What Is An Asthma Attack
When you breathe normally, muscles around your airways are relaxed, letting air move easily and quietly. During an asthma attack, three things can happen:
- Bronchospasm: The muscles around the airways constrict . When they tighten, it makes your airways narrow. Air cannot flow freely through constricted airways.
- Inflammation: The lining of your airways becomes swollen. Swollen airways dont let as much air in or out of your lungs.
- Mucus production: During the attack, your body creates more mucus. This thick mucus clogs airways.
When your airways get tighter, you make a sound called wheezing when you breathe, a noise your airways make when you breathe out. You might also hear an asthma attack called an exacerbation or a flare-up. Its the term for when your asthma isnt controlled.
What Should I Do If I Have A Severe Asthma Attack
If you have a severe asthma attack, you need to get immediate medical care.
The first thing you should do is use your rescue inhaler. A rescue inhaler uses fast-acting medicines to open up your airways. Its different than a maintenance inhaler, which you use every day. You should use the rescue inhaler when symptoms are bothering you and you can use it more frequently if your flare is severe.
If your rescue inhaler doesnt help or you dont have it with you, go to the emergency department if you have:
- Anxiety or panic.
- Bluish fingernails, bluish lips or gray or whitish lips or gums .
- Chest pain or pressure.
- Very quick or rapid breathing.
New Gina Recommendation For Mild Asthmatics
At the time the 2019 GINA Report was published, neither BUD-FORM nor BDP-FORM had been registered as on-demand relievers when not used in maintenance treatment nonetheless, the GINA experts issued this recommendation. For safety reasons, GINA no longer recommends using SABAs as monotherapy.
GINA experts recommend low-dose ICS-FORM as needed as the preferred treatment option during the first step of treatment for patients who suffer from asthma symptoms less than twice per month and who are not at risk of exacerbation. An alternative option is the use of low-dose ICS whenever SABA is taken. Maintenance use of low-dose ICS was recommended in 2014 for patients with risk factors, but this therapy is no longer recommended due to the low rate of compliance in these patients and the risk of exposing them to SABA-only treatment.
In addition to the other preferred options, low-dose ICS-FORM as needed and low-dose ICS and SABA as needed were added by experts to the list of potential options for the second step of treatment. The alternative options include low-dose ICS whenever SABA is taken as well as a leukotriene receptor antagonist.
What changes have caused these recommendations to appear?
Read Also: How To Soothe Asthma Without Inhaler
The Reasons For Changes In The Gina Guidelines
The results of these studies coincided with the publication of alarming epidemiological data from England and Wales, which showed the growing trend of deaths from asthma. In the last decade, the number of deaths due to asthma has increased there by 25%, reaching the highest number per year in this century .
Since effective, safe medications are available and the recommendations for how to effectively treat asthma are commonly known, what is causing this increase?
One of the problems seems to be the overuse of SABA in monotherapy by patients with mild asthma. Therefore, for safety reasons, GINA no longer recommends treatment using only SABA monotherapy in any step.
The introduction of symptom-driven treatment that combines RABA and ICS in the first step of therapy unifies the message of the principles of treating this disease, which had up to now been contradictory. From the beginning, it has been commonly known that asthma is an inflammatory disease, but anti-inflammatory drugs were recommended only in the second step of therapy. Another problem was the ambiguous message given to patients: on one hand, the recommendations assumed freedom in the use of drugs by patients during the first step of therapy, but on the other hand, these recommendations were much stricter and more inflexible during the second through fifth steps of therapy.
Is Your Asthma Still Mild Persistent
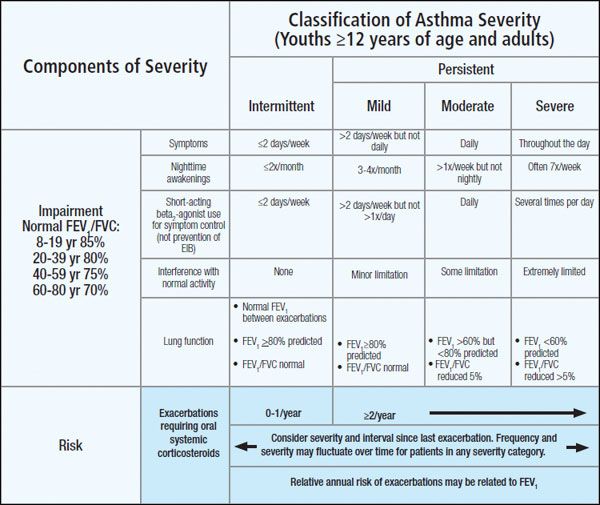
Intermittent asthma is the mildest form of asthma, with infrequent symptoms and no interference with normal activity. It is possible that, with proper trigger control and treatment, your mild persistent asthma could be downgraded to this classification.
On the other hand, while your disease can worsen due to circumstances that are out of your control, like genetics, factors like frequent exposure to asthma triggers or skipping your medications can worsen your asthma severity and push you into a more severe classification.
Moderate persistent asthma affects your daily activities and requires daily use of short-acting inhalers.
If you experience symptoms throughout the day, you may be diagnosed with severe persistent asthma.
It’s a good idea to know what differentiates mild persistent asthma from the other classifications so that you can talk to your healthcare provider if your symptoms seem to be changing. In that case, it’s quite possible that your asthma classification may have changed as well.
The classifications are helpful for gauging changes in your disease. When re-evaluating you case, your healthcare provider will carefully evaluate your symptoms and diagnostic tests while taking into account the fact that your medication use colors how criteria can be considered.
You May Like: What To Do If Someone Passes Out From Asthma Attack
Mild Persistent Asthma: Is Any Treatment Needed
Asthma is a chronic inflammatory disease caused by airway inflammation found in the airways and lungs. This further leads to limited airflow and difficulty in breathing. As per the American Lung Association, it is the most common chronic condition found among children. Both mild asthma and severe asthma often develop in childhood, although even adults can develop it at a later stage. While asthma cannot be cured completely, it is still possible to find asthma control with a proper line of treatment.
Asthma severity can differ from person to person. Sometimes, the people suffering from asthma may show very mild effects, meaning they require little to no medical treatment. On the other hand, people can also have some severe effects and may require daily treatment with asthma medication to keep it under control. The frequency and severity of asthma majorly lie between these two ends.
Generally, people who dont show asthmatic symptoms daily but for more than two days a week may have mild persistent asthma. So, is it risky? Do you need a special asthma management plan and treatment in this case? Read on to find more about mild persistent asthma.
Current Treatment Recommendations For Mild Persistent Asthma
Asthma treatment guidelines have been consistent in describing the goals and objectives of asthma treatment. These are to: 1) minimise or eliminate asthma symptoms 2) achieve the best possible lung function 3) prevent asthma exacerbations 4) do the above with the least possible medications 5) minimise short- and long-term adverse effects and 6) educate the patient about the disease and the goals of management 2. In addition to these goals and objectives, each of these documents has described what is meant by the term asthma control. This includes the objectives above but also includes minimising the need for rescue medications, such as inhaled 2-agonists to less than daily use, minimising the variability of flow rates that is characteristic of asthma, as well as having normal activities of daily living. Some of these outcomes can be regarded as patient centred, which are outcomes that the patient would regard as obvious benefits of treatment, such as eliminating asthma symptoms, preventing severe exacerbations, normal activities of daily living and minimising medication adverse effects. Other outcomes can be considered as physician centred, particularly measurements of lung function, which are very important in establishing asthma control but changes in which are often not recognised by the patient. This distinction is particularly important in studies of mild asthma, where lung function is already normal.
Recommended Reading: Little Rock Allergy And Asthma Clinic
Risk Of Asthma Exacerbation In Patients Overusing Saba Or Using Them In Monotherapy
Later, Stanford et al. determined the magnitude of the risk of asthma exacerbation depending on SABA demand. Based on two large databases, researchers calculated that the consumption of 3 or more SABA canisters within the previous year increased the risk of asthma exacerbation. For adults, such a marker may be the use of 2 or more SABA canisters in a shorter 36 month period. The use of an additional SABA canister resulted in a corresponding increase in the risk of asthma exacerbation by 8% to 14% and 14% to 18% in children and adults, respectively.
In a survey conducted by Price et al. in eight Asian countries, only 14.5% of respondents taking exclusively rescue medications had controlled asthma, and two-thirds had experienced severe exacerbations in the previous year. Unfortunately, in this study, similar proportions of adverse events were also found in the group taking controller medications, which may be because respondents confess that they fear the regular use of asthma drugs and then only take them occasionally additionally, most of these patients could not correctly identify drugs for asthma prescribed by doctors.
The Evolution Of The Treatment Of Intermittent / Mild Asthma
Asthma severity is assessed retrospectively from the level of treatment required to control symptoms and exacerbation. Therefore, this parameter is not a static feature but may change over time, and can be assessed when the patient has been on controller treatment for several months allowing to distinguish mild, moderate and severe asthma. The asthma severity model was the foundation for the stepwise approach to asthma management, which goal is to achieve good symptom control and to minimize future risk of asthma-related mortality, exacerbation, persistent airflow limitation and side-effects of treatment. In order to achieve these goals, appropriate pharmacological treatment should be accompanied by optimal non-pharmacological strategies which include education of patients for self-management and correct use of devices, environmental control for airway irritants and specific allergens and identification and treatment of comorbidities .
The risks of SABA overuse were the focus of extensive research in the 1980s and 1990s which showed an increased risk of death . Concurrently, randomised controlled trials found no advantage in regular versus as-needed SABA so that, by the late 1990s, most guidelines recommended as-needed rather than regular SABA. In parallel, many authors highlighted the protective role of regular use of ICS which resulted associated with a dramatic reduction in the risk of asthma-related hospitalisations and death.
Read Also: Can Asthma Cause Coughing And Mucus
What Are Common Asthma Attack Triggers
You can have an asthma attack if you come in contact with substances that irritate you. Healthcare providers call these substances triggers. Knowing what triggers your asthma makes it easier to avoid asthma attacks.
For some people, a trigger can bring on an attack right away. For other people, or at other times, an attack may start hours or days later.
Triggers can be different for each person. But some common triggers include:
Other Characteristics Of Your Diagnosis
In addition to classifying your asthma based on its severity, you will also be diagnosed with a specific type of asthma. There are several, and they are based on triggers.
For example, if you meet the above criteria and physical activity is what brings on your asthma symptoms, you likely have mild persistent exercise-induced asthma. If exposure to pollen exacerbates your condition, you likely have mild persistent allergic asthma.
On follow-up visits, your healthcare provider may also assess your asthma as well-controlled, not well controlled, or very poorly controlled based on criteria that include nighttime awakenings, rescue inhaler use, and lung function.
Asthma control is not the same as asthma classification, but it also helps guide your treatment, especially because it may be difficult for your healthcare provider to reassess your asthma without medication if you rely on it.
Recommended Reading: Which Of The Following Are Associated With Extrinsic Asthma
Mild Persistent Asthma Criteria
Asthma is classified based on several factors, including the frequency, severity, and impact of symptoms on daily activities.
Your healthcare provider will consider your medical history, perform a physical examination, and order diagnostic tests to determine if your asthma is mild persistent or not. The first time this is done, they will base the assessment on your asthma symptoms and test resultswithout treatment.
How Do Healthcare Providers Diagnose Asthma
Your healthcare provider will review your medical history, including information about your parents and siblings. Your provider will also ask you about your symptoms. Your provider will need to know any history of allergies, eczema and other lung diseases.
Your provider may order spirometry. This test measures airflow through your lungs and is used to diagnose and monitor your progress with treatment. Your healthcare provider may order a chest X-ray, blood test or skin test.
Recommended Reading: Is Broccoli Good For Asthma
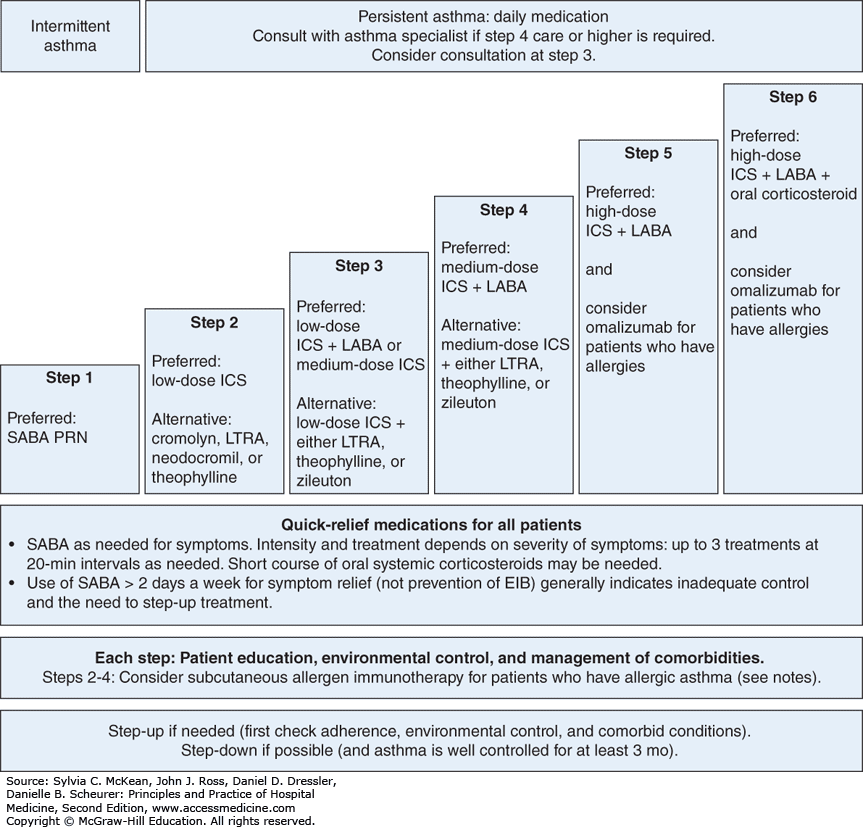
Wise Approach To Asthma Treatment In Adults
Current national and international asthma guidelines recommend a five-step approach to treatment . Treatment is based on regular patient education, checking the patients inhaler technique, reducing asthma triggers , and treatment of comorbidities . Potential workplace-related asthma triggers should be identified and eliminated in some cases a change of workplace or occupation may be unavoidable .
Stepped approach to pharmacological therapy according to the German National Disease Management Guideline 2020
Following GINA, the German National Disease Management Guideline recommends a five-step approach to treatment. Depending on the level of asthma control, medications are stepped up or down until good asthma control is achieved with as few medications as possible at the lowest possible dosage.
Modified from .
*1 Fixed-dose combination on an as-needed basis is not approved for steps 1 and 2
*2 ICS+formoterol as needed if this combination is also used for maintenance therapy
GINA, Global Initiative for Asthma ICS, inhaled corticosteroid LABA, long-acting 2-agonist LAMA, long-acting muscarinic antagonist
LTRA, leukotriene receptor antagonist OCS, oral glucocorticosteroid SABA, short-acting inhaled 2-agonist
What Asthma Treatment Options Are There
You have options to help manage your asthma. Your healthcare provider may prescribe medications to control symptoms. These include:
- Bronchodilators: These medicines relax the muscles around your airways. The relaxed muscles let the airways move air. They also let mucus move more easily through the airways. These medicines relieve your symptoms when they happen and are used for intermittent and chronic asthma.
- Anti-inflammatory medicines: These medicines reduce swelling and mucus production in your airways. They make it easier for air to enter and exit your lungs. Your healthcare provider may prescribe them to take every day to control or prevent your symptoms of chronic asthma.
- Biologic therapies for asthma: These are used for severe asthma when symptoms persist despite proper inhaler therapy.
You can take asthma medicines in several different ways. You may breathe in the medicines using a metered-dose inhaler, nebulizer or another type of asthma inhaler. Your healthcare provider may prescribe oral medications that you swallow.
Also Check: Acid Reflux And Asthma Symptoms
Avoid Asthma Triggers In The First Place
Whether your doctor has identified the stage and severity or is yet to do the same, it is essential to identify what triggers your asthma symptoms. Avoiding them or reducing your exposure to them can help prevent and control your asthma flares, so you can avoid a severe asthma attack.
Outlined below are five ways to avoid your asthma triggers:
Dust-proof your home: Clean your home as much as you can as dust mites can trigger asthma. If your home has carpets, remove them. Wash the linens regularly and use dust-resistant bedding.
Use an air conditioner: While natural air may be enticing, it can trigger asthma as it brings along humidity, pollen, and grasses. Its best to use an air conditioner to eliminate exposure to these outdoor irritants.
Protect your face: Again, when you breathe cold air, you are at high risk of experiencing asthma flares. So, to be on the safer side, it is recommended to cover your face with a scarf or mask whenever you step out of your house.
Clean regularly: Clean the damp areas of your home at regular intervals to prevent mold accumulation. Also, remove mold traps like leaves or firewood from your yard.
Stay healthy: People experiencing normal flu or common cold can also be at higher risk of experiencing more asthma symptoms. Get required vaccines, make a habit to wash hands during seasonal transitions.
Types Of Asthma And Biomarkers
Types of asthma and biomarkers
In adults, two common types of asthma are distinguished: allergic asthma, where there is a clear relationship to allergy, and intrinsic or eosinophilic asthma, which usually starts in adulthood without evidence of any relevant allergies.
In adults, two common types of asthma are distinguished. The first is allergic asthma, where there is a clear relationship with allergy. Onset is often during childhood or adolescence and often accompanied by allergic rhinitis and/or atopic dermatitis this form is known as early-onset asthma. The second is an intrinsic type, usually with onset in adulthood and usually without evidence of any relevant allergies this form is referred to as adult-onset or late-onset asthma) . In both types of asthma, an increased level of typical cytokines and eosinophil granulocytes is found, together with dysfunction of structural cells characteristics referred to collectively under the name type 2 asthma . The inflammation can be measured through biomarkers . Routine diagnostic procedures covered by statutory health insurance carriers in Germany include blood eosinophil count and allergy markers fractional exhaled NO measurement is available as a self-pay option. It should be noted that these biomarkers can be falsified: for example, eosinophil counts can be greatly reduced by inhaled or oral steroids and FeNO levels by tobacco smoke .
Don’t Miss: How To Get An Asthma Inhaler
Pharmacological Basis Of The Bud
In 1996, Schreurs et al. demonstrated the dose-dependent effect of formoterol in the maintenance therapy of patients with moderate asthma. Compared to placebo, 6 g formoterol b.i.d. was found to be the lowest effective dose for improving the morning and evening peak expiratory flow . Increasing the dose from 6 to 24 g b.i.d. provided an additional effect of 18 L min1 in the evening PEF. In 1998, Malolepszy et al. demonstrated the effectiveness and safety of formoterol at high doses in the treatment of acute severe airway obstruction. Adult patients with asthma and COPD who had been admitted to intensive care units with acute severe bronchoconstriction were randomized to receive 20 inhalations of either formoterol or terbutaline within the first 3 h of therapy, but all received 40 mg of methylprednisolone i.v. in the 90th min of therapy. High doses of formoterol were equally as effective as terbutaline in improving lung function. Additionally, formoterol therapy resulted in significantly lower pulse rates than terbutaline therapy, which confirmed the safety profile of formoterol administered in high doses. Five years later, a similar study was performed comparing formoterol with salbutamol in an emergency setting . In this study, using 54 µg^ of formoterol compared to 3600 µg of salbutamol resulted in greater acute lung function improvement over the 4-h assessment period.
