Why Is Asthma An Important Public Health Issue
| The negative impact on asthmatics from direct or second-hand smoke is significant. |
The incidence of asthma has been increasing in the last few decades in the developed world,especially amongst children. Asthma is now a serious chronic condition in Ontario and in Canada.Asthma impacts the quality of life of those affected with the disease, as well as their families.According to the 1996-97 National Population Health Survey, more than 2.2 million Canadians hadbeen diagnosed with asthma by a physician at some time in their lives . The same survey found that approximately 10 per cent ofCanadian children and five per cent of adults had asthma at the time of the survey .
The prevalence of asthma in Canadian children aged 0-14 years increased from 141,000 childrenin 1978/79, to 167,000 children in 1983/84, and then to 672,000 children in 1994/95. This is adramatic increase from 2.5 per cent to 11.2 per cent of children under 14 years, over a periodof 18 years.
Asthma is also becoming more prevalent among low-income adults over the age of 35 years. It is notclear at this time whether that higher prevalence can be attributed to lifestyle , residential status, occupation or other factors.
Yet, despite these statistics, 35 per cent of people with asthma were regularly exposed to smoke inside their home. Thus, it is evident that a change in attitudes and behaviors around smoking is especially important for asthma sufferers.
* age standardized to 1991 population
Which Condition Is Associated With The Highest Rate Of Comorbidity With Depression
The most prevalent comorbidities are anxiety disorders,8 substance use disorders9 and other depressive disorders. Epidemiologic studies have shown that the prevalence of at least one lifetime anxiety disorder was 59% in patients with lifetime MDD,10 while the prevalence of substance use disorders in MDD was 14%./span>
The Impact Of Asthma On Daily Life
Asthma is often under-diagnosed and under-treated, particularly in low- and middle-income countries.
People with under-treated asthma can suffer sleep disturbance, tiredness during the day, and poor concentration. Asthma sufferers and their families may miss school and work, with financial impact on the family and wider community. If symptoms are severe, people with asthma may need to receive emergency health care and they may be admitted to hospital for treatment and monitoring. In the most severe cases, asthma can lead to death.
Read Also: Do Inhalers Make You Gain Weight
Prevalence And Symptoms Of Multi
Multi-symptom asthma was detected in 2.0% of the population. No significant differences were found by age, while it was significantly more common among females than males . Subjects with multi-symptom asthma comprised 24.4% of subjects with physician-diagnosed asthma. All investigated symptoms were more common among multi-symptom asthmatics compared with nonasthmatics, while all symptoms except allergic rhinitis were more common compared with subjects with other asthma .
Who’s Strategy For Prevention And Control Of Asthma
WHO recognizes that asthma is of major public health importance. The Organization plays a role in coordinating international efforts against the disease. The aim of its strategy is to support Member States in their efforts to reduce the toll of disease, disability and premature death related to asthma.
Read Also: What Happens If You Smoke Weed With Asthma
Can Asthma Get Worse As You Age
With age, the immune system’s response to inflammation becomes blunted, making it harder to fight off infections that can trigger asthma exacerbations. Other biological changes, notably shifts in patterns of inflammation, may reduce older patients’ response to inhaled corticosteroids that need to be taken daily./span>
Updating Prior To Publication
In order to update the review prior to publication, we undertook forward citation on all included studies . Pursuing references from included studies is an efficient approach to updating systematic reviews as it is unlikely that relevant papers will have been published without citing at least one of the included studies.
You May Like: Does Weight Gain Make Asthma Worse
Reducing The Burden Of Asthma
Asthma cannot be cured, but good management with inhaled medications can control the disease and enable people with asthma to enjoy a normal, active life.
There are two main types of inhaler:
- bronchodilators , that open the air passages and relieve symptoms and
- steroids , that reduce inflammation in the air passages. This improves asthma symptoms and reduces the risk of severe asthma attacks and death.
People with asthma may need to use their inhaler every day. Their treatment will depend on the frequency of symptoms and the different types of inhalers available.
It can be difficult to coordinate breathing using an inhaler especially for children and during emergency situations. Using a spacer device makes it easier to use an aerosol inhaler and helps the medicine to reach the lungs more effectively. A spacer is a plastic container with a mouthpiece or mask at one end, and a hole for the inhaler in the other. A homemade spacer, made from a 500-ml plastic bottle, can be as effective as a commercially-manufactured inhaler.
Access to inhalers is a problem in many countries. In 2019, only half of people with asthma had access to a bronchodilator and less than one in five had access to a steroid inhaler in public primary health-care facilities in low-income countries .
Breastfeeding And The Risk Of Asthma
Literature review
Publications on asthma and breastfeeding were sought from the MEDLINE database for the period 1 Jan. 2000 to 31 Jan. 2003 by searching for publications that contained both of these terms anywhere in their title, abstract or MESH subject headings. We retrieved 27 citations, of which 10 were primary studies that had collected and analyzed information on the independent association of breastfeeding and asthma. Publications pertinent to this area that appeared through to December 2004 were reviewed, but they contained insufficient data to modify the recommendations.
Current evidence
A meta-analysis of prospective studies examining the relation between breastfeeding and asthma reviewed the literature up to 1999. Among the 41 studies reviewed, 12 comprised more than 8000 children whose average age was 4.1 years. Overall, breastfeeding had a protective effect with respect to diagnosed asthma and recurrent wheeze among children with an atopic predisposition . Of interest, the benefit was less pronounced in studies where participants were followed past the age of 2 years. Since the end of 1999, several more studies have examined this association among children < 6 years of age at follow-up, using either prospective or cross-sectional, designs. The results are quite similar to those reported in the meta-analysis breastfeeding appears to be protective against wheezing syndromes early in life in similar populations.
Don’t Miss: Does Smoking Weed Help Asthma
The Economic Burden Of Asthma :
1. Costs to the Health Care System
An estimate of the total cost of asthma in Canada in 1990 is between $504 million and $648 million.Sixty-one per cent of all asthma costs were direct costs such as in-patient care,emergency visits, physician services, nursing services, and drugs. Drug costs were by far the singlelargest component of direct costs , followed by hospital in-patient care and physician services . Indirect costs accounted for $197.7 million and includedthose costs related to travelling, absence from school, disability, and premature deaths. Illness-related disability was the largest contributor to indirect costs , followed by absence from school and premature deaths .
Health Canada data on the economic burden of illness in 1993 for Chronic/Bronchitis/ Emphysema/Asthma combined, reports direct costs of $1.3 billion and indirect costs of approximately $3 billion,for a total cost of $4.3 billion. This more recent cost data does not show the costs of asthma alone,but reveals that the economic burden of these respiratory diseases is a substantial one.
2. Costs to Individuals and Families
Global Alliance Against Chronic Respiratory Diseases:
The Global Alliance against Chronic Respiratory Diseases is part of WHOâs global work to prevent and control asthma. GARD is a voluntary alliance of internationally-recognized organizations, institutions and agencies from a range of countries working towards a common goal of improving global lung health. Its vision is to make the right to breathe freely a reality for all. GARD promotes an integrated approach that capitalizes upon synergies of chronic respiratory diseases with other chronic diseases. GARD focuses specifically on the needs of low and middle income countries and vulnerable populations. The Global Initiative for Asthma , which was formed in 1992 by WHO and the US-based National Heart, Lung and Blood Institute, is part of GARD, as is the Global Initiative on Allergic Rhinitis and its impact on Asthma , in which WHO is a participant. WHOâs Practical Approach to Lung Health , which is a strategy designed to help primary health care workers better manage respiratory symptoms, is used in GARDâs implementation strategy.
Read Also: Can Albuterol Cause Dizziness
Real Life Data On Incidence And Risk Factors Of Severe Asthma Exacerbations In Children In Primary Care
- 25% of children with a severe asthma exacerbation will experience another exacerbation within 1 year.
- 4 out of 1000 children with treated asthma will experience a severe exacerbation per follow-up year.
- The risk of severe asthma exacerbations is the highest in spring and fall.
- A previous asthma exacerbation is the strongest risk factor for subsequent asthma exacerbations.
What Are The Risk Factors Associated With Asthma

| Asthma also affects the quality of life of the families of individuals with asthma |
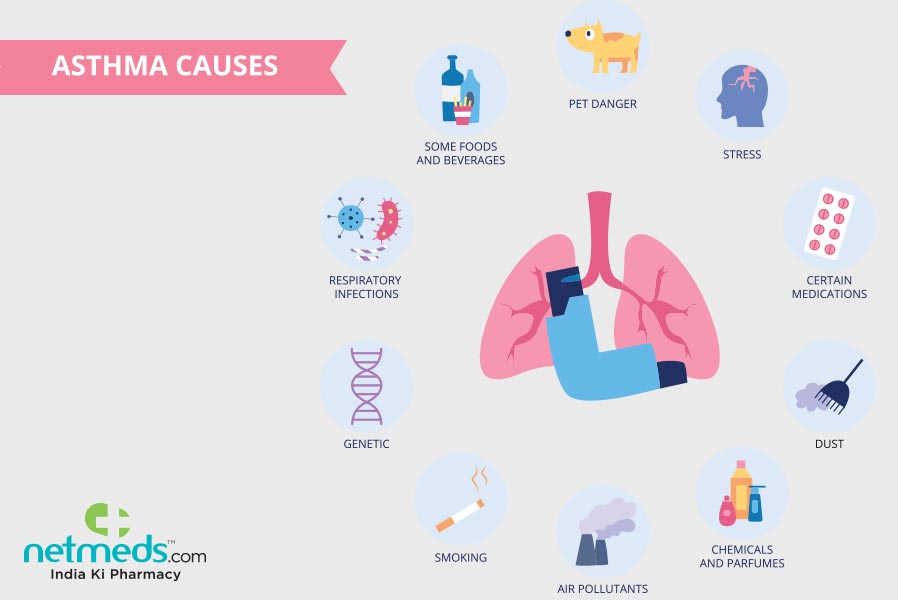
The exact cause of asthma is not known, but it appears to be the result of a complex interaction ofthe following two groups of factors :
1) Predisposing Factors :
Atopy – Atopy is a greater tendency to have allergic reactions to environmental allergens. This appears to be the strongest identifiable predisposing factor for asthma.
Gender – Young boys appear to develop asthma more often than do young girls, probably as a resultof their smaller airways. This imbalance reverses with age however, and by the time girls reachadulthood, it is adult women who more often develop asthma than men.
Genetics – Asthma is more common in families where at least one parent has asthma. This link is even stronger when it is the mother who has asthma.
Solid Food at an Early Age – Although the research is somewhat conflicting, there are indications that children who are breast-fed seem to have a lower risk of developing asthma.
2) Triggers :
| Allergens can include pets, dust mites, cockroach allergen, moulds, pollen, foods and additives. |
Triggers are factors that exacerbate asthma. They are exposures to causal factors that have alreadysensitized a person’s airways. Triggers may be irritants, allergens or viral infections. Some asthmatics may react only to one trigger, others may react to several. Also, an individual’s triggers may change over time.
Two triggers, in particular, are worthy of further discussion :
Recommended Reading: Can Allergies Cause Asthma Attacks
Family History Of Asthma
Blame Mom or Dad or both for your asthma. Your inherited genetic makeup predisposes you to having asthma. In fact, it’s thought that three-fifths of all asthma cases are hereditary. According to a CDC report, if a person has a parent with asthma, they are three to six times more likely to develop asthma than someone who does not have a parent with asthma.
Comparisons To Other Studies
Comparisons with other studies should be interpreted with caution due to varying definitions of disease. The prevalence of current eczema in our study was 13.5 %. Earlier studies addressing eczema in adults have found similar magnitudes of prevalence with 11.6 % in Sweden , 8.1 % in Italy , 14.3 % in Denmark , 11.5 % in Colombia and 10.210.7 % in the United States . Earlier studies of rhinitis have mainly focused on either allergic rhinitis or symptoms of chronic rhinosinusitis. Our definition of current rhinitis included subjects with either allergic rhinitis or other chronic nasal symptoms. The observed prevalence of current rhinitis in our study was 42.8 %. This high prevalence of rhinitis may seem remarkable however, another recent study in Sweden found that the prevalence of rhinitis symptoms was 51 % . Further, 28.1 % in our study reported use of medication against rhinitis in the last year. Allergic rhinitis has also seen a significant increase in prevalence during the last thirty years . The prevalence in Italy has been estimated at 26 % and in southern Finland it has exceeded 40 % .
Also Check: Does Weight Gain Make Asthma Worse
Af And Multiple Risk Factors
The AF was highest for a family history of allergy, which explained 37.1% of the multi-symptom asthma in the study population . In addition, a family history of asthma , female sex , and occupational exposure to gas, dust or fumes were important explanations for multi-symptom asthma. When the AF for occupational exposure to gas, dust or fumes was calculated for males and females separately, the AF for males was 35.3% and for females was 12.5%, reflecting the fact that 56.0% of the males and 24.4% of the females were exposed at work.
Attributable fractions for multi-symptom asthma.
An obvious additive risk effect on OR was seen when analysing the joint effect of family history, occupational exposure and current smoking. Using nonsmoking subjects with no family history of asthma or allergy and no occupational exposure to gas, dust or fumes as a reference, the OR for multi-symptom asthma for subjects with a history of both asthma and allergy, and occupational exposure and/or current smoking was 10.5 .
The effect of interaction between family history, smoking status and occupational exposure on the odds ratios for multi-symptom asthma. : OR 1 whiskers: 95% CI.
Environmental Factors And Asthma
Indoor air pollution such as cigarette smoke, mold, and noxious fumes from household cleaners and paints can cause allergic reactions and asthma. Environmental factors such as pollution, sulfur dioxide, nitrogen oxide, ozone, cold temperatures, and high humidity are all known to trigger asthma in susceptible individuals. In fact, asthma symptoms and hospital admissions are greatly increased during periods of heavy air pollution. Ozone is the major destructive ingredient in smog. It causes coughing, shortness of breath, and even chest pain — and can boost the susceptibility to infection. Sulfur dioxide, another component of smog, also irritates the airways and constricts the air passages, resulting in asthma attacks.
Gas stoves are the primary source of indoor nitrogen dioxide, a common indoor pollutant. Studies show that people who cook with gas are more likely to have wheezing, breathlessness, asthma attacks, and hay fever than those who cook with other methods. It is estimated that more than half of the households in the U.S. use gas stoves.
Weather changes can also result in asthma attacks in some people. For instance, cold air causes airway congestion and an increase in mucus production. Increases in humidity may also cause breathing difficulty in a certain population.
You May Like: Reduce Asthma Symptoms
Implications For Parents And Clinical Practice
Our findings suggest that it is possible to identify the high-risk child with asthma. The factors associated with moderately or greatly increased risk are easily identifiable in routine practice. For example: a history of acute attacks, persistent troublesome symptoms, frequency of prescription requests and comorbid atopic/allergic conditions are recommended components of regular reviews, and knowledge of the social context is a core component of family medicine practice.
Identifying that their child is at-risk enables parents to take decisions about modifying risk, such as reducing exposure to ETS, and reconsidering the necessity for controller treatment against their concern about harms of regular medication. Clinicians alerted to the at-risk child can target care, specifically instituting evidence-based management to reduce risk.
Greatly Or Moderately/greatly Increased Risk Of Attacks
Previous attacks
Previous attacks were consistently associated with a greatly increased risk of future attacks . Due to the consistency of findings and quality of the studies the Panel was highly confident in this assessment .
Poor control and/or persistent symptoms
Ten studies had at least one significant result demonstrating that poor control or persistent symptoms identified a child at moderately/greatly increased risk of future attacks . The exception was a small , short duration cohort study of moderate quality which showed no association. The Panel was highly confident in this assessment. Persistent symptoms of any severity were associated with greater risk.
Poor access to healthcare
Five studies examined access to healthcare defined by insurance status. Four demonstrated that poor access to healthcare was associated with a moderately/greatly increased risk of attacks. A small cohort study of moderate quality demonstrated no increased risk in children with or without Medicaid . The Panel was moderately confident in this assessment. The studies were all US based with participants from deprived inner-city populations: one study controlled for ethnicity and poverty.
You May Like: What Happens If Eosinophil Count Is High
Slightly Increased Risk Of Attacks
ETS exposure
Five studies found at least one positive association between ETS exposure and asthma attacks. One high-quality cross-sectional study highlighted that the association between cotinine levels and risk of attack was lost when parent report was used to estimate ETS. Of note, the three negative studies relied on parental report. The Panel was highly confident that ETS exposure was associated with a slightly increased risk of asthma attack .
Younger age
All six of the studies that examined the effect of age on risk of asthma attacks found that younger children were more likely to have an attack. The ORs ranged from 0.8 to 1.0 the Panel was highly confident of this.
Overweight/obesity
Four studies showed a significant, though small association between overweight or obesity and increased risk of attacks. The Panel was highly confident that there was a slightly increased risk of an attack in overweight or obese children.
Low parental education
All four studies, including one large, high-quality cross-sectional study, showed slightly increased risk of attacks in children of families with low parental education level . The Panel was moderately confident in this assessment.
