Combination Ics/laba Controller Medications
LABA is recommended in combination with ICS for long-term control and prevention of symptoms in patients aged 5 years or older who have moderate or severe persistent asthma or asthma that is inadequately controlled by ICS alone. ICS and LABA can be administered via separate inhalers or via a single inhaler containing both drugs. Two single-inhaler ICS/LABA therapies are currently available and have been demonstrated to be effective and well tolerated: budesonide in combination with formoterol,2326 and fluticasone in combination with salmeterol.2731 Fluticasone/salmeterol is indicated for use in children aged 4 to 11 years, as well as in adolescents and adults.32 Currently, budesonide/formoterol pressurized metered-dose inhaler is indicated for use in individuals aged 12 years or older in the United States.33 Outside the United States, budesonide/formoterol dry powder inhaler 80/4.5 g and 160/4.5 g doses are approved for patients aged 4 years or older, and the 320/9 g dose is indicated for patients aged 12 years or older.
Preferences For Asthma Treatment
Among the participants, 80.4% replied with consistent responses to the pair of consistency questions. Overall, patients strongly preferred attributes related to greater levels of reduction in the frequency of severe asthma attacks, greater levels of improvement in lung function, and no black box warning issued by the FDA for the risk of a life-threatening allergic reaction . Participants preferred treatments administered at home rather than at a doctors office or clinic and those that could also treat one or more additional chronic conditions over those that did not have such a benefit . Dosing frequency and the type of device used for the subcutaneous injections did not significantly affect participants preferences for asthma treatments.
|
Table 4 Preferences for Attributes of Biologic Treatments for Asthmaa |
Onset Of Bronchodilator Action Of Fixed
One characteristic that differs between budesonide/formoterol and fluticasone/salmeterol with the potential to influence patient preference is the onset of effect. Comparative trials have shown that formoterol has a rapid onset of effect, similar to that of albuterol, and significantly more rapid than that of salmeterol.41,42 Similar results have been found in randomized, crossover studies with the combination inhalers budesonide/formoterol and fluticasone/salmeterol. When both combinations were delivered by DPI, budesonide/formoterol showed a significantly faster onset of bronchodilatory action than fluticasone/salmeterol , as measured by mean forced expiratory volume in 1 second at 3 minutes after inhalation.43,44 Likewise, a comparison of the bronchodilatory effects of budesonide/formoterol pMDI , fluticasone/salmeterol DPI , and albuterol pMDI showed that the improvement in FEV1 observed at 3 minutes after dosing was significantly greater with budesonide/formoterol pMDI than with fluticasone/salmeterol DPI, and similar to that with albuterol pMDI.45
Recommended Reading: What Is An Asthma Attack Like
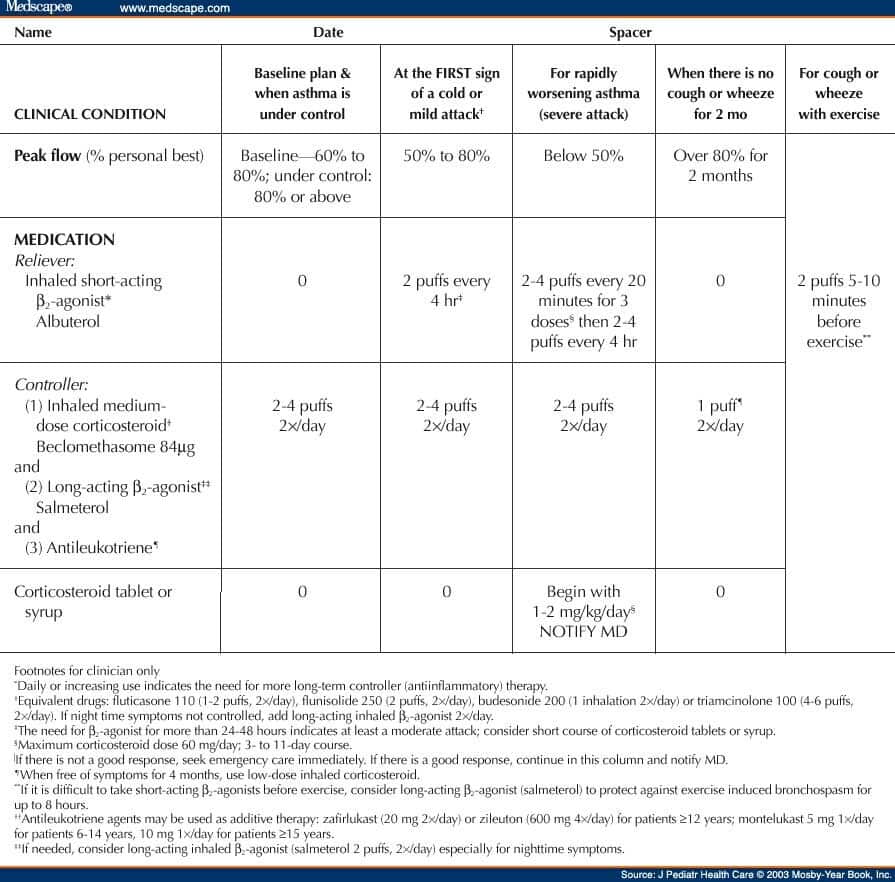
Postdischarge Therapy And Importance Of An Action Plan
Before discharge from the hospital or the emergency department, arrangements for follow-up within 12 weeks should be made for patients. Patients who are hospitalized for their asthma may be especially receptive to information and advice about how to control symptoms and avoid future exacerbations. Health-care providers or an asthma educator should provide detailed education to all patients before discharge. Discussion should assure that the patient understands the cause of his or her exacerbation, modifiable risks factors , the purpose and correct use of medications, and an updated asthma action plan. The action plan should identify each discharge medication, the dose, and frequency. It should also outline how often to take the quick reliever medications if symptoms increase or PEF/FEV1 decreases, when to consider taking oral corticosteroids, and how to reach their primary care provider or obtain emergency care if their asthma does not respond to a step-up in therapy. Patients > 5 y of age usually are discharged with a flow meter, with instructions to keep track of their values until they are seen in follow-up. This is especially important for patients with brittle asthma or for patients identified at risk for near-fatal exacerbations of asthma. Patients should demonstrate the proper use of their inhalers and be discharged with a sufficient quantity of medication to last for at least 12 months.
Adherence To Ics/laba Combination Therapy
Use of combination ICS/LABA therapy may help with patient nonadherence. Administration of the ICS/LABA combination in a single inhaler simplifies the treatment regimen and improves patient adherence, as shown by analyses of medical and pharmacy claims from a large managed care organization and Medicaid patients.46,47 In both analyses, patient adherence was significantly greater with fluticasone/salmeterol administered in a single inhaler than with the individual drug components administered separately. In 1 analysis, short-acting 2-agonist use was significantly lower when combination fluticasone/salmeterol therapy was administered in a single inhaler than when administered separately 47 however, this finding was not seen in a study by Stempel and colleagues.46 Retrospective analysis of matched cohort data from a Canadian provincial healthcare and public drug insurance plan database revealed that combination ICS/LABA therapy was associated with significantly greater persistence, better treatment adherence, fewer asthma exacerbations, and lower use of SABAs than concurrent inhaler therapy.8 These studies are retrospective and based on pharmacy claims data and not direct measures of adherence.
Read Also: How To Strengthen Lungs With Asthma
Talk With Others Who Understand
MyAsthmaTeam is the social network for people with asthma and their loved ones. On MyAsthmaTeam, more than 7,000 members come together to ask questions, give advice, and share their stories with others who understand life with asthma.
Are you a parent or caregiver for a child with asthma? Share your experience in the comments below, or start a conversation by posting on your Activities page.
Changes In The 2019 Guidelines
The 2019 guidelines include five notable changes with regard to asthma treatment in adults. The first change is the switch from SABA-only treatment to ICS-containing treatment for as-needed treatment of symptoms in mild asthma.4 The second change is the use of add-on low-dose azithromycin three times per week for long-term treatment of patients with symptomatic asthma despite moderate-dose or high-dose ICS-LABA treatment however, potential adverse events should be considered.17
The third change is the recommendation for dupilumab, an antiinterleukin-4 receptor alpha monoclonal antibody, as an additional treatment option for patients aged 12 years and older with severe type 2 asthma or OCS-dependent asthma.19 A trial by Wenzel and colleagues demonstrated that dupilumab increased lung function and reduced severe exacerbations in patients with uncontrolled persistent asthma.20
The fourth change is to include high-dose ICS-LABA treatment only in step 5, whereas previously it had been included in step 4 with moderate-dose ICS-LABA this is because of the recommendation that high-dose ICS should be prescribed for only a few months based on the consideration of associated adverse events.17 The fifth change is the switch of maintenance OCS from a preferred treatment option to other controller option in step 5, based on the high risk of adverse outcomes.19
Also Check: Does Asthma Make You Feel Tired
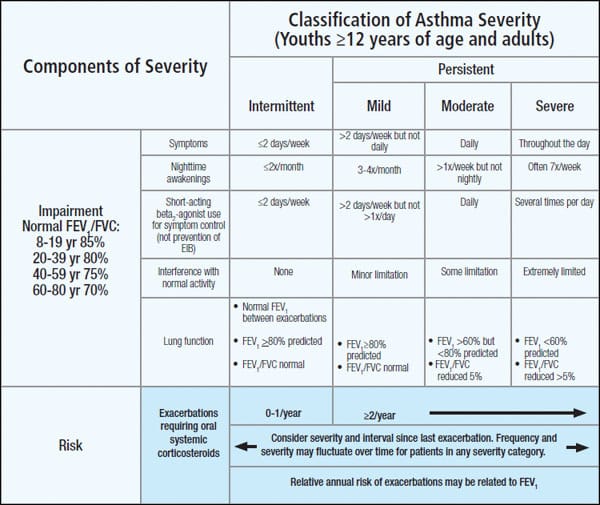
What Are The Differences Between Mild
Patients who have mild-to-moderate asthma can generally control their disease with commonly prescribed medications. But patients with more severe illness, who are on high doses of medications including oral corticosteroids, still may find themselves visiting hospital emergency rooms because of an asthma attack and unable to control their disease. They may find that they have to typically adjust their daily lives, be it missing work, missing school, or not participating in physical activities. The asthma attacks experienced by patients with Severe Asthma may even result in death.
Patients with Severe Asthma are more reliant on their asthma medications. A cross-Canada survey conducted by Asthma Canada looking at the impact of Severe Asthma found that the majority of respondents said they use their controller medication once a day, and about seven out of every 10 said they use it at least twice a day. A significant portion of respondents with Severe Asthma said they use their reliever medication once a day, and 28.8% said they use it at least twice daily.
One of the other differences between mild-to-moderate asthma and Severe Asthma is that patients with severe disease are more likely to have co-morbidities or co-existing medical conditions. These include obesity, obstructive sleep apnea, and gastroesophageal reflux disease .
How Can I Manage My Persistent Asthma
- Follow your asthma action plan. This is a written plan that you and your doctor create. It explains which medicine you need and when to change doses if necessary. It also explains how you can monitor symptoms and use a peak flow meter. The meter measures how well air moves out of your lungs.
- Identify and avoid triggers. Keep your home free of pets, dust mites, cockroaches, and mold.
- Manage other health conditions , such as allergies, sinus problems, sleep apnea, or acid reflux.
- Do not smoke, and avoid others who smoke. Nicotine and other chemicals in cigarettes and cigars can cause lung damage. Ask your doctor for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your doctor before you use these products.
- Ask about the flu vaccine. The flu can make your asthma worse. You may need a yearly flu shot.
You May Like: How To Treat Cough Variant Asthma
Japanese Society Of Allergology
Guidelines for adult asthma were published in October 2020 by the Japanese Society of Allergology .
Diagnosis
The JSA recommends spirometry for assessing the extent of airflow limitation or airway reversibility.
The JSA recommends daily measurement of peak expiratory flow for unstable asthma and patients lacking obvious dyspnea during attack.
Although useful for diagnosing asthma, the JSA does not recommend assessing bronchial hyperresponsiveness in patients with low FEV1 or low %FEV1 since excess airway narrowing may occur due to irritant inhalation.
Treatment of long-term adult asthma
The JSA recommends using a jet nebulizer for budesonide inhalation suspension.
The JSA recommends adding one or more agents other than inhaled corticosteroids , as opposed to increasing the dose of an ICS, to control asthma.
The JSA recommends long-acting 2-agonists , leukotriene receptor antagonists , sustained-release theophylline, and long-acting muscarinic antagonists as add-on drugs.
The JSA recommends that anti-immunoglobulin E antibodies and other biologics as well as oral steroids be reserved for very severe and persistent asthma related to allergic reactions.
The JSA recommends inhaled 2-agonists, aminophylline, corticosteroids, adrenaline, oxygen therapy, and other approaches be used as needed during acute exacerbations.
Treatment during pregnancy
The JSA recommends ICSs as first-line treatment for long-term management of pregnant women with asthma.
Definition Epidemiology And Background
Asthma is a common, chronic inflammatory disorder of the airways characterized by paroxysmal or persistent symptoms and is associated with airflow limitation and airway hyper-responsiveness . Canadian experts have proposed that asthma can be diagnosed in children as early as 1 year of age, if presenting with frequent asthma-like symptoms or recurrent exacerbations reversible with salbutamol with no other alternative diagnosis . Asthma is the most common chronic disease in young people. The general prevalence of asthma in Canada has been estimated at 10%, but is higher in children and youth, including their Indigenous peers -. Asthma exacerbations are a frequent cause of emergency department visits and hospitalizations in children , and asthma is the leading cause of absenteeism from school . Preschool age children with asthma represent more than 50% of consultations in the ED . In one Alberta study, nearly 10% of paediatric ED visits resulted in admission, with one death for every 25,000 ED visits .
Many health care centres, along with national and international associations, have developed practice guidelines for the assessment and management of acute asthma exacerbations -. This statement specifically addresses the management of acute asthma exacerbations in paediatric patients with a known diagnosis of asthma, including preschoolers whose pattern of symptoms suggests likelihood for asthma or suspected asthma .
You May Like: Can Urgent Care Treat Asthma Attack
A Personalized Treatment Plan May Include:
Macrolide antibiotics are used to help the body fight infection. These medicines control the number of white blood cells found in your airways. One study showed positive results using macrolide antibiotics in people with high counts of neutrophils in blood or sputum samples. Doctors dont suggest these medications be used long term though because side effects, such as antibiotic resistance, can be very serious.
Oral corticosteroids are medicines that help to control inflammation. While experts recommend these medicines only for short-term use, doctors may prescribe them long-term for people with more frequent asthma flare-ups. Severe asthma patients use these medications in combination with quick-relief medicine, high-dose inhaled corticosteroids and long-acting bronchodilators. Side effects from using oral corticosteroids can pose a risk to the function of other bodily organs, but the benefits may at times outweigh the risk. The hope is that by using these powerful drugs for a short period of time, patients can gain better control and will eventually not need them at all. This treatment option is approved for adults and children, although long-term use in children is not recommended due to the higher risk side effects. If symptoms are still not controlled with long-term use of an oral corticosteroid, another treatment option should be considered.
|
Type of severe asthma |
How Common Is Severe Asthma
It is estimated that as many as 250,000 Canadians suffer from Severe Asthma. Fatalities are higher in this group compared to patients with mild-to-moderate disease. Each year, about 250 Canadians die from asthma. Globally, 250,000 patients with asthma die prematurely on an annual basis because of their condition.
You May Like: Can You Be In The Military With Asthma
How Is Severe Asthma Diagnosed
More steps are taken to arrive at a diagnosis of Severe Asthma compared to mild-to-moderate asthma. As in mild-to-moderate asthma, healthcare providers will take a detailed medical history, listen for wheezing on examination of the chest, and assess for underlying allergic and non-allergic triggers. Underlying diseases such as eczema or allergic rhinitis may be clues that allergy is present. Allergy skin testing may be performed to evaluate if specific allergic triggers are present that can result in asthma attacks.
In addition, healthcare professionals will likely also conduct objective examinations of lung function including spirometry, or peak expiratory flow , and in some cases, sputum cell counts, which indicate the presence, type, and extent of inflammation in the airways. These objective tests in addition to history will help determine if a patient has Severe Asthma, and will inform treatment choices for patients.
Healthcare providers should refer patients with Severe Asthma to a specialist to confirm their diagnosis and assist in management.
How Is It Diagnosed
To diagnose asthma, a doctor will ask about peoples family history and medical conditions to understand the symptoms and what causes them.
This diagnosis stage also includes questions about peoples lifestyle, such as whether they usually smoke or exercise, their environmental conditions, and the presence of other medical conditions, such as hives and eczema.
If a doctor suspects asthma, they will perform a physical exam and order tests. These screenings may include lung function tests such as spirometry and a peak flow test.
The doctor may also request a chest X-ray, a blood test, or other tests to confirm their diagnosis and rule out other conditions.
Read Also: Is Broccoli Good For Asthma
Figure : Stepwise Approach To Asthma Management For Children Ages 0
ICS=inhaled corticosteroids, LABA=long-acting beta agonists, SABA=short-acting beta agonistsAdditional Figure 3 notes
- Every step: Reduce exposure to triggers, exercise, eat healthy, and manage stress
- Steps 2, 3, and 4: Consider immunotherapy for allergies
- Steps 5 and 6: Consider adding asthma biologics
Comparative Safety And Efficacy Of Fixed
The safety and efficacy of fixed doses of budesonide/formoterol and fluticasone/salmeterol have been directly compared in several large, randomized, controlled trials,3539 which formed the basis of a recently published Cochrane meta-analysis.40 Drawing on 5 randomized studies including data from 5537 adolescent and adult patients with asthma , the meta-analysis found that budesonide/formoterol and fluticasone/salmeterol were equally effective and well tolerated, with no significant differences between treatments on primary efficacy outcomes or secondary efficacy outcomes .40
Don’t Miss: How Can We Prevent Asthma
Types Of Asthma And Biomarkers
Types of asthma and biomarkers
In adults, two common types of asthma are distinguished: allergic asthma, where there is a clear relationship to allergy, and intrinsic or eosinophilic asthma, which usually starts in adulthood without evidence of any relevant allergies.
In adults, two common types of asthma are distinguished. The first is allergic asthma, where there is a clear relationship with allergy. Onset is often during childhood or adolescence and often accompanied by allergic rhinitis and/or atopic dermatitis this form is known as early-onset asthma. The second is an intrinsic type, usually with onset in adulthood and usually without evidence of any relevant allergies this form is referred to as adult-onset or late-onset asthma) . In both types of asthma, an increased level of typical cytokines and eosinophil granulocytes is found, together with dysfunction of structural cells characteristics referred to collectively under the name type 2 asthma . The inflammation can be measured through biomarkers . Routine diagnostic procedures covered by statutory health insurance carriers in Germany include blood eosinophil count and allergy markers fractional exhaled NO measurement is available as a self-pay option. It should be noted that these biomarkers can be falsified: for example, eosinophil counts can be greatly reduced by inhaled or oral steroids and FeNO levels by tobacco smoke .
What Are The Economic And Social Burdens In Canada Related To Severe Asthma
Severe Asthma takes a serious toll on patients and on Canadas healthcare system. Patients with Severe Asthma will often need more medical care and will be visiting hospital emergency rooms, and visiting their family doctors and specialists. In 2015, asthma attacks led to more than 70,000 visits to emergency rooms in Canada. The cost of asthma to the Canadian economy is expected to climb to $4.2 billion by 2030.
According to one study, children with Severe Asthma were more likely to miss seven days or more of school than children with mild or moderate disease .
In terms of a social burden, Severe Asthma as a chronic condition impairs an individuals ability not only to breathe but to work and live a happy and healthy life. With increased disease severity, a patients quality of life becomes progressively worse. Sadly, depression is a co-morbidity that occurs with Severe Asthma.
Recommended Reading: What Is The Difference Between Asthma And Bronchial Asthma
