What Is Eosinophilic Esophagitis
Besides being a difficult name to pronounce, eosinophilic esophagitis is a disease that was only first recognized as a distinct clinical problem in 1993. Also sometimes referred to as allergic oesophagitis, the condition is characterized by allergy-related inflammation of the epithelial lining of the esophagus. Eosinophilic esophagitis is still fairly rare, but incidences of diagnosis have been increased slightly in recent years as more doctors are becoming aware of it it is estimated that it afflicts 1-4 people in 10,000.
At a basic level, the inflammation central to eosinophilic esophagitis is a reaction to an allergen the current prevailing thought is that food allergies are the primary trigger. The difference between eosinophilic esophagitis and other types of inflammation is a type of white blood cell called eosinophil that is not typically found in the esophagus. In patients with eosinophilic esophagitis, large numbers of eosinophils are sent to the esophagus by the immune system and cause inflammation as a part of their regular immune response.
Although it is located in the esophagus and can have a significant impact on the digestive system, eosinophilic esophagitis is classified as an autoimmune disorder, a type of condition where the immune system inadvertently attacks the body itself. It is considered a chronic condition and is not curable in a conventional sense, but there are treatments that can encourage it to become inactive.
How Is Eosinophilic Granulomatosis With Polyangiitis Diagnosed
The healthcare provider may use the following tests to diagnose EGPA:
- Medical history: to look for EGPA, especially asthma, allergies and other features of the disease.
- Physical examination: to discover which organs are involved and to rule out other illnesses that may look similar.
- Blood tests: to look for abnormal blood counts and an increase in eosinophils and special antibody testing called ANCA.
- Urinalysis: to detect whether there is too much protein, or red blood cells, in the urine.
- Imaging tests such as x-rays and computed tomography to look for any abnormalities in areas such as the lungs or sinuses.
Once the diagnosis of EGPA is suspected, a biopsy is often performed to try to find eosinophils, eosinophilic granulomas and/or vasculitis. Biopsies are not required in all cases, and are only recommended when abnormal findings are seen in the exam, laboratory tests, or imaging tests.
Eosinophilic Granulomatosis With Polyangiitis
Eosinophilic granulomatosis with polyangiitis was first described by Churg and Strauss in 1951 . The disease progresses through three overlapping phases: adult-onset asthma, peripheral and tissue eosinophilia, and necrotizing vasculitis with tissue infiltration of eosinophils . EGPA is an idiopathic type of small vessel vasculitis and is also part of the hypereosinophilic syndromes . It is associated with HLA and IL-10 polymorphisms . About 40% of EGPA patients have perinuclear ANCA antibodies against myeloperoxidase , resulting in the classification of EGPA as an ANCA-associated vasculitis . The presence or absence of ANCA in EGPA may indicate two clinical subtypes with different organ involvement. ANCA-positive patients have more frequent vasculitis and glomerulonephritis, whereas ANCA-negative patients have more frequent heart and lung involvement .
Blood eosinophils in EGPA show an activated phenotype expressing high levels of CD69 and CD11b . Moreover, they express IL-25, a cytokine that increases release of IL-4, -5, and -13 from T cells. Serum IL-25 is increased in patients with active EGPA compared to inactive disease or healthy controls. It is also detectable in eosinophils from lesional biopsies. T cells in these biopsies and in the blood express the IL-25 receptor IL-17RB . This suggests a feed-forward loop between eosinophils and Th2 cells in EGPA.
You May Like: Can You Join The Army If You Have Asthma
Cell Culture And Cell Induction Conditions
Immortalized human keratinocyte HaCaT cells and BEAS-2B cells were cultured in DMEM medium containing 10% fetal bovine serum , 100 U/ml penicillin, and 100 g/ml streptomycin , at 37°C with 5% CO2 and 95% humidity. The experimental cells were divided into the control group , Solarbio), IL-4 25 ng/ml, 50 ng/ml, 100 ng/ml induction group and the induction duration was 12h, 24 h and 48h, respectively . In the stimulation experiments, cells were cultured in serum-free medium.
What Are Egpa Symptoms
Because EGPA can affect several different organs, there is a wide range of symptoms.
People who have EGPA may feel generally ill and fatigued or have fevers. They may lose their appetite and lose weight. Other symptoms depend on the organs or diseases involved. For example, you may have:
- Shortness of breath from asthma or inflammation in the air sacs and blood vessels of the lungs.
- Chest pain from disease that affects the lungs or heart.
- Rashes on the skin.
- Abdominal pain or blood in the stools from intestinal tract involvement.
- Abnormal feelings, and numbness or loss of strength and feeling from nerve involvement.
You may have any combination of these symptoms.
Kidney disease caused by EGPA often does not have any symptoms. You may not know about inflammation of the kidney until the kidneys begin to stop working. Therefore, if you have any form of vasculitis, you must have regular urinalyses .
Don’t Miss: Airway Inflammation In Asthma
Eosinophilic Esophagitis: Symptoms And Causes
Modern medicine is a train that keeps rolling along, and this means that new discoveries are made every day and new understandings are around every corner. This can be good news for many people because it means that diseases that once had a dire prognosis are now curable or able to be successfully mitigated. Still, as amazing as modern medicine is, there are still new conditions that emerge and pose new challenges for doctors. One example of a recently identified disease that is still not very well understood is eosinophilic esophagitis.
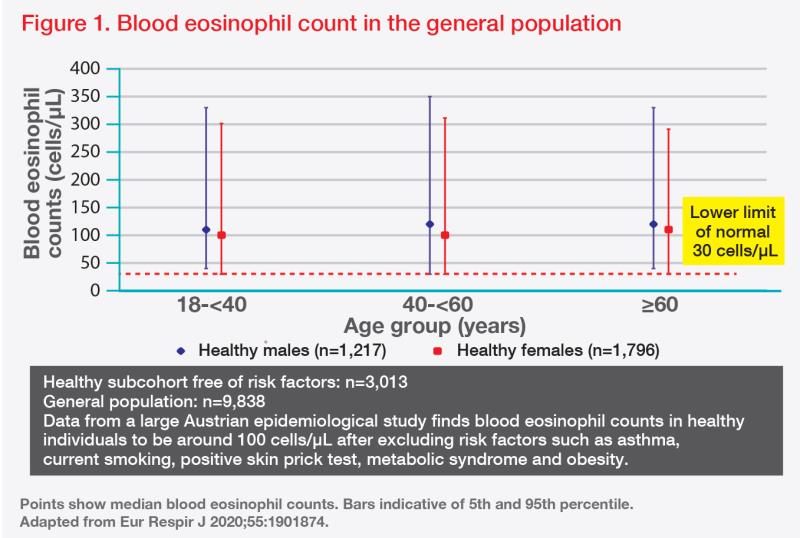
Perspective From Eosinophil Biology
Eosinophils are short-lived, bone marrowâderived granulocytes. Eosinophil differentiation is largely dependent on IL-5, which is produced by Th2 cells and group 2 innate lymphoid cells . Although type 1, 2 and 3 inflammation may overlap and balancing real life , type 2 inflammation is closely associated with eosinophilic inflammation. In response to type 2 cytokines, terminally differentiated eosinophils are mobilized from a niche in the bone marrow into the blood circulation. In a normal homeostatic condition, the half-life of blood eosinophils is approximately 25 hours, and the majority of senescent eosinophils are cleared in the liver and spleen, where they are taken up by macrophages of the reticuloendothelial system. Apoptotic eosinophil clearance by phagocytotic cells mediates the resolution of inflammation and is shown to be dependent on the receptor tyrosine kinase Mer. Although the life span of eosinophils within the tissue is unknown, it is estimated to be < 1 week in homeostatic conditions. Tissue presence of eosinophils is determined based on recruitment, retention and clearance . Eosinophil express various surface receptors and stored presynthesized specific granule proteins and mediators in their crystalloid granules, indicating that they can regulate immune system within minutes of stimulus-induced cell activation .
FIGURE 2
Recommended Reading: Can A Humidifier Help With Asthma
Classic Symptoms And Signs Of Egpa
Asthma is one of the cardinal features of EGPA. Asthma symptoms may begin long before the onset of vasculitis e.g., many years before any other symptoms of EGPA arise, and long before the diagnosis of EGPA is made. Other early symptoms/signs include nasal polyps and allergic rhinitis.
The next phase of the disease is often marked by eosinophilia, the finding of an excessive number of eosinophils in the blood or in tissues. An eosinophil is one subtypes of white blood cell. Normally, eosinophils comprise 5% or less of the total white blood cell count. In EGPA, the percentage of eosinophils may reach as high as 60%. In the picture below, the eosinophils are shown by the dark pink stain.
The third phase of the illness is a vasculitis, which involves the skin, lungs, nerves, kidneys, and other organs. Particular mention should be made of the frequent devastating involvement of the nerves , which produces severe tingling, numbess, shooting pains, and severe muscle wasting/power loss in the hands or feet. The list below contains the organs commonly involved by EGPA and the specific disease manifestation in each organ.
- Lesions are occasionally found in the GI tract
- Granuloma sometimes found in spleen
Preparing For A Doctors Appointment
Patients with asthma or suspected asthma will likely be referred to an allergist or a pulmonologist. These tips may help you be more prepared for your appointment:
- Keep a log of symptoms you are having, even if they are seemingly unrelated.
- Bring a list of any prescription or over-the-counter medications you are taking. Dont forget to list vitamins and supplements, too.
- Jot down a list of questions, such as:
- What tests or procedures will be performed?
- How will my asthma be monitored?
- How should I use my medications? How should they be stored?
- What triggers might cause my asthma to flare? Is there anything I can/should do to reduce my risk of having an asthma attack?
- Will I have an asthma action plan?
- How often do I need follow-up care?
You May Like: How To Smoke Weed With Asthma
What Are The Types Of Asthma
Various types of asthma are described below:
- Allergic asthma: Allergens trigger this type of asthma. Allergens include pet dander, food, dust, pollen, and mold. Allergic asthma is often seasonal.
- Nonallergic asthma: Mainly, air pollutants trigger this type of asthma. Irritants include cold air, the smoke of air pollution, viral illness, cigarette smoke, air fresheners, cleaning products, perfumes, and burning of wood.
- Occupational asthma: Occupational asthma is triggered in the workplace. These include dust, gases, fumes, certain chemicals, animal proteins, and dyes.
- Exercise-induced bronchoconstriction : EIB usually occurs within a few minutes of starting exercise or physical activity. Most asthmatics will experience EIB however, not everyone with EIB will have other types of asthma.
- Eosinophilic asthma: Eosinophilic asthma is often associated with high eosinophils . People with eosinophilic asthma do not have any allergies. A specific cause has not been identified for eosinophilic asthma.
Tslp/il3: Possible Common Genetic Factor For Adult
TSLP is an essential epithelial cell-derived cytokine induced by allergens, pollutants, bacteria and viruses. A recent study showed that double-stranded RNA-stimulated lung endothelial cells produce both IL-33 and TSLP higher than those of bronchial epithelial cells. In the GWAS on NP and CRS, the top signal at the TSLP locus was rs1837253, which is also associated with ANCA-negative EGPA at genome-wide significant levels. Rs1837253 is located immediately upstream of TSLP, and the frequencies of rs1837253 greatly differ across various ethnic populations . GWASs, including meta-analyses, have also identified associations of rs1837253 and asthma in various ethnic groups, asthma-related phenotypes and eosinophilia.- A recent study reported a significant association of the rs1837253 genotype with CRSwNP and N-ERD, and demonstrated a positive correlation between the risk allele and the number of eosinophils in mucosal tissues of patients with CRSwNP in the Japanese population.
Also Check: How Can U Get Asthma
Can I Live A Normal Life With Egpa
EGPA shouldnt stop you from your normal, day-to-day activities, as long as you seek and receive treatment from your healthcare provider.
A note from Cleveland Clinic
EGPA is a serious illness that can affect a variety of organs but, fortunately, more than 80% survive the symptoms . Stay in close contact with your healthcare provider and be sure to follow his or her instructions regarding your care.
What Is The Outlook For Eosinophilia
Treating the cause of high eosinophil counts affects the outcome. In more serious conditions, outcomes also depend on the extent of target organ and how the person responds to treatment.
Last reviewed by a Cleveland Clinic medical professional on 02/15/2018.
References
- Fulkerson PC, Rothenberg ME. Targeting Eosinophils in Allergy, Inflammation and Beyond. Nature reviews Drug discovery. 2013 12:10.1038/nrd3838. doi:10.1038/nrd3838.
- Common Laboratory Tests. In: LeBlond RF, Brown DD, Suneja M, Szot JF. LeBlond R.F., Brown D.D., Suneja M, Szot J.F. Eds. Richard F. LeBlond, et al.eds. DeGowinâs Diagnostic Examination, 10e New York, NY: McGraw-Hill 2014.
- Merck Manual Professional Version. Accessed 3/2/2018.Eosinophilia.
- American Partnership for Eosinophilic Disorders. Accessed 3/2/2018.What is an eosinophil-associated disease?
- Hsieh, Fred H Eosinophilia and the Hypereosinophilic Syndrome. In: _eLS. John Wiley & Sons, Ltd: _Chichester. doi: 10.1002/9780470015902.a0002155.pub2
- Kovalszki A, Weller PF. Eosinophilia. Primary care. 2016 43:607-617. doi:10.1016/j.pop.2016.07.010.
- Rothenberg ME. Eosinophilia. N Engl J Med. 1998 338:1592-600.
- Butt, N. M., Lambert, J., Ali, S., Beer, P. A., Cross, N. C. P., Duncombe, A., Ewing, J., Harrison, C. N., Knapper, S., McLornan, D., Mead, A. J., Radia, D., Bain, B. J. and the British Committee for Standards in Haematology , Guideline for the investigation and management of eosinophilia. Br J Haematol, 176: 553â572. doi:10.1111/bjh.14488
Recommended Reading: What’s An Asthma Attack Feel Like
Is Eosinophilic Asthma An Autoimmune Disease
Eosinophilic asthma is also one type of asthma in which a persons eosinophils levels are higher than average .
Individuals with autoimmune disorders may also have high eosinophils. However, eosinophilic asthma is not an autoimmune disease. As with all types of asthma, eosinophilic asthma is an inflammatory condition.
What Is Eosinophilic Asthma
Eosinophilic asthma is a subtype of asthma that is often severe. It is commonly seen in people who develop asthma in adulthood, although it may occur in children and young adults.
Asthma is a chronic lung disease in which diseased airways are infiltrated by inflammatory cells and obstructed by fluid and mucous. This causes spasms in the bronchial tubes, making breathing difficult. Asthma may result from allergy or other hypersensitivities however, many patients who have eosinophilic asthma do not have a history of allergic conditions .
In eosinophilic asthma, the numbers of eosinophils are increased in blood, lung tissue, and mucus coughed up from the respiratory tract . The whole respiratory tract is involved in airflow obstruction from the sinuses to the small or distal airways. Patients with eosinophilic asthma frequently suffer from chronic sinus disease and nasal polyposis.
Research has shown that an elevated number of eosinophils in the blood correlates with future risk and severity of asthma attacks.
Asthma can range in severity and treatment may vary from patient to patient. To help outline the best course of treatment for an asthmatic patient, it is important for a health care provider to determine which subtype of asthma a person might have, because there are now new therapies that target specific subgroups of asthma, like eosinophilic asthma.
Also Check: Does Weight Gain Make Asthma Worse
Genetic Background Of Adult
Recent genome-wide association studies of adult-onset asthma, EGPA, CRSwNP, have convincingly identified a number of susceptibility loci .- The reported or mapped genes, which were associated with these asthma-related phenotypes in at least 2 GWASs, are listed in Table .
| Locus |
|---|
- The reported or mapped genes of GWASs of adult-onset asthma were obtained from GWAS Catalog .
- Shaded boxes are the genetic loci associated with the specific disease.
- aThese reported genes are located within 500 kb.
- bRepresentative genes are shown at the HLA locus.
Bioinformatics Analysis Of The Biological Function Of Flg Exon Snps
Since FLG rs75235053 C> G and rs192116923 T> G were associated with severe EA and EA patients with AD, respectively, their biological functions were tested by bioinformatics. FLG encodes the filaggrin precursor protein profilaggrin, which contains 4061 amino acids. Its protein code is mainly in the third exon region, and mutations are also mainly distributed in this region. Rs192116923 T > G is a missense mutation p. Glu 2652 Asp, while rs75235053 C > G is a missense mutation p. Ser 3662 Thr, and both of them are anticipated by Polyphen 2, SIFT score, Mutation Taster, and CADD as non-harmful mutations. HaploReg v4.1 predicts that rs192116923-T mutation to -G can modify its binding motif to Smad3, and SNP2TFBS predicts that it can bind to Smad2_Smad3_Smad4, whereas PROMO suggests that rs75235053-C mutation to -G may reduce the binding to c-Jun.
Also Check: How To Help Your Asthma Without An Inhaler
Treatments For Eosinophilic Esophagitis
As a chronic condition, eosinophilic esophagitis cannot be strictly cured. There are, however, a number of treatment methods doctors can employ to mitigate the symptoms or even make the diseases essentially inactive:
- Diet Therapy: Since food allergies appear to be one of the primary triggers of the initial inflammation, a dietary approach is typically the first step. However, since people are different and have different allergies, a doctor will order a series of allergy tests to determine which foods are actually the problem. A restricted diet that avoids these foods can sometimes more or less eliminate or substantially reduce the inflammation.
- Medication: Proton pump inhibitors are often prescribed initially though they have an unreliable record at treating eosinophilic esophagitis, the lack of responsiveness to PPI can actually help confirm the diagnosis. Another medication that may be used is a topical steroid like fluticasone or budesonide, a liquid that when swallowed can coat the inner lining of the esophagus and reduce inflammation.
- Dilation: In some cases of eosinophilic esophagitis where there is a narrowing of the esophagus, the doctor may use endoscopy to mechanically stretch out the esophagus. While it doesnt address the inflammation, dilation can make the passage of food bolus more smooth.
Diagnosis Of Eosinophilic Esophagitis
The similarity to GERD in terms of symptoms makes the diagnosis of eosinophilic esophagitis somewhat dependent on first ruling out GERD. In order to confirm eosinophilic esophagitis, though, the doctor will typically utilize several tests:
- Upper Endoscopy: An endoscope is a long, flexible tube with a camera on one end that is used to examine, among other parts of the body, the gastrointestinal tract. The doctor will insert the endoscope in the patients mouth and inspect the esophageal lining. Telltale signs of eosinophilic esophagitis include inflammation, swelling, strictures , white spots, or horizontal rings.
- Biopsy: While performing an endoscopy, the doctor may also take a biopsy, a small cutting of tissue that can then be analyzed. The presence of eosinophils typically confirms eosinophilic esophagitis.
- Blood Test: A blood test is one of the final procedures that can confirm eosinophilic esophagitis as well as point to the potential allergens that might be causing the problem. Besides eosinophil count, total immunoglobulin E levels can also point to allergy-related eosinophilic esophagitis.
Don’t Miss: I Have Asthma And I Smoke Weed
