Breathing: Normal Airways Vs Asthma Airways
Normal: In someone with optimal lung function, air is inhaled through the nose and mouth, passing through the trachea before moving into the bronchi . The bronchi branch into smaller tubes, ending in many small sacs called alveoli. Its in the alveoli that oxygen is passed to the blood and carbon dioxide is removed.
Asthma: In someone with asthma, the airways are inflamed, and when triggered, can constrict even more, obstructing airflow to the lungs.
Candidate Genes And Snps
shows the list of common candidate genes in asthma with their locations derived from a large number of single nucleotide polymorphisms studies. The following are some of the extensively studied candidate genes and SNPs associated with asthma, with special reference to studies in the Indian population:
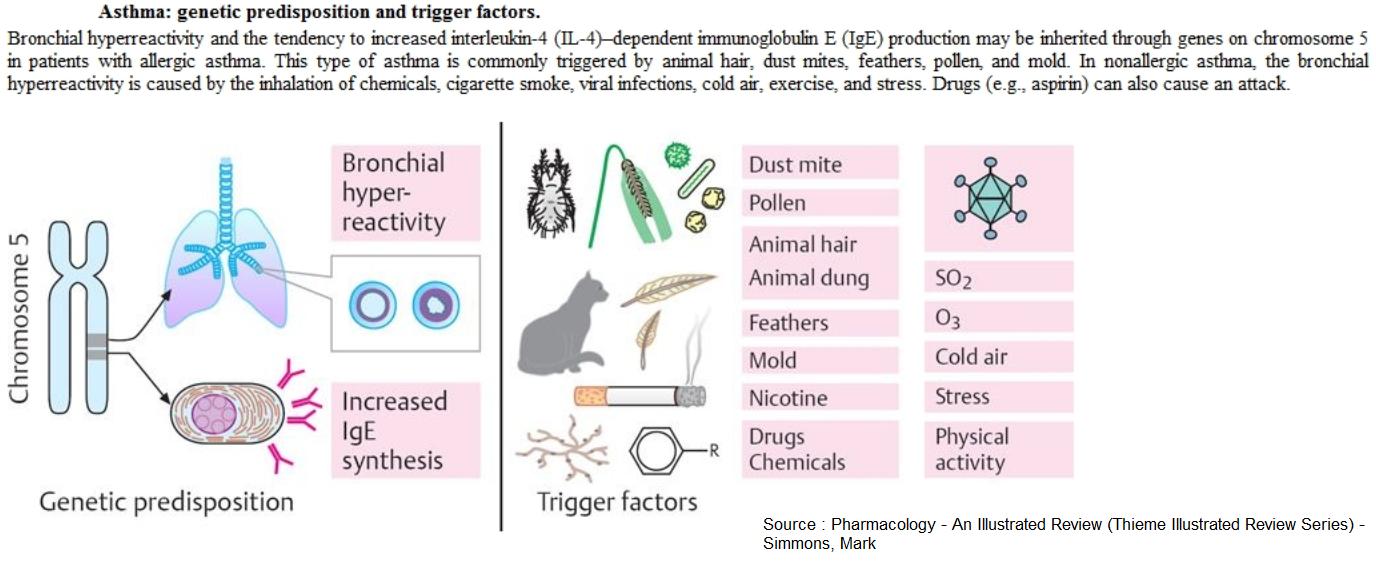
2. Interleukin-4 : This is located on chromosome 5 at position q31 with 32675 bps, 10 exons and 9 introns. IL-4 is a cytokine secreted by helper T cell type 2 that stimulates the production of IgE and induces eosinophil-mediated attacks against allergens. Chiang et al established that polymorphism in the promoter of the IL-4 is associated with asthma and is a disease modifier in terms of the severity of airway hyper-responsiveness . A total of 16 polymorphisms were identified in the IL4, of which one in the promoter and other on the 5 untranslated region of the IL4 have been identified that influence total serum IgE levels and bronchial hyper-responsiveness. Nagarkati et al indicated that the promoter of the IL4 gene is invariant in Indian population and Bijanzadeh et al reported that there are no significant association between this SNP of the IL-4 and asthma in an Indian population.
6. G-protein-coupled receptor for asthma : This is localized on chromosome 7p with 7 SNPs. A hierarchical genotyping design was used to identify this gene. The data implied that this gene is involved in the pathogenesis of atopy and asthma and may have application in other inflammatory diseases.
What Are The Symptoms
Asthma can be different for everyone. Asthma symptoms can also vary over time, with few or no symptoms when asthma is well controlled. The common signs and symptoms of poorly controlled asthma include:
- Shortness of breath
- Trouble sleeping because of breathing difficulty
- Being unable to take part in physical activities without breathing difficulty
These symptoms can occur slowly over hours or days, or they can come on as sudden, recurring attacks after which the symptoms can persist for some time before disappearing. If left untreated, asthma can cause permanent structural changes in your airways called airway remodelling, which is why it is important to get your asthma under control and keep treating it over the long term.
Don’t Miss: What Happens If You Smoke Weed With Asthma
Asthma And Allergies Tend To Run In Families
If theres asthma, eczema, hay fever or other allergies in your family it makes asthma more likely.
If you have asthma yourself, your child is much more likely to have asthma too, particularly if both parents have asthma. Theres slightly more chance of asthma being passed on by the mother than the father.
Environmental Factors And Asthma
Indoor air pollution such as cigarette smoke, mold, and noxious fumes from household cleaners and paints can cause allergic reactions and asthma. Environmental factors such as pollution, sulfur dioxide, nitrogen oxide, ozone, cold temperatures, and high humidity are all known to trigger asthma in susceptible individuals. In fact, asthma symptoms and hospital admissions are greatly increased during periods of heavy air pollution. Ozone is the major destructive ingredient in smog. It causes coughing, shortness of breath, and even chest pain — and can boost the susceptibility to infection. Sulfur dioxide, another component of smog, also irritates the airways and constricts the air passages, resulting in asthma attacks.
Gas stoves are the primary source of indoor nitrogen dioxide, a common indoor pollutant. Studies show that people who cook with gas are more likely to have wheezing, breathlessness, asthma attacks, and hay fever than those who cook with other methods. It is estimated that more than half of the households in the U.S. use gas stoves.
Weather changes can also result in asthma attacks in some people. For instance, cold air causes airway congestion and an increase in mucus production. Increases in humidity may also cause breathing difficulty in a certain population.
You May Like: Difference Between Chronic Asthma And Acute Asthma Exacerbation
Segregation And Linkage Analysis
Segregation analysis can provide insight into the genetics of a trait, e.g. the number of genes involved and the genetic model: dominant or recessive, polygenic, and those with environmental effects. Using this type of analysis, the heritability, mode of inheritance, penetrance and frequency of a trait are being estimated and also indicated the involvement of major genes.
A large study performed by the European Community Respiratory Health Survey Group analyzed the pooled data from 13,963 families using complex seg-regation analysis. The results of this study showed further evidence of genetic regulation of asthma and a model with a two-allele gene with codominant inheritance fitted the data best, assuming a major gene has to be involved in the pathogenesis of asthma, but the penetrance of such a gene is low. Jenkins et al presented a segregation analysis of 7,394 families in which 15.9 per cent of the index individuals had asthma. A segregation analysis of physician-diagnosed asthma in 3,369 randomly selected individuals from 906 nuclear families done by Holberg et al in Tucson, AR, USA, showed evidence of a polygenic or an oligogenic model with some evidence of a recessive gene, explaining only part of the segregation.
Kleeberger and Peden have studied different environmental factors in isolation which have been shown to affect asthma and related phenotypes but their interaction effects have been missed.
Other Omic Studies And Integration Of Multiomics
Other omics technologies, apart from genomics, are powerful tools to increase the current knowledge about asthma pathophysiology . These are focused on data from a wide variety of biological sources: genomic modifications , gene transcription , protein levels and chemical modifications , endogenous and exogenous metabolites , and the microbiome , among others . The application of omics approximations in asthma is still incipient compared to other diseases . Still, several studies have been performed in asthma in the last years as it was reviewed elsewhere .
To our knowledge, a total of 26 asthma studies using other omics approaches have been published in the last 2 years . Just like recent GWAS of asthma, these studies have been equally focused on childhood and adulthood asthma since 2016. Moreover, most of them have been carried out in patients of European descent. A total of 18 studies focused on asthma susceptibility or severity three focused on the ICS response two explored the interactions with environmental factors and three inspected the overlap with other pulmonary diseases . Nonetheless, other experts have discussed the recent omics advances in asthma in this issue except for those of transcriptomics. Therefore, we focused on summarizing the main findings of studies made using this approach.
Recommended Reading: Air Trapping In Asthma
Estimating The Contribution Of The Sentinel Variants To The Heritability Ofasthma Hay Fever And Eczema
Five steps were involved. First, we performed a GWAS of the individualdiseases in the HUNT study, which was not included in the discoverymeta-analysis. The HUNT study is described in greater detail in the .Briefly, based on self-reported questionnaire information, we identified 1,875cases and 16,463 controls for the asthma GWAS 6,939 cases and 12,844 controlsfor the hay fever GWAS and 2,630 cases and 16,131 controls for the eczema GWAS.After quality control filters, we analyzed 7.6 million common variants for association with each individual phenotype. Thegenomic inflation factor for these analyses were 1.049 for asthma,1.078 for hay fever, and 1.041 for eczema. Second, for each of the threediseases, we quantified the overall SNP-based heritabilities with LD scoreregression using a subset of 1.2 millionHapMap SNPs. To obtain a heritability estimate on the liability scale, we setthe population prevalence to be the same as the sample prevalence, given thatthis was a population-based study. Third, we removed the 136 sentinel variants fromthe individual disease GWAS results. Fourth, we re-estimated SNP-basedheritabilities as described for step two, but now using the GWAS results withoutthe 136 top associations. In the fifth and final step, the contribution of the136 sentinel variants towards the heritability of each disease was calculated asthe difference between the SNP-based heritability estimated in steps two and four .
Common Traits And Diseases Associated With Allergic Disease Riskvariants
We first identified all variants in LD with a sentinel risk variant usingdata from Europeans of the 1000 Genomes Project , and extracted anyassociations with these reported in the NHGRI-EBI GWAS catalog database or byAstle et al. , a large GWAS of bloodcell counts . To complement this analysis, weestimated the SNP-based genetic correlation between our GWAS and resultsreported for 229 common traits or diseases, using LD Hub . In these analyses, results from our meta-analysis werenot corrected for the LD score intercept, either at the study level or after themeta-analysis.
Also Check: Asthma Mast Cells
Children With Allergies Can Go On To Develop Asthma
If your child tends to get allergies theyre said to be atopic. Being prone to allergies is usually something that runs in families. And if your child has one allergy theyre more likely to get another one.
For example, children with eczema, and a family history of allergy, are more at risk of developing asthma than other children.
GPs and researchers talk about the atopic march, says Dr Andy Whittamore, Asthma UKs in-house GP. This is when allergies appear in children in a certain order, depending on their age.
Sometimes allergies overlap, and sometimes your child will switch from one allergy to another. A small child with eczema may go on to have a food allergy, and then, as they get older, hay fever, and then asthma.
Unexplored Genetic Variation In Asthma
Exploring non-coding variation has been also proposed as a promising strategy to disentangle the genetic basis of complex diseases such as, microRNAs . These are short, non-coding and single-strand RNA molecules that interact with different genomic elements and regulate gene expression at transcriptional level . Interestingly, these are involved in the regulation of the stability of immune cells and the intensity of inflammation . In fact, miRNAs have been proposed as potential non-invasive asthma biomarkers that could be used for asthma diagnosis . However, although some authors have suggested the implication of miRNAs on asthma susceptibility, severity, and exacerbations , there is a lack of studies that have extensively evaluated their role in asthma and further studies are needed .
As mentioned, the main reason for the scarce evaluation of these types of genetic variation in asthma could be attributed to the fact that research strategies on asthma genetics have focused on using SNP genotyping platforms, which are suboptimal for inferring CNVs, and do not capture rare or pLoF variants , as these would be optimally detected by means of sequencing approaches. Given that simultaneous sequencing of millions of small DNA fragments is currently possible at great speed and relatively low cost thanks to large improvements in next-generation sequencing technologies , the interest on the impact of these types of genetic variation in asthma will continue to rise.
Don’t Miss: What Is Type 1 Asthma
How Does Asthma Work
Asthma is an inflammatory lung disease characterized by shortness of breath, chest tightening, coughing, and wheezing. The symptoms vary from person to person and differ in severityevery person with this disease has individual triggers. Some people may experience an asthma attack once a year, while others deal with them several times a month. One consistency stands outpeople with asthma are at risk of developing more severe symptoms due to smoking or air pollution exposure.
The disease often appears in childhood alongside allergic reactions, although its not unusual for adults to develop it. Several variations of it exist, including occupational, adult-onset, and non-allergic asthma. A viral infection, such as rhinovirus or parainfluenza, usually triggers adult-onset asthma. Scientists have found a link between the presence of airway eosinophilia and the development of viral-induced asthma.
People with eosinophilia have an abnormally high level of eosinophils, or white blood cells, in their bodies. This condition often signals allergic reactions, infections, or any illnesses targeting the immune system.
Drawing Connections Between Disease And Genetics
Asthma affects numerous people, but they can manage it through regular care and medications. The disease doesnt have to ruin ones quality of life or remove the fun from physical activity. By learning more about the condition and how it manifests, scientists can create improved methods to prevent and treat it.
Emily Folk is a sustainability and green tech writer. You can read more of her work on her blog, Conservation Folks, or follow her on.
Read Also: Can Allergies Cause Asthma Attacks
Molecular Genetics Of Asthma
Over a hundred different genes have been associated with asthma and the list is still growing. Asthma susceptibility genes fall mainly into three categories relating to 1) functioning of the immune system, 2) mucosal biology and function, and 3) lung function and disease expression . However, just because a gene has been associated with asthma in a single study does not necessarily establish a connection between that gene and the disease. A major problem in many genetic studies of asthma is the lack of replication of results from previous studies. Notably, only a subset of identified genes has been found to be associated with asthma in more than one study and many regard replication as one of the most important features of a gene’s candidacy . However, some genes may be important only in a subset of asthmatics, for example, in childhood-onset asthma, atopic asthma, house dust mite sensitive asthma, or occupational asthma, and therefore replication across these different populations cannot always be expected. Moreover, some genes are expressed only in certain environmental contexts, for instance, in children growing up with a cat or in those exposed to passive smoking in the first years of life . The importance of gene-environment interaction in asthma causation should not be underestimated every gene’s role should be viewed within the context of a permissive environment.
Family And Twin Studies
Familial aggregation of asthma was probably first described by Sennertus in 1650. Two large studies were performed the inheritance of atopy, one in 1916 and the other in 1924. In the first and second studies 48.4 and 58.4 per cent of family history cases respectively were reported and autosomal dominant inheritance of atopy was suggested. Schwartz reported that the prevalence rates of asthma in the 1,634 relatives of the 161 asthmatic subjects was 6.6 per cent, but, in the 1,790 relatives of the control group, only 1 per cent. Sibbald et al reported that the overall prevalence of asthma in the first degree relatives of asthmatics was 13 per cent and in the relatives of controls only 4 per cent. This indicates that there is a considerable genetic component in the pathogenesis of asthma.
Twin studies have generally shown that concordance rates for asthma are significantly higher in MZ twins than in DZ twins, whether reared apart or together. Broad-sense heritability estimates derived from twin studies range from 36 to 75 per cent. Twin studies have revealed a 0.74 concordance between monozygotic twins and a 0.35 concordance between dizygotic twins, implicating a genetic contribution to asthma development.
Recommended Reading: How To Handle An Asthma Attack Without An Inhaler
Does Asthma Run In The Family
Asthma, a chronic lung condition that affects the airways, can occur in people of all ages. In some cases, asthma symptoms can be mild and are well controlled with asthma medications. For others, symptoms are more severe and can have a debilitating effect on daily life and work. Asthma and other atopic conditions can run in the family, meaning if you have a family history of the condition, you are more at risk to developing it.
Theres no cure for this bronchial condition, but it can be effectively managed with modern treatments, and research continues to reveal more about asthma causes.
Read on to discover if asthma is genetic or environmental and if theres any truth in the idea that asthma can run in families.
Its Difficult To Say For Sure Why People Get Asthma But Thanks To Research Were Clear About Some Of The Risk Factors That Make Asthma More Likely
What causes asthma is different to what triggers asthma:
- The causes are the underlying reasons why someone gets asthma in the first place.
- Triggers are things like dust mites or pollen that can make asthma symptoms worse.
Here we look at what causes asthma, and where its possible for you to lower the risk. The good news is that some of these risk factors are things you can do something about.
Also Check: Does Ibuprofen Make Asthma Worse
Do Genetics Affect Asthma
The gene pool is a complex topic that no one in the world can fully understand. However, astudy by the European Clinical Respiratory Journal shows that 70% of an individuals risk of developing asthma comes from genetics. Asthma is indeed hereditary, and children with one or both parents who suffer from asthma have a greater chance of suffering from it as well.
While there is nothing to be done to stop the genetic spread of asthma, parents can know the risk by researching family health history. After all, genetics extends to more people than just parents. A child may develop asthma from a grandparent or great-grandparent . Even if the parent doesnt suffer from asthma,a child may inherit it from someone else.
Whether hereditary or not, proper asthma maintenance is important for the health and safety of any asthmatic. It is also important to remember that genetics are primarily responsible for childhood asthma, not adult-onset asthma. Adult-onset asthma generally occurs due to allergens, anxiety, or an unhealthy BMI.
