Inflammation Mechanism In Asthma
Fig. 3
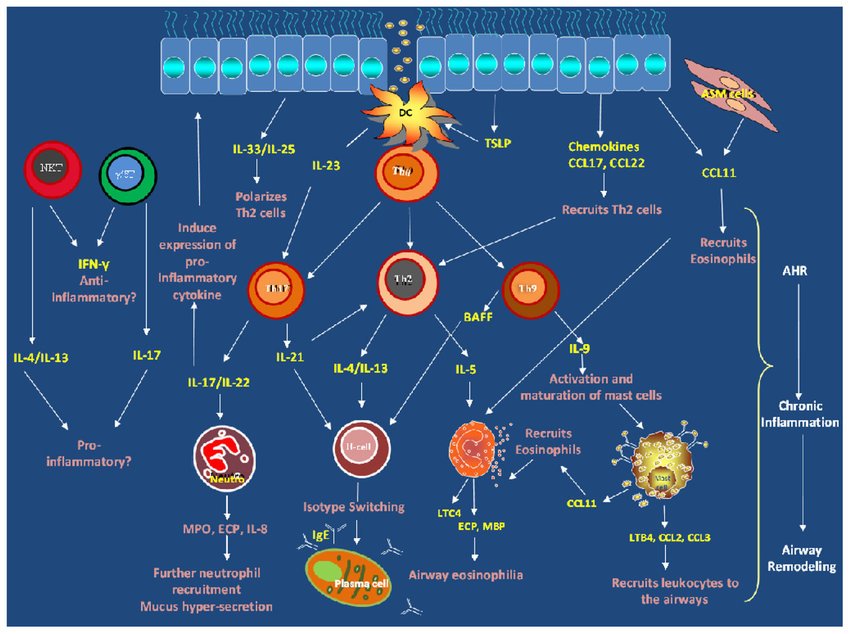
Inflammatory response in asthma: TLRs recognize patterns of allergens . Myeloid DC process allergens and release CCL17 and CCL22 to attract TH2 to injured region. IgE molecules sensitize mast cells to release cysteinyl leukotrienes and PGD2. Damaged epithelial cells release CCL11 to recruit eosinophils which attract more proinflammatory mediators to the damaged region. Eosinophils produce PD1 and PD1 secrets IL10 which promotes macrophage activation . Damaged epithelial cells releases SCF to activate myofibroblast to repair damaged epithelial cells. TLRs: Toll-like-receptors, CCL: CC-chemokine ligand, TH2: T helper cells type 2, IgE: immunoglobulin E, PGD2: prostaglandin D2, SCF: stem-cell factor, PD1: pro-resolving lipid mediators
Summary And Future Directions
This paper reviews key mechanisms of inflammation in airway diseases. It discusses the role of mathematical and computational modeling in furthering our understanding of the complex inflammation mechanism in airway diseases. Results from experimental studies have greatly improved our knowledge of the cellular and molecular events that are involved in the acute inflammatory response to infection and tissue injury in many organs . Experimental studies usually use reductionist approach, so they may fail to describe system-level behavior accurately. Mathematical and computational models can be employed to study the interactions across various biological scales and make predictions for future outcomes of existing interactions based on currently available experimental data.
We recommend that multiscale models should be implemented to test hypotheses that explain how changes at the molecular and cellular-levels may influence the onset and progress of chronic inflammation. Multiscale models should also be used to investigate how chronic inflammation could be caused by prolonged exposure to different kinds/levels of trauma, increased activation and diffusion of chemotactic attractants or high levels of inflammatory cytokines at a site of injury. Multiscale models could be employed to understand the tissue microenvironment effects on inflammation mechanism in young and aged lungs.
Experimental Observation Of Inflammation In Airway Diseases
Asthma and COPD occur due to chronic inflammation of the airways. However, the mechanism of action is different. In asthma, mast cells, eosinophils and CD4 T lymphocytes represent the predominant cell types in the inflammatory process. In COPD, neutrophils, macrophages and CD8 T lymphocytes are the predominant cell types in the inflammatory process . In CF, neutrophils are the predominant cell types in the inflammatory process and they release oxidants, proteases, and elastase that causes respiratory exacerbations .
Aging is a complex process that occurs in different cell types and tissues and is controlled by environmental, genetic, stochastic, epigenetic events and their long-term interactions . Inflammaging is associated with most of the age-related diseases but its precise etiology and potential causal role remain largely unknown . An understanding of the mechanism of lung inflammaging is therefore important in determining whether treatments that modulate inflammaging may be beneficial in combating age-related airway diseases.
Don’t Miss: How To Get Rid Of Asthma Without Inhaler
Environmental Remediation For Asthma
The medical management of asthma and treatment of acute attacks has improved substantially, but the prevalence of asthma continues to rise in urban settings in industrialized Western countries. There is still controversy about the hygiene hypothesis, and it is not yet clear that early exposure to certain antigens could be exploited as a preventive measure. Given what is known about asthma, avoidance of asthma trigger factors would be expected to at least reduce the frequency and severity of symptoms. EPA recommendations for an “Asthma Friendly House” are shown in the iFrame below.
EPA Recommendations Asthma Friendly House
For additional measures, also see the EPA Home Environment Checklist.
There is some evidence that interventions to reduce dust, animal dander, mold, and exposure to cockroaches are effective, but the literature indicates that allergen reduction is difficult to achieve and the effectiveness is not as great as expected. The four articles cited below suggest that environmental remediation interventions that target one or two potential targets are of limited, if any value. However, they suggest that multifaceted interventions can reduce symptoms, school absences, and hospital visits for acute asthma care.
From the Abstract:
Results
Summary:
From the Abstract:
“Evidence synthesis
Summary
Eicosanoid Release From Endogenous Sources
Cell capacity to release eicosanoids from endogenous arachidonic acid was evaluated using ionophore alone. AM, PMN, and PBM released LTB4. No detectable amounts of diHETEs and lipoxins were observed under our analysis conditions in AM or PBM. Nevertheless, besides the normally generated leukotrienes, PMN from untreated asthmatic subjects were able to generate considerable amounts of 5,15-diHETE as well as lipoxins and 6 , respectively). These metabolites were not found in PMN from control subjects.
Also Check: Asthma Cure Without Inhaler
Vasoactive Amines And Peptide
Histamine is released in a quantity of few pictograms from basophils to maintain acute-phase response during inflammation events .
Serotonin is produced via decarboxylation of tryptophan, and it is stored in the granule . In murine, the serotonin is available in basophilic granules, while in humans, it is present in platelets. Four serotonin receptors, namely 5-HTl, 5-HT2, 5-HT3, and 5-HT4, were documented to mediate its biological functions .
Bradykinin is a nanopeptide created from plasma KininKallikrein system . Two or more distinct receptors are present for bradykinins which have been titled B1 and B2 . Similar to histamine and serotonin, it can increase the synthesis of prostaglandins and produces pain locally .
What Happens After Exposure To An Asthma Trigger
For the sake of simplicity, lets assume our subject has allergic asthma with an allergy to dust mites. While other cells also release mediators, well just discuss the ones released by mast cells here.
Early Phase Asthma Attack. After you are sensitized to dust mites, the next time you are exposed to dust mites your immune system recognizes them as harmful. This begins the early phase asthma attack. Mast cells are told to release their contents, which include various mediators of inflammation.
Don’t Miss: Does A Chest Xray Show Asthma
Additional References For Asthma
Mouse Models Of Allergic Asthma
Most asthma related research continues to be pursued using mouse models due to the vast number of immunological and molecular techniques that are available to study them. The development of transgenic and knockout mice has afforded asthma researchers with new technology that enables more comprehensive analysis of mediators involved with the disease .
Mice do not naturally develop asthma, so, an artificial allergic asthmatic-like reaction has to be induced in the airways. There are various sensitization and challenge protocols developed using different strains of mice . The most commonly used strain for allergen challenge is the Balb/C mice because they are known to be high IgE responders to many allergens . Female mice are preferred because they develop greater eosinophilia, influx of immune cells and Th2 responses than their male counterparts .
Don’t Miss: Can Allergies Cause Asthma Attacks
Sputum Mediators In Airway Inflammatory Phenotypes
Differential mediator expression was present between eosinophilic and non-eosinophilic airway inflammation . There was no difference in mediator expression between subjects with asthma and subjects COPD after dichotomising for eosinophilic or neutrophilic airway inflammation .
Fig. 4
Bar chart comparing measured sputum mediators in eosinophilic airway inflammation and non-eosinophilic airway inflammation. Mediators that are marked by an asterisk are significantly different . Horizontal and error bars are set at the geometric mean and 95% CI.
Computational Models Of Inflammation In Asthma
Chernyavsky et al. used a theoretical model to identify the role of inflammation resolution speed in airway smooth muscle mass accumulation in asthma. They present a mathematical model that describes qualitatively the growth dynamics of airway smooth muscle cells over short and long terms in the normal and inflammatory environments often observed in asthma. Their model predicts that long-term airway smooth muscle growth is influenced by the inflammation resolution speed, the inflammation magnitude, and the frequency of inflammatory episodes. Their model highlights the importance of the resolution speed of inflammation in the long-term management of asthma. A limitation of their model is that it does not account for the mechanical interaction of the cells between each other and with the extracellular matrix that could affect the growth and apoptosis rates as well as the total capacity of an airway wall. In addition, the model neglects the spatially heterogeneous and anisotropic growth observed in micrographs and cell hypertrophy .
Their simulation results show that a higher viral load or longer duration of infection provokes a stronger immune response from the macrophage system. Their result also showed that the differences in response to respiratory viral infection in normal and asthmatic subjects skews the system toward a response that generates more severe symptoms in asthmatic patients. Thus, respiratory viral infection can aggravate symptoms in asthmatic patients .
Also Check: How To Get Rid Of Asthma Without Inhaler
Cellular Mechanisms Of Asthma21415
Many cell types are involved in the pathophysiology of asthma. A summary of the interactions between these cells is shown in Figure 27.2, which also shows the principal cytokines that facilitate communication between the cells.
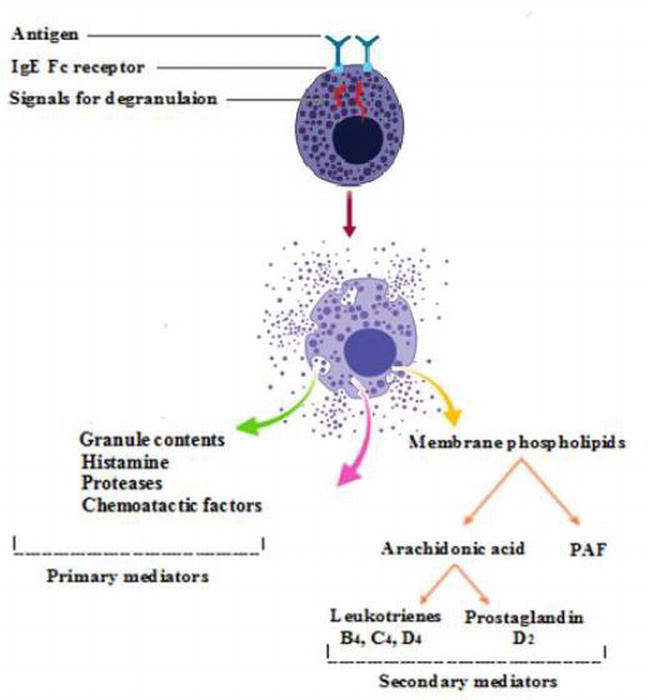
Mast cells are plentiful in the walls of airways and alveoli and also lie free in the lumen of the airways where they may be recovered by bronchial lavage. Mast cell activation is the main cause of the immediate bronchospasm seen in allergen-provoked asthma. The surface of the mast cell contains a large number of binding sites for the immunoglobulin IgE. Activation of the cell results from antigen bridging of only a small number of these receptors, and may also be initiated by complement fractions C3a, C4a and C5a, substance P physical stimulation and many drugs and other organic molecules.
The second major event after mast cell activation is the initiation of synthesis of arachidonic acid derivatives . The most important derivative of the cyclooxygenase pathway is prostaglandin PGD2, which is a bronchoconstrictor, although its clinical significance is still not clear. The lipoxygenase pathway results in the formation of leukotriene C4, from which two further peptide leukotrienes, LTD4 and LTE4, are formed .
Susana Marinho, Adnan Custovic, in, 2008
Airway Inflammation In Asthma And Copd
Airway eosinophilic and neutrophilic inflammation was present in 48 and 35% and in 45 and 59% of asthma and COPD subjects, respectively. Sputum eosinophils were higher in asthma compared to COPD subjects . There was no difference in sputum neutrophil counts between asthma and COPD . Sputum neutrophils but not eosinophils were significantly lower in mild asthma compared to moderate/severe asthma . Sputum eosinophils but not neutrophils were significantly lower in mild/moderate COPD compared to severe COPD .
Fig. 2
Scatter plots presenting differential sputum neutrophil counts and differential sputum eosinophil counts in asthma and COPD subjects grouped according to severity of disease. Horizontal and error bars are set at the mean and SEM and the geometric mean .
Don’t Miss: What Causes Increased Mucus Production In Asthma
Aging And Airway Remodeling
Asthma mortality has declined in the United States, but not in elderly patients. The probability of death from asthma is more than five times higher in elderly asthmatics . Aging affects the lung and chest wall, reducing FEV1 , FEV1/FVC , and FVC , and increasing residual volume . Age-dependent decrements in FEV1 proceed linearly from 25 to 30 years of age through adulthood, then accelerate with increasing age . This deterioration is further accelerated in asthmatic patients . Lung parenchyma structural changes affecting elastic recoil are postulated to underlie peripheral airway narrowing with reduced airway surface-to-volume ratio observed in the elderly . Elderly patients with no known underlying lung disease also manifest alveolar dilation and ductal ectasia without emphysema or fibrosis . The chest wall compliance of elderly patients is reduced by costochondral joint calcification, degenerative joint disease of the spine, and kyphosis . Diaphragmatic weakness and skeletal muscle weakness reduce maximum inspiratory and expiratory pressures . Comorbidities, frailty, and poor nutrition result in respiratory muscle weakness . However, airway remodeling does not appear to occur as an intrinsic feature of aging. Rather, it is an intrinsic feature of asthma, manifesting in a subset of adult asthmatic patients.
Inflammation Mechanism In Copd
Fig. 2
Inflammatory response in COPD: Cigarette pollutants trigger TLRs and apoptotic, necrotic and dead cells release DAMPs . Activated inflammatory cells recruit neutrophils and monocyte to injured region . Recruited inflammatory cells to the injured site release elastase and MMP9, which results in mucus hypersecretion and elastin degradation and emphysema, respectively. Macrophages discharge TGF- which triggers fibroblast proliferation . Airway smooth muscle produces inflammatory cytokines, proteases, and growth factors, which may contribute to the remodeling process. TLRs: Toll-like-receptors, DAMPs: damage-associated molecular patterns, MMP9: matrix metalloproteinase-9 , TGF-: transforming growth factor-
Don’t Miss: Olbas Aromatic Inhaler
What Inflammatory Mediators Are Produced In Asthma
4/5Mast cellscellscell
Mast cells are the central effector cell in allergic disease and are present in increased numbers in the airways of patients with asthma. Binding of allergen to IgE on the cell surface induces a signal transduction cascade that results in the release of mediators.
Furthermore, what is airway inflammation in asthma? Asthma is a long-term disease of the lungs. You might hear your doctor call it a chronic respiratory disease. It causes your airways to get inflamed and narrow and makes breathing difficult. Coughing, wheezing, shortness of breath, and chest tightness are classic asthma symptoms.
Just so, is asthma an inflammatory response?
Asthma is characterized by a chronic allergic inflammatory response in all airways that results in bronchoconstriction, vasodilatation, airway oedema and activation of sensory nerve endings.
What causes bronchoconstriction in asthma?
In acute exacerbations of asthma, bronchial smooth muscle contraction occurs quickly to narrow the airways in response to exposure to a variety of stimuli including allergens or irritants. In addition, other stimuli can cause acute airflow obstruction.
inflammatorystopprevent asthmainflammatoryLeukotriene modifiers include:
Inflammatory Mediators Of Asthma Health Essay
Info: 1430 words Essay 1st Jan 2015 inHealth
Once IgE binds to mast cells , an amplification system operates since the cells not only release the spasmogens and other mediators specified but also can stimulate cells to produce more IgE. Furthermore, the production of IL-5, IL-4 IL-13 and IL-9 amplifies the Th2-mediated events.
It is believed that asthma symptoms are manifested because of Th2 mediated immune response. Pulmonary allergic inflammation in mice lead to decrease in pulmonary IL-5 concentration, specific IgE, IgG1, and eosinophil and T cell recruitment in wild type mice in the absence of T cells. T cells are important in IL-4 dependent IgG1, IgE and Th2 cell mediated lung inflammation, further more there is evidence that CD4+T cells have a role in asthma process. For example, in murine model external protein induced T cells increases IL-5 production and produces airway eosinophilia.
Asthma is a complex chronic inflammatory airway disorder that involves the activation of the inflammatory and structural cells. These released inflammatory mediators cause typical pathophysiological changes of asthma .
Don’t Miss: Can Asthmatics Smoke Weed
Mesenchymal Cells As Effectors Of Airway Remodeling
It is now well-recognized that resident airway smooth muscle cells and fibroblasts drive key cellular and structural features of asthmatic airway remodeling, specifically the increase in ASM mass and subepithelial fibrosis . Paracrine signals from epithelial cells and immune cells may sustain mesenchymal cell activation in the airway wall . Bidirectional crosstalk between the epithelium and the mesenchyme is critical for normal lung development including branching morphogenesis reactivation of this epithelial-mesenchymal tropic unit has been proposed as a driving mechanism in the repair response to chronic injury . Cytokines such as transforming growth factor- and fibroblast growth factors secreted by the mesenchyme instruct the growth and differentiation of epithelial cells, while epithelial growth factor , TGF-, sonic hedgehog , and Wnt proteins from the epithelium direct the proliferation, differentiation, and fate of mesenchymal cells. An aberrantly activated EMTU in combination with inflammatory stimuli, such as the Th2 cytokines IL-4 and IL-13, may sustain the sub-mucosal mesenchymal response by ASM and fibroblasts to execute pathological airway remodeling.
Why Do We Need Animal Models
Humans are the ideal subjects for studying disease pathogenesis. However, for ethical and logistic reasons, most in vivo experiments are carried out in experimental animals . Animal models of asthma afford us the opportunity to design and conduct studies using intact immune and respiratory systems and give us a better understanding of their interaction in the lung . The experimental animal models also allow testing the safety and efficacy of new drugs and therapeutic agents . Although there is no perfect model, several species and study designs have been employed to model allergic airway inflammation and asthma . Animal models of allergic airway inflammation can be credited for highlighting the importance of the Th2 phenotype and various cytokines and chemokines in the development and progression of asthma .
It is important to note that most animals used to study asthma do not spontaneously develop the disease , therefore, they have to be sensitized and challenged with allergens to develop asthmatic-like immune reactions . Due to the complexity of asthma, some models are more suitable for studying the disease than others depending on both practical and research considerations. It is, however, unlikely that a single animal model will be able to replicate all the morphological and clinical features of asthma .
Also Check: Joining Military With Asthma
Mediators Produced By Epithelial Cells
TSLP
The epithelial cells express thymic stromal lymphopoietin with the highest levels in lungs and skin epithelial cells . It was first thought to primarily be a lymphocyte growth factor but it is now clear that TSLP elicits its effects on other cells types, namely DCs, eosinophils, mast cells and ASM cells . Studies in both human and murine models have implicated TSLP in the development and progression of allergic diseases. In mice, TSLP has been found to amplify the differentiation of alternatively activated macrophages therefore contributing to allergic inflammation . Mice challenged with HDM extract in the absence of TSLP receptor showed drastic reduction in allergic inflammation and pro-inflammatory cytokines with decreased eosinophil recruitment in bronchoalveolar lavage fluid and decreased mucus production .
SP-A and SP-D
Activin A
