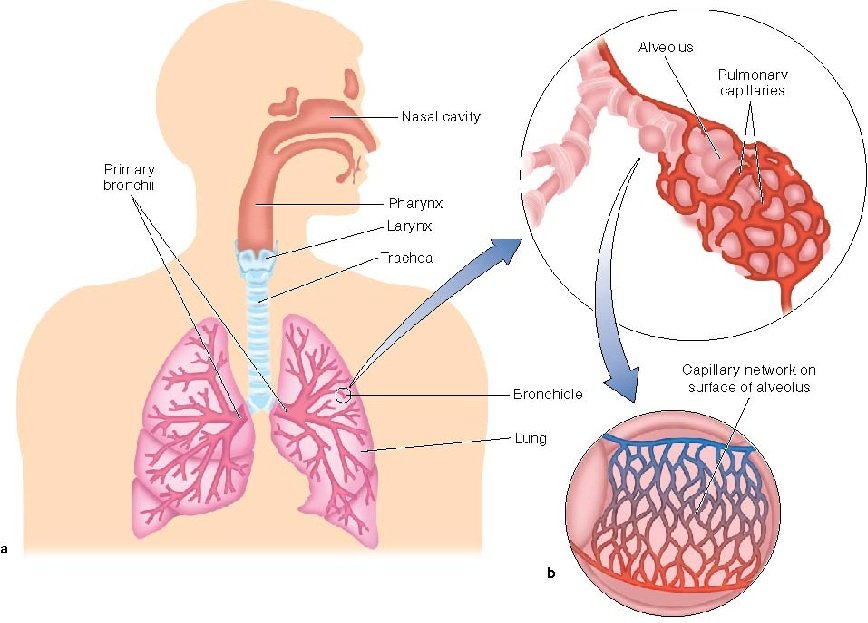
The primary function of the lungs is breathing. Gas exchange is the name of the process by which oxygen enters the bloodstream and carbon dioxide waste leaves the body . The structure of the lung has evolved to perform this task very efficiently. The basic structure of the lungs is a series of hollow tubes, called airways. Airways branch and get smaller, ending in tiny air sacs called alveoli. Alveoli are covered in small blood vessels named capillaries, which function to exchange gases in the blood . The lungs can be compared to a tree that has a large, main trunk with branches becoming smaller the further away they are from the trunk. The alveoli are like the leaves.
- Figure 1 – The mucociliary escalator in a healthy person and in a person with a diseased mucociliary escalator .
- The mucociliary escalator is found in the trachea, bronchi, and bronchioles, which are part of the conducting zone. Gas exchange occurs in the alveoli in the respiratory zone .
Also Check: Asthma In The Air Force
Ventilation/perfusion Mismatch In Acute Exacerbation Of Chronic Obstructive Pulmonary Disease
Mechanisms responsible for the development of low V/Q ratio in patients with AE-COPD include airway narrowing due to bronchial inflammation, bronchospasm, or mucous accumulation. Shunt fraction is not increased during acute exacerbation probably due to the absence of complete airway occlusion or the presence of collateral ventilation.
Barberàet al. evaluated the mechanism of hypoxemia in 13 male patients admitted to hospital with acute exacerbations COPD . Both V/Q mismatch and reduced PvO2 are responsible for hypoxemia development in AE-COPD. PvO2 is an important contributor to hypoxemia and for a given level of V/Q mismatch reduced PvO2 is associated with reduced level of PaO2. PvO2 is reduced due to greater consumption of oxygen by the overactive respiratory muscles. CO is one extrapulmonary factor that can modulate the impact of low PvO2 on resulting hypoxemia by improving the PvO2 value. Therefore, we should be cautious in using drugs that can reduce CO in COPD patients during AE.
How Can I Stop My Asthma Getting Worse Over Time
The best way to stop your asthma getting worse over time is to stick to a good routine of taking your preventer medicines as prescribed.
And if you notice your symptoms are getting worse, see your GP or asthma nurse as soon as possible so they can review your treatment.
You can also cut your risk of frequent asthma attacks, and your asthma getting worse, by stopping smoking.
Having an asthma review at least once a year, gives you a chance to talk through any symptoms or new triggers. You can check youre on the right medicine and that youre using your inhaler in the right way to get the most benefits.
You can also talk to your GP or asthma nurse about whether you need a higher dose or an add-on treatment to help with symptoms.
Also Check: Can Asthma Come Out Of Nowhere
Normal Exchange Of Oxygen And Carbon Dioxide
The exchange of O2 depends on a partial pressure gradient between alveolar gas and pulmonary capillary blood. In the normal lung, capillaries deliver mixed venous blood with a low PO2 to the alveolus . Because the PO2 in the alveoli is much higher than in the pulmonary capillary, O2 diffuses passively from the alveolar space into the blood. Under normal conditions, the PO2 rapidly equilibrates between the alveolar gas and pulmonary capillary blood, although there is always a small difference between the alveolar and arterial O2, referred to as the alveolar-arterial O2 difference O2) due to blood returning to the left atrium from the bronchial and thebesian veins. As will be described further below, the magnitude of the PO2 can be used to identify cause of hypoxemia in a given patient.
A single-lung unit model with notations used for partial pressures , gas fractions , and content for oxygen for different compartments. Note that with a single-unit lung model, arterial and end-capillary values are equal.
Exchange of CO2 follows similar principles. The partial pressure of CO2 is greater in mixed venous blood than in the alveolar gas , so net flow is down a pressure gradient from capillary blood to alveolar gas. Elimination of CO2 is highly efficient due to the steepness of the carbon dioxide dissociation curve in the physiologic range of partial pressures when compared with oxygen .
How Do Your Airways Work When You Have Asthma
When you have asthma, your airways aren’t able to function as well as they should.
- Wheezing
- Chest tightness
Asthma causes inflammation, or swelling, in the lungs. It can also cause squeezing, called bronchoconstriction , and extra sensitive or twitchy airways.
When something bothers your airways, you have trouble breathing. This is called an asthma attack or episode. It gets harder to breathe because the tiny muscles around your airways squeeze tightly and they have swelling inside.
Your airways will make more mucus inside your airways, which makes it even harder to breathe. These changes in your airways can cause coughing and wheezing.
There is no cure for asthma. But you can take steps to manage it. If you have asthma, it’s important to see an asthma specialist, like an allergist or pulmonologist, to come up with the right asthma treatment plan. Medicines and avoiding asthma triggers can help reduce swelling and relax tight muscles in your airways.
ASTHMA Care for Adults
Read Also: What Can Cause Asthma Exacerbation
Icles And Germs In The Airwhy The Lungs Need Defense
There are many types of particles that could enter the lungs and cause damage. Some of these particles are pollutants, such as emissions from gas-powered vehicles, carbon monoxide from fireplaces, toxins from vaping or smoking, and aerosols like hairspray. Particles can get trapped in various areas of the lung. Short hairs, like the kind on top of your head, line the insides of the nostrils and are covered with mucus. These mucus-covered hairs help trap larger particles as they enter the nose. Particles that enter the conducting zone can hurt the airway cells, which may reduce the movement of their cilia and lead to a buildup of mucus that cannot be cleared from the airways . Mucus-clogged airways may not allow air to travel as effectively, like the way leaves in a gutter interfere with water flow. Smaller particles can sometimes get all the way to the alveoli. Damage to the alveoli makes breathing considerably more difficult, because oxygen will not diffuse as well into the blood. This reduced efficiency of gas exchange may cause the rest of the body to be hypoxic, which means low in oxygen. Only the conducting zone, from the trachea to the bronchioles, has the ability to move mucus using cilia, so alveoli cannot rely on this mechanism to get rid of these small particulates . Living in a polluted city or years of smoking/vaping can cause the lung tissue to become inflamed and lead to diseases, such as chronic obstructive pulmonary disease .
Phenotypic Diversity Among Subjects
We used four different tests of airway function to evaluate our subjects for airway pathology consistent with the diagnosis of asthma. Our subjects showed variable degrees of airway hyperresponsiveness, airflow limitation, and airway inflammation . Thus the results from the inclusion criteria studies highlight the heterogeneity of bronchial asthma and the lack of association between different tests of airway function in asthmatic subjects.
Also, subjects 6, 17, and 21 had a PC20> 16 mg/ml. This is important given the notion that airway hyperresponsiveness to direct-acting stimuli is necessary for the diagnosis of asthma. The alternative view is that asthma is more akin to a syndrome with multiple phenotypes and indicators of airway pathology . Asthma is a complex and heterogeneous condition, and in our view it is overly simplistic to ascribe the diagnosis of asthma on the basis of one outcome measure. Furthermore, we sought to study a group of subjects with a diverse range of airway characteristics consistent with the diagnosis of bronchial asthma.
Read Also: What Happens If You Smoke Weed With Asthma
Breathing Mechanics Measurements During Exercise
Before exercise, subjects performed several maximum volitional flow-volume loops while standing on the treadmill and breathing on the same apparatus used during exercise. EFL was estimated as described previously , and end-expiratory lung volume during exercise was determined by subtracting the exercise IC volume from TLC. Ventilatory capacity during exercise was estimated using the preexercise MFVL and the spontaneous exercise tidal flow-volume loops as described previously . Ventilatory capacity was thus calculated on the basis of the maximal expiratory flow rates achievable at the actual operating lung and tidal volumes measured during the exercise. A nasopharyngeal 10-cm latex balloon-tipped catheter connected by polyethylene tubing to a differential pressure transducer was used to measure esophageal pressure. Inspiratory pulmonary resistance was calculated at peak inspiratory flow according to the technique of Mead and Whittenberger .
Ventilation/perfusion Mismatch In Mild Chronic Obstructive Pulmonary Disease
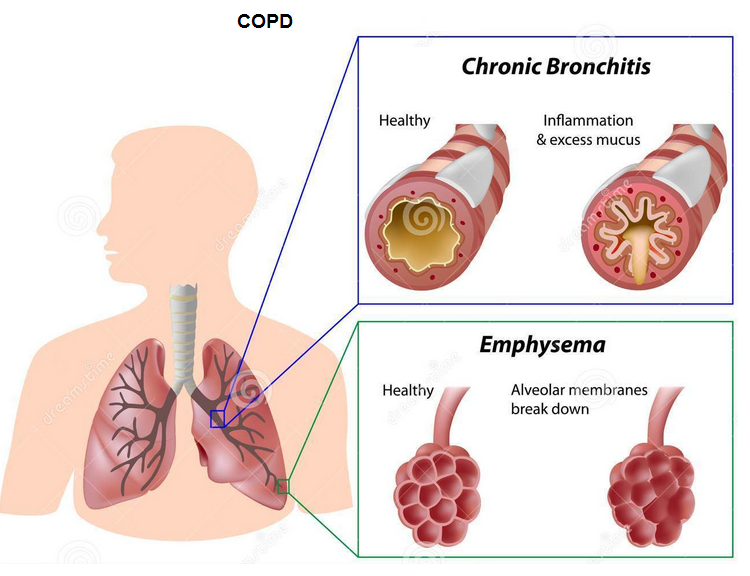
The V/Q mismatch worsens along with the progression of COPD. Rodríguez-Roisin et al. evaluated the V/Q mismatch in 150 patients with COPD of various severities and reported a steady worsening of both V/Q mismatch and arterial blood gas disturbances with the progression of COPD. However, in GOLD Stage IV, the V/Q mismatch was only modestly worse compared to Stage 1 despite the FEV1 value fallen to 20% of predicted. One factor could be that V/Q mismatch is already at its worst in Stage 1, so there is less scope for further deterioration. Patients with GOLD Stage 1 COPD with minimum spirometric abnormalities developed substantial V/Q mismatch. It indicates that pulmonary gas exchange abnormalities occur quite early in the natural history of COPD even before lung function abnormalities develop. The second factor could be simultaneous decrease in both VA and pulmonary blood flow producing a buffering effect. Airway obstruction causes reduced ventilation and alveolar dilatation and HPV causes reduced perfusion.
Don’t Miss: Can Asthmatics Take Ibuprofen
Breathing Mechanics During Exercise
Pulmonary resistance showed large variability among subjects during exercise: Rli was normal in several subjects but increased in others relative to values previously reported in healthy subjects . The slight group mean increases in Rli during exercise are largely explainable by the increased inspiratory flow rates and the nonlinearity of the pressure-flow relationship . On the basis of previous studies that determined transpulmonary pressure at different inspiratory flow rates in otherwise resting humans , we calculated that the increased inspiratory flow rates, per se, caused a 1.0 cmH2O·l1·s increase in mean Rli at minute 1 of the prolonged exercise bout. This accounts for all the observed increase in Rli in 10 of the 14 subjects who demonstrated an increase relative to rest at this time. The increased Rli in the remaining four subjects was beyond that attributable to increased inspiratory flow rate, per se, indicating a decrease in airway caliber during exercise in these subjects.
Vq Mismatch Due To Pulmonary Embolism
The origin of this graph is also a paper by Wagner and West , except for some reason this time they let David R. Dantzker be the first author. The investigators anaesthetised a bunch of dogs and then sent large tantalum-doped emboli into their pulmonary circulation.
As one can see, this scenario produced a similar effect to emphysema i.e. as the result of taking out a large segment of the pulmonary circulation, the patient developed a significant amount of dead space, poorly perfused but normally ventilated lung.
Read Also: What Is Mild Intermittent Asthma
V/q Matching In Emphysema
This graph represents the distribution of flow across the lungs of a patient with severe bullous emphysema. It comes from a study by Wagner et al , where the MIGET technique was used to study “23 male patients with severe and advanced but stable COPD”.
One can immediately notice the difference between this plot and the plot of the normal young patient. For one, it extends well beyond the young man’s maximum V/Q ratio, past a V/Q of 10. At that range, there is an obvious excess of ventilation for a region where perfusion is poor. These are the people who present to hospital with hypercapnia in spite of their having a minute volume of 12L/min or more. All that ventilation is wasted on lung regions with a high V/Q.
What Diseases Can Happen When The Mucociliary Escalator Is Not Working Correctly
Some people inherit abnormal genes from their parents and are born with a disease called primary ciliary dyskinesia . PCD is a lung disease that prevents the cilia from beating effectively and, in severe cases, prevents them from moving at all . In PCD patients, the airways become infected due to ineffective mucus transport, which damages the airway cells. When airways become damaged over time, they become floppy, like a collapsed straw, preventing air from moving through them and causing breathing to become difficult. Imagine drinking a thick, delicious milkshake less effort is required when you use a normal-width straw compared with a straw that is the width of a spaghetti noodle.
Chronic obstructive pulmonary disease is a disease that can occur after smoking cigarettes or vaping e-cigarettes. COPD can negatively impact the mucociliary escalator and cause lung disease that looks similar in many ways to CF . Damage to the mucociliary escalator can contribute to other common diseases like pneumonia and asthma, which have similar, but sometimes less severe, problems of mucus.
Also Check: What Is The Blood Test For Eosinophilic Asthma
Limit Your Exposure To Pollutants
Use an air cleaner or purifier at work or at home to reduce indoor dust and fumes. You can also wear a mask, if youre exposing yourself to extra dust, mold, or allergens.
Be aware of days when outdoor air pollution is high. You can find forecasts online for
- pollen counts
- wind speeds and direction when you look up weather forecasts in your area
On days when the air quality index is at an unhealthy range, keep your exposure minimal by keeping doors and windows closed and circulating air inside.
Assessment And Interpretation Of Arterial Blood Gases
An orderly, systematic, multi-level approach is recommended, based on the preceding physiological discussion, perhaps as laid out below. Just how detailed one needs to get will depend on the clinical questions at hand one should ask for what purpose was the blood gas sample obtained? What was the clinical question that needs to be answered? The suggested system is a physiologically based construct, and is not designed to provide pathogenetic diagnosis of any particular disease state. In other words, it is limited to providing quantitative assessment of the severity of gas exchange disturbances, and the physiological factors underlying them. The levels proceed from the simplest to more complex, and, past level 1, require either additional measurements or making assumptions that may or may not be valid in any given situation. As stated previously, the acid/base component of arterial blood gas analysis is beyond the scope of this article and is not addressed.
The minimal requirement is an arterial blood gas sample in which the PO2, PCO2, pH, haemoglobin level and O2 saturation have been measured, although additional measurements will be necessary for some of the derived indices described below .
Examples are shown in and .
Level 3: calculate the physiological shunt and the physiological deadspace , both defined below.
CiO2 = 1.39 Ã Ã fractional O2 saturation + 0.003 Ã PAO2
CaO2 = 1.39 Ã Ã fractional O2 saturation + 0.003 Ã PaO2
Examples are shown in and .
You May Like: Does Smoking Weed Cause Asthma
