How Is It Diagnosed
Eosinophilic asthma is diagnosed when a doctor finds elevated numbers of eosinophils in a blood or sputum sample.1,2 Less often, your doctor will perform a bronchial biopsy and count the number of eosinophils in a tissue sample taken from the lungs.
A newer test identifies inflammatory biomarkers for eosinophils in the blood, which gives doctors a more accurate idea of whether the person has EA and which medicines are more likely to control their severe eosinophilic asthma.
Other things your doctor may consider when diagnosing eosinophilic asthma are:
- Medical history and physical examination
- Age of onset
EA is sometimes misdiagnosed as chronic obstructive pulmonary disease .1
How Is The Ige Test Performed
A serum IgE test is performed by drawing a blood sample from a vein by inserting a needle which takes a few minutes. The method is safe and fast and you might feel a slight prick while the needle is being inserted. The blood sample is then tested for specific levels of IgE. The blood collection method includes the following steps. The skin around the vein from which blood is collected is cleaned. An elastic band is tied around the area to make the veins swell up with blood. The point chosen is generally around the elbow or at the back of the palm. A needle is inserted in the vein to draw the blood into a connected syringe. The elastic band is taken off and the needle is pulled out from the skin. In the case of some individuals, it can be difficult to find a vein so the healthcare professional may have to try more than once. For babies, blood is often drawn from the heel area through a tiny needle and the method is often termed as heel stick collection.In some special cases, the test is also done through a collection of the cerebrospinal fluid that surrounds the brain and spinal cord. In these cases, an anesthetic shot is administered to prevent any discomfort during the collection. A hollow needle is inserted in the space between two vertebrae in the lower spine to remove a small amount of the fluid.
When To Discuss The Ige Blood Test
The most common reason for the IgE blood test to be ordered is because of an unknown allergy. The signs and symptoms of allergies will typically be present when this test is ordered. Itching, watery eyes, a runny nose, and a scratchy throat are all common symptoms of an allergic reaction. Some people may develop nausea or having diarrhea that is difficult to control. Coughing, sneezing, and other forms of congestion are also possible.
Someone who may be suspected in having asthma may also have the IgE blood test ordered to screen out the possibility of an allergy causing the symptoms. This includes a tightness in the chest, wheezing, and a feeling of not being able to catch ones breath.
Recommended Reading: How To Breathe Asthma Attack
Targeting Single Vs Multiple Cytokines
While animal models have shown that antibody-mediated neutralisation of Th2 cytokines greatly diminishes airway inflammation , clinical trials of some biological agents have not always been particularly successful with positive trials frequently requiring patient stratification . What has become clear is that the formation of cytokineanti-cytokine immune complexes does not guarantee cytokine neutralisation indeed, the formation of these complexes can, in some cases, potentiate target cytokine activity rather than neutralise it. For example, in a lebrikizumab dose-finding study in moderate-to-severe asthma patients with high periostin levels, there was a direct correlation between exacerbation rate and lebrikizumab dose . Moreover, treatment with neutralising antibodies may also increase cytokine levels in the circulation for example, mepolizumab-treated patients had higher circulating levels of IL-5 with the majority of it bound in IL-5anti-IL-5 complexes , and treatment of asthma patients with anti-IL-13 antibodies directly increased serum levels of IL-13 . These findings would suggest that direct targeting of the cytokine itself might not be particularly effective and that targeting a pathway or multiple cytokines might have a greater clinical effect.
Study Of Serum Ige Levels In Childhood Asthma In Barabanki Region India
Ekansh Rathoria, Utkarsh Bansal, Abhishek Gupta, Nyay Bhai Gupta, Ravindra Ahuja, Richa Rathoria
Abstract
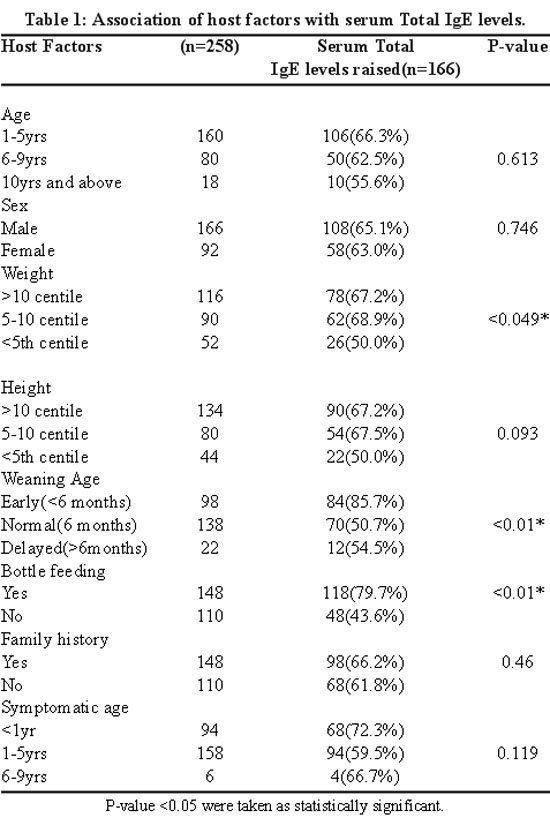
Background: Elevated Serum Immunoglobulin E levels are characteristic of most of the allergic diseases including asthma. Most of the asthma patients are allergic to inhaled antigens and chemical antigens, which lead to their sensitization and induce a state of hypersensitivity that is IgE mediated hypersensitivity reaction. The aim of this study was to estimate and compare serum IgE levels in childhood asthmatics and in normal subjects and to obtain the relationship between serum IgE levels and severity of asthma.
Methods: A stratified sample of 58 patients within the age group of 5-15 years including 36 male and 22 female asthmatic patients and 58 healthy controls within the same age group were included in this study and classified according to GINA classification 2016. Serum IgE levels were estimated by using ELISA kit.
Results: Mean IgE levels ranged from 163.82 IU/mL in normal subjects to 881.81 IU/mL in asthmatics. The mean values of Serum IgE levels in mild, moderate and severe asthmatic children were 625.25 IU/mL, 871.77 IU/mL, 1225.05 IU/mL respectively.
High Serum Immunoglobulin E levels were found in childhood asthmatics as compared to normal subjects. Serum IgE levels were found to increase as the severity of asthma increased. The variability in each grade of asthma was very large so we could not find any statistically significant correlation.
Keywords
Also Check: Are Oil Diffusers Bad For Asthma
Clinical Significance Of Measuring Serum Free Ige Levels
Serum free IgE decreases rapidly following the administration of omalizumab, and this decrease is maintained with continuous therapy. In a clinical study of 240 patients with allergic rhinitis who were administered omalizumab for 12 weeks, although symptoms improved in the groups with serum free IgE levels of < 20 ng/ml and > 40 ng/ml, symptoms improved more markedly in the < 20 ng/ml group. Furthermore, there was no difference observed between the < 40 ng/ml, > 100 ng/ml, and < 100 ng/ml groups.
Based on these results, the clinical target level of a patients total serum IgE in omalizumab therapy is 30 ng/ml . The omalizumab dose is calculated from the patients pre-treatment total serum IgE levels and body weight however, at present, there is no proposal to revise and recalculate the dose from IgE levels after initiating treatment from the study groups, and there is no specific recommendation for revising the dosage of omalizumab from the manufacturer.
Omalizumab Therapy Indications And Therapeutic Effects
Omalizumab treatment is considered for both adults and children aged 6 years with serum total IgE levels of 30150 IU/ml and poorly controlled severe atopic asthma despite treatment at step 5, according to the GINA guidelines. The therapeutic effects of omalizumab therapy are determined at 16 weeks, at which time it is recommended to examine whether treatment should be continued. The European Respiratory Society and American Thoracic Society guidelines regarding severe asthma note that, although the increased use of medical resources is an issue, omalizumab appears to be beneficial .
Several clinical studies have demonstrated the effectiveness of omalizumab in the treatment of severe asthma . In a Cochrane collaboration review of 19 clinical trials, upon examining the effect of omalizumab therapy as an adjunct to oral steroids, observations from weeks 1660 revealed a significant inhibitory effect on asthma exacerbation . Exacerbation was observed in 26% of the placebo group, in contrast to only 16% of the omalizumab therapy group . Furthermore, it was reported that, during observations from weeks 2860, the risk of hospitalization due to exacerbation was 3% in the placebo group and 0.5% in the omalizumab therapy group, with a significantly lower risk of hospitalization in the latter group .
Read Also: What Is An Asthma Flare
What Does It Mean If My Ige Level Is High
The Role of IgE Symptoms Caused by Excess IgE Diagnosis IgE Testing High IgE Levels Allergic Conditions Infections Autoimmune and Inflammatory Diseases Blood-Related Cancers Other Conditions Treatment for High IgE Levels A Word From Verywell Frequently Asked QuestionsRelated contentVideos
Asthma can be described as allergic or non-allergic. Allergic asthma is associated with immunoglobulin E an antibody generated by the immune system, in this case, in response to a normally harmless substance. In contrast, non-allergic asthma episodes are not typically triggered by exposure to a substance and are not associated with IgE.
IgE plays a key role in allergic responses, however it can sometimes be elevated for other reasons, such as chronic infections or inflammatory diseases. Additional testing is often needed and depends on symptoms.
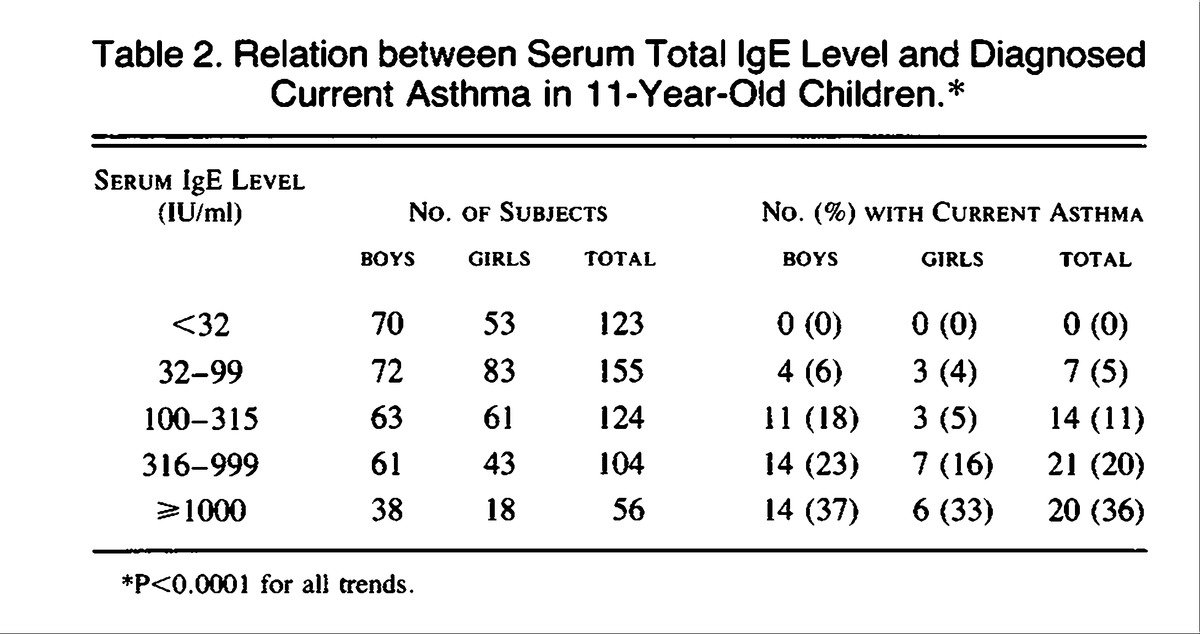
Children who have asthma are more likely to have elevated IgE levels than adults with asthma. Asthma that begins for the first time during adulthood, called adult-onset asthma, is more likely to be intrinsic, non-allergic asthma.
Given the role of IgE in certain asthma cases, treatment may involve an anti-IgE medication to lower amounts of this antibody and its effects. A blood test to check your levels can help determine whether this may or may not be useful in your case.
What Is The Role Of Eosinophils In Severe Asthma
Eosinophils were first identified in the late nineteenth century and eosinophilia has been known to be associated with a wide variety of conditions, including asthma and atopic diseases . The relatively recent discovery of IL-5, in 1980 , its interaction with eosinophils, and subsequent results of anti-IL-5 blocking mAb treatment in patients with asthma confirmed the importance of IL-5 in eosinophil-mediated inflammation in humans .
Accumulation of eosinophils at the bronchial level causes damage by degranulation and release of toxic proteins such as eosinophil-derived neurotoxin, eosinophil cationic protein, eosinophil peroxidase, and major basic protein. Airway remodelling is the consequence of ongoing inflammation and repair, and there is increasing evidence that eosinophils are important in the pathophysiology of this process in both allergic and non-allergic asthma. Even though the main, and well-known, function of eosinophils relate to the induction of bronchial wall damage as final effector cells, they also represent the source of a number of regulatory and pro-inflammatory cytokines and chemokines .
Effective antigen presentation to Th cells by human eosinophils has been recently confirmed. In fact, GM-CSF-stimulated human eosinophils can act as antigen-presenting cells to stimulate Th-cell responses against a range of antigens including allergens, an ability that may help the development of allergic disease .
You May Like: Can Asthma Just Show Up
Symptoms Of Conditions That Increase Ige
There are no symptoms associated with high IgE levels per se. Instead, people with high IgE may only show symptoms of conditions discussed above. Your doctor will discuss your results with you. They may run additional tests to pinpoint the underlying cause of your high levels.
In most cases, the levels increase as a consequence of an allergic response with the symptoms such as :
- Itchy skin and eyes
- Fatigue
Efficacy Of Omalizumab Therapy In An Asthmatic With Low Ige
1Department of Pulmonary Medicine, Rajagiri Hospital Chunangamvely, Aluva, 683112, Kochi, Kerala, India
Abstract
Asthma is one of the most common respiratory diseases encountered in clinical practice. Although the vast majority of asthmatics can be adequately controlled with inhaled steroids and other preventer medications, a small proportion remain uncontrolled. Anti-IgE treatment with omalizumab has been proposed in patients as a preferred approach in step 5 asthma therapy according to GINA guidelines. Although therapy with this molecule is approved for patients with atopic asthma and pretreatment serum IgE levels of 30-1500 only, there have been a few reports of its efficacy in subjects outside this reference IgE range. We report the case of a middle-aged lady with severe corticosteroid-dependent asthma and low serum IgE levels who was successfully treated with 9 months of omalizumab therapy. She gained good asthma control and was tapered off steroid use by the fifth month of therapy with omalizumab. The case report stresses the need for further investigation into expanding the spectrum of omalizumab usage in asthma beyond the current IgE suitability range.
1. Introduction
2. Case Report
You May Like: Can You Be In The Fbi With Asthma
Clinical And Laboratory Tests For The Detection Of Allergen Specific Ige Antibodies
Allergy Skin Tests
Prick skin tests can be used to identify specific IgE sensitization. The skin is marked for testing with a panel of appropriate allergens for the patient, selected on the basis of the clinical history and knowledge of the allergens commonly found in the locality. Positive and negative comparator tests using histamine and saline also should be performed to prove that the skin is capable of demonstrating a positive reaction and to prevent the interpretation of false-positive results occurring as a result of dermatographism.
In-vitro tests for specific IgE antibodies.
The discovery of IgE allowed the development of immuno-assays for IgE and IgE-antibodies, enabling direct and objective measurement of the extent and specificity of the immune response. Immunoassays such as RAST ,, FAST and ELISA have been developed each using a different detection system. For each assay, allergens are linked to paper discs or polyurethane caps and are incubated with the individual’s serum. Binding of IgE specific to allergens is detected by the use of an enzyme linked anti-human IgE antibody leading either to a colorimetric or fluorescent product that can be measured. There is a good correlation between the results of serum tests for IgE antibodies, and positive skin and provocation tests, as well as symptoms of allergy. Positive in-vitro results to a specific allergen demonstrate IgE sensitization but are not proof that the allergen is the cause of clinical symptoms.
Heres What You Need To Know
The only way to proactively avoid having high IgE levels is to avoid the things that may be causing an allergic reaction. The levels of antibodies in the blood are not affected by the amount of exercise a person performs daily or the foods they choose to eat.
Doctors that specialize in diagnosing allergies will often perform this test within their own offices. General family providers will typically send out the sample for analysis and receive results in 3-5 business days. If the test is positive, then further testing may be required to determine the extent of the allergy.
One of the usual tests outside of the allergen-specific IgE blood tests is the allergen skin test. In this test, the skin is pricked so that it will bleed. Then the suspected allergens are exposed to the blood to determine if an allergy develops. Positive skin test results for allergies will cause a red swelling to occur at the application site. Multiple skin pricks are required for each allergen, so it is not typically a test that is performed unless all other detection methods have been exhausted.
Having uncontrolled allergies may not seem serious, but they can be. A severe allergic reaction may cause swelling in the face and throat, making it difficult to breathe. That type of reaction is always treated as a medical emergency.
Recommended Reading: How To Improve Asthma Naturally
Asthma And Ige Levels In Rural And Urban Communities Of The Gambia
R. C. GODFREY
Faculty of Medicine, University of Southampton and MRC Laboratories, Fajara, The Gambia, West Africa
R. C. GODFREY
Faculty of Medicine, University of Southampton and MRC Laboratories, Fajara, The Gambia, West Africa
Get access to the full version of this article.You previously purchased this article through ReadCube.
Institutional Login
Log in to Wiley Online Library
If you have previously obtained access with your personal account, please log in.
- View the article/chapter PDF and any associated supplements and figures for a period of 48 hours.
- Article/Chapter can not be printed.
- Article/Chapter can not be downloaded.
- Article/Chapter can not be redistributed.
- Unlimited viewing of the article/chapter PDF and any associated supplements and figures.
- Article/Chapter can not be printed.
- Article/Chapter can not be downloaded.
- Article/Chapter can not be redistributed.
- Unlimited viewing of the article/chapter PDF and any associated supplements and figures.
- Article/chapter can be printed.
What Should You Know About Ige Levels
IgE can be easily measured after taking some blood samples. The normal or expected concentration of IgE is low compared to other antibody isotypes. The normal range of IgE is between 4.2 and 592 U/ml. Ant IgE level above 592 U/ml is considered as a high IgE concentration.
Elevated IgE levels are typical for people suffering from allergies , asthma, atopic dermatitis, certain types of cancers and in case of autoimmune diseases. High IgE levels are also a characteristic of Job syndrome, a rare immunodeficiency disorder. Atopic people may have up to 10 times bigger level of IgE than normal. They are prone to allergic illnesses and may develop asthma, hay fever and other allergic diseases.
Low levels of IgE are connected to rare immunodeficiency diseases and may also be a characteristic of a rare inherited illness called ataxia telangiectasia.
You May Like: Is Asthma A Chronic Medical Condition
Immunoglobulin E And Allergic Asthma
Asthma can be described as allergic or non-allergic. Allergic asthma is associated with immunoglobulin E an antibody produced by the immune system, in this case, in response to a normally harmless substance. In contrast, non-allergic asthma attacks are usually not triggered by exposure to a substance and are not associated with IgE.
Please enable JavaScript
Given the role of IgE in some cases of asthma, treatment may involve anti-IgE drugs to reduce the amount of this antibody and its effects. A blood test to check your levels can help determine if this is useful in your situation.
The Discovery Of Ige And Its Role In Allergic Inflammation
While the discovery of IgE in 1966 brought to an end the search for the elusive reagin, it unlocked an era of discovery that investigated the genetics, structure, functions and clinical applications of this immunoglobulin . As has been recognised since the early part of the twentieth century, IgE has unique properties among the immunoglobulin isotypes in its abilities both to induce extremely rapid pathological responses and to act as a highly sensitive immunological amplifier. Furthermore, it is well established that IgE levels are increased in patients affected by atopic conditions and that IgE provides the critical link between the antigen recognition role of the adaptive immune system and the effector functions of mast cells and basophils at mucosal and cutaneous sites of environmental exposure . These functions have made IgE an attractive target for pharmacological intervention with IgE blockade having clinical potential across many different therapy areas.
Recommended Reading: Will Allergy Shots Help My Asthma
