Similarities And Differences In Regular Standard Treatment Of Asthma And Copd
-
In both diseases the adequate treatment may reduce symptoms and number of exacerbations and improve the quality of life.
-
Treatment of asthma is characterized by suppression of inflammation.
-
Treatment of COPD is characterized by decreasing of symptoms.
The GOAL of treatment in ASTHMA is to: reduce inflammation and to achieve¸total control . The GOAL of treatment in COPD is to: reduce symptoms, prevent exacerbations and decrease mortality . In both asthma and COPD almost the same drugs are used, but not in the same order and the same efficiency in treatment.
Knowing When To See A Professional
Clearly, there are numerous ways to effectively manage asthma and COPD, which means the prognosis for both diseases can be hopeful as long as each condition is caught early. While neither asthma nor COPD are considered curable, asthma is typically easier to control on a daily basis by avoiding triggers and taking the proper medication. As a progressive disease, COPD may get worse over time, but sticking with a physician-prescribed treatment plan can slow the disease’s progression and lessen symptoms.
The first step in successfully managing both conditions is to see a medical professional. Whether you suffer from difficulty breathing, coughing, wheezing or chest tightness or simply have a family history of the disease, you should consider seeking professional help. After consulting with a medical specialist, you will have a better idea of your condition and available treatment options.
It is especially important to receive medical attention specifically intended for your individual condition. Look for a rehabilitation center like Post Acute Medical that offers cardiopulmonary health services explicitly created to benefit asthma and COPD patients. At Post Acute Medical, there are precise treatment plans and therapies for a wide range of cardiopulmonary conditions, including COPD and asthma.
- Methods to maximize oxygen intake.
- Disease pathology.
- Infection control.
- Respiratory care.
Copd Vs Asthma: Which Is Worse
| | | | | | | | |
Asthma and chronic obstructive pulmonary disease are diseases of the lung that have a lot in common, but they also have key differences. Both conditions have similar symptoms caused by swelling of the airways or airway obstruction. Airflow limitation commonly results in breathing difficulties, coughing, wheezing, chest tightness, and shortness of breath.
Symptoms from asthma, triggered by allergens or exercise, come and go. COPD symptoms that can be caused by long-term smoking or prolonged exposure to chemical irritants are persistent. With COPD, chronic inflammation results in irreversible damage to the tissues lining the airways as well as pathological changes to the lung.
Though both diseases are chronic, COPD is a progressive condition, meaning symptoms are constant and the condition gets worse over time. With asthma, measures can be taken to control the disorder and when managed properly, its possible not to experience any symptoms for extended periods of time. Its important to distinguish COPD from asthma to determine the best course of treatment. Lets investigate the similarities and differences between asthma and COPD.
How Is Emphysema Treated
Because emphysema can worsen over time and there is no known cure, treatment is focused on slowing the speed of decline. The type of treatment will depend on the severity of the disease.
Quitting smoking: If you smoke, quit. This is the most important step you can take to protect your lungs. It is never too late to quit. Your doctor can help you find the best smoking quitting method for you.
Bronchodilator medications: These medicines relax the muscles around the airways. They are often used to treat . , given through hand-held inhalants, produce more immediate results and have fewer side effects than oral medications.
Anti-inflammatory medication: These medications reduce inflammation in the airways. However, long-term side effects of these drugs include , , high blood sugar, and fat redistribution.
Oxygen therapy: Oxygen therapy is prescribed for patients whose lungs are not getting enough oxygen to the blood . These patients cant absorb enough oxygen from the outside air and need to get more oxygen through a machine .
Lung volume reduction surgery: Lung volume reduction surgery involves removing a portion of diseased lung tissue, then joining together the remaining tissue. Doing this may relieve pressure on the breathing muscles and help improve lung elasticity . The results of the surgery have been very promising. Not all patients with emphysema are candidates for this surgery.
Diagnosing Asthma And Copd
With all the similarities between asthma and COPD symptoms, it can be challenging to diagnose each disease correctly without mistaking one for the other. Asthma is the most common alternative diagnosis for COPD. However, it is important to correctly identify which condition a patient is dealing with so they can receive the proper treatment.
When a patient has symptoms that pertain to both asthma and COPD, there are a few key factors that differentiate the two. To develop an accurate diagnosis, medical professionals will ask patients dealing with breathing issues specific questions about their symptoms, such as what time of day they feel the worst. They will also inquire about the patient’s medical, family and smoking histories and exposure to irritants, as well as gases or vapors.
Airflow Limitation In Copd
The chronic airflow limitation of COPD is caused by a mixture of small airway disease and parenchymal destruction , the relative contributions of which vary from person to person . Chronic inflammation causes structural changes and narrowing of small airways. Destruction of the lung parenchyma, also by inflammatory processes, leads to the loss of alveolar attachments to the small airways and decreases lung elastic recoil; in turn these changes diminish the ability of the airways to remain open during expiration .
So in COPD inflammation causes small airway disease and parenchymal destruction that all lead to airflow limitation .
Inflammatory Cells In Asthmatic Airways
Mast cells -activated mucosal mast cells release bronchoconstrictor mediatorshistamine, cysteinyl leukotriens, prostaglandin D2. They are activated by allergens through IgE receptors or by osmotic stimuli . Eosinophils are in increased number in airways, release basic proteins that may damage epithelial cells, and have a role in releasing a growth factors and airway remodeling , T lymphocytes are in increased number and release specific cytokines, including IL-4, IL-5, IL-9, IL-13 that orchestrate eosinophilic inflammation and IgE production by B lymphocytes . There may also be an increase in inKT cells which release large amounts of T helper: Th1 and Th2 cytokines . Dendritic cells,Macrophages are in increased number, and release inflammatory mediators and cytokines that amplify the inflammatory response . Nutrophils are in increased number in airways and sputum of patients with severe asthma and in smoking asthmatics, but the role of these cells is uncertain and their increase may even be due to steroid therapy .
Whos Likely To Have Asthma Copd Or Aco
People who smoke or breathe in pollution or chemicals at work for many years have higher chances of having COPD. That’s why the condition often starts in middle age or later in life.
Asthma is sometimes caused by gene changes that are passed down through families. If one of your parents has the disease, you’re more likely to have it.
Symptoms of asthma often start in childhood, and the condition is one of the most widespread long-term illnesses in kids. It affects about 1 in 10 children.
Besides a family history of the condition, a few things can raise your chances of asthma:
- Being around chemicals or other irritants in the air
People who get ACO tend to be over 40 but younger than people with just COPD, and they have .
Q: How Is Acos Treated
Your provider can begin treatment if you have COPD or asthma alone. But if you have ACOS, you may want to see a pulmonologista specialist in lung health. People with ACOS often experience more severe symptoms than those with a single lung disease, but working with a specialist can help you feel better. Treatment for ACOS usually includes medicine.
The Differences Between Copd And Asthma
editorial processSanja Jelic, MDMedical Review Board
and chronic obstructive pulmonary disease are both respiratory diseases involving chronic inflammation that leads to airflow obstruction. While they share similar symptoms, their causes and treatments differ. In some cases, asthma and COPD may overlap in what is termed asthma-COPD overlap syndrome, or ACOS.
However, the frequency and predominating symptoms in asthma and COPD are different. With COPD, you are more likely to experience a morning cough, increased amounts of sputum, and persistent symptoms. If you have asthma, you are more likely to experience episodic symptoms during and/or at night.
Another difference between asthma and COPD is the intermittent symptoms seen with asthma versus the chronic, progressive symptoms seen in COPD. Asthma symptoms are likely to occur after exposure to specific triggers, whereas COPD symptoms occur more regularly.
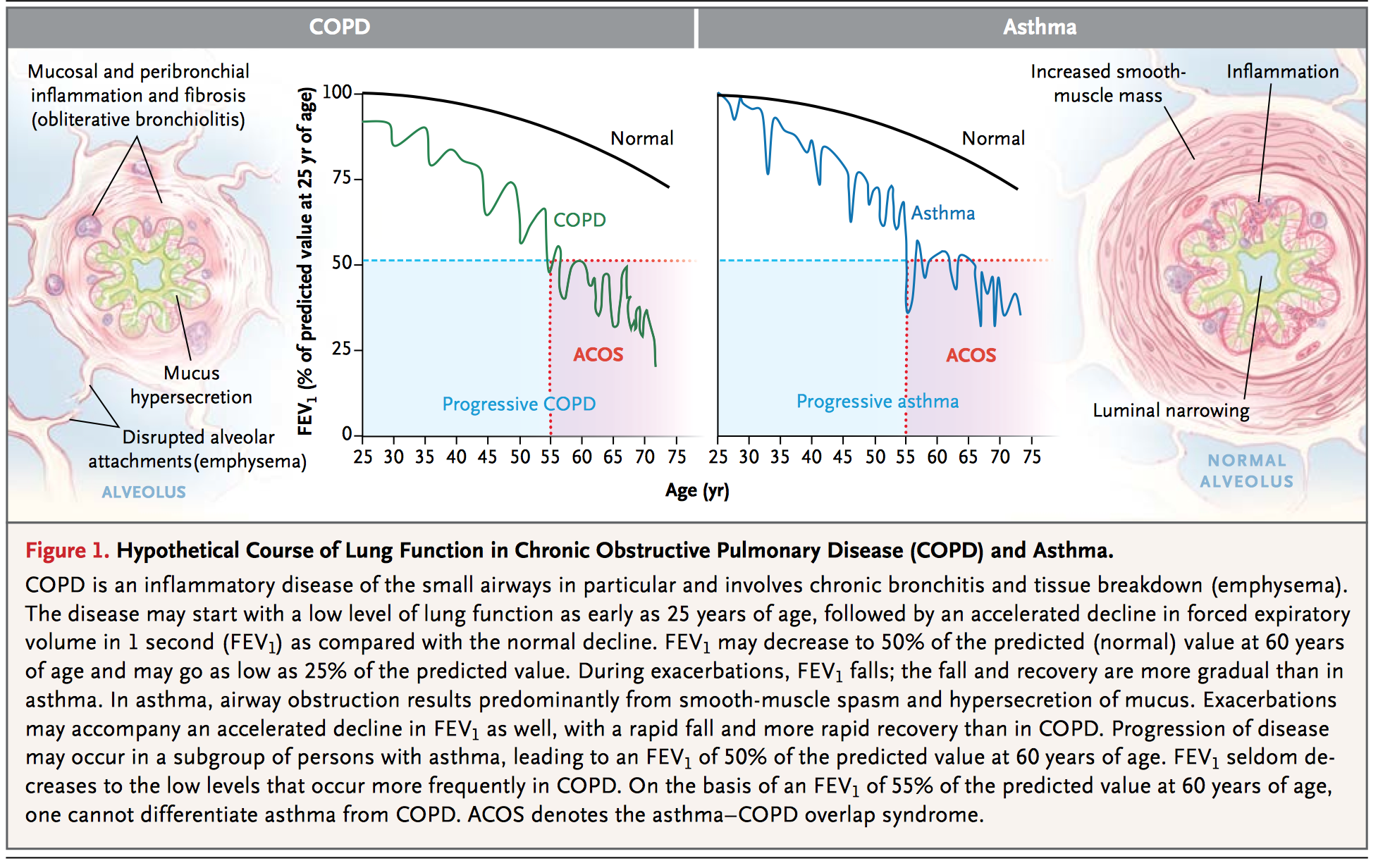
Clinical Recognition And Inflammatory Features Of The Overlap Syndrome: What Is It
The clinical recognition of both asthma and COPD requires assessment of symptoms and physiological abnormalities . Symptoms can indicate the presence of a disease process; however, their sensitivity and specificity for asthma or COPD may be limited. At a physiological level, patients with overlap syndrome have evidence of incompletely reversible airflow obstruction that can be detected by a reduced postbronchodilator FEV1 . In addition, they have increased variability of airflow, which can be determined by increased bronchodilator responsiveness or BHR. The presence of airflow obstruction can confound the assessment of BHR in COPD. For recognition of the overlap syndrome, it may be preferable to use an indirect acting stimulus to assess BHR. Such agents do not directly cause airway smooth muscle contraction, and include hypertonic saline, adenosine and mannitol.
Informative data can be obtained from studies of discrete patient groups who have features of asthma and COPD. These groups include patients with asthma who smoke, those with asthma who develop incompletely reversible airflow obstruction and non-smokers who develop COPD. Smokers with asthma have features resembling COPD, since they are less responsive to corticosteroids and are less likely to have eosinophilic inflammation and more likely to have increased airway neutrophilia.
Do Thunderstorms Worsen Asthma And Copd Symptoms
Anyone familiar with hay fever understands that weather impacts respiratory symptoms. However, many of weathers effects on respiratory function remain unclear. One unanswered question is the extent to which storms affect people with chronic lung disease, particularly the type affecting the way air moves in and out of the lungs. These obstructive lung diseases are characterized by problems with airway narrowing. The most common obstructive lung diseases are and chronic obstructive pulmonary disease . The two main types of COPD are chronic bronchitis and emphysema.
Obstructive lung diseases affect approximately 10% of the US population, and account for an outsized portion of hospitalizations and deaths. Indeed, COPD is the fourth most common cause of death among US adults.
What Is The Difference Between Asthma And Copd
Asthma is a respiratory disease affecting the bronchial tubes, or airways, making them sensitive to allergens or irritants, both of which can bring on an asthma attack. During an asthma attack, it is hard to breathe, and wheezing, coughing, and chest tightness may occur. While COPD can also cause these symptoms, its more likely to experience a consistent cough with phlegm.
Unlike asthma, COPD is a chronic condition caused by damage to the lungs over time, most often from smoking, and it is irreversible. With asthma, breathing returns to normal after an attack, but COPD symptoms are more regular. Usually, COPD develops in people after age 40 and becomes a chronic disease of lung function while asthma may develop in people of almost any age.
Can Asthma Turn Into Copd
Asthma doesnt always lead to COPD, but it is a risk factor. Lung damage caused by poorly controlled asthma along with continual exposure to irritants like cigarette smoke or occupational chemicals and fumes is irreversible and can increase a persons risk of developing the lung disease COPD. It is possible to have both asthma and COPD, a condition called Asthma-COPD overlap syndrome .
Asthma Vs Copd Over Time
- Asthma is usually considered a periodic disease. This means symptoms only occur sometimes. COPD is usually considered a persistent disease. This means that symptoms may appear to some degree all the time.
- Periods between asthma attacks may last days, weeks, months, or even years. In this way, asthma can seem to go into remission in some people. COPD flare-ups may also be periodic in this way. But, COPD does not go into remission.
- Asthma usually does not progress over time. COPD is generally considered a progressive disease. But, this progression may be slowed with a proper diagnosis and aggressive treatment.
- Speaking of diagnosis, both diseases may be confirmed with a test called a pulmonary function test . The test will show if triggers cause airflow limitation. It can also show if this airflow limitation is reversible or not reversible .
- Asthma medicines are used to prevent and control asthma symptoms. COPD medicines are used to allay symptoms and slow the progression of the disease.
Climate Change May Portend More Symptom Flares In People With Asthma And Copd
One of the effects of climate change is an increase in the number and severity of storms. As the climate changes, patients with lung disease will probably have more frequent, severe worsening of symptoms requiring emergency room visits. This would both increase the burden of disease in these patients and increase the stress on our healthcare system.
Asthma Treatment Options&copd Treatment Options
In many cases, both lung diseases treatments are the same, such as Bronchodilators and inhalable steroids, but there are also a few treatment options that are specific to each condition.People with asthma may be encouraged to stay away from triggers or avoid going outdoors when pollen levels are high. In cases of people with severe asthma, a bronchial thermoplasty may be recommended. The procedure burns off some of the muscles in the airway, reducing their ability to constrict.
On the other hand, people with COPD may be encouraged to alter lifestyle habits, such as quitting smoking, to help prevent any further damage. They may also be prescribed oxygen or pulmonary rehabilitation. In severe cases of COPD, procedures like lung volume reduction surgeries and lung transplants may be suggested.
Both Asthma and COPD are treatable diseases that will require some lifestyle changes. Staying informed on your options and taking care of your health is very important in managing lung diseases. For any further questions about these conditions and their treatments, click the link below!
Similaraties And Differences In Acute Exacerbation Of Asthma And Copd
-
Pathology is different in exacerbation of asthma and COPD
-
Causes of acute exacerbation of asthma and COPD are different.
-
Different role of LABA and ICS in prophylaxis of exacerbation of asthma and COPD.
-
Treatment of acute exacerbation is similar in asthma and COPD.
Acute exacerbation of Asthma
Triggers of acute exacerbation of asthma are usually: allergens, infections , GE reflux, other triggers, sometimes and co-morbidity .
Pharmacotherapy of acute asthma exacerbation
-
Bronchodilators ;
-
corticosteroids . Other therapy
-
oxygen therapy ;
-
non -invasive mechanical ventilation ;
-
antibiotics;
-
epinephrine rarely in a very serious asthma attack;
-
He/Ox rarely and MgSO4 intravenously rarely.
Acute exacerbation of COPD
Triggers of acute exacerbation of COPD are usually: infections , airpollution, GE reflux, sometimes and co-morbidity .
Pharmacotherapy of acute COPD exacerbation:
-
Bronchodilators ;
-
antibiotics in patients with severe exacerbation Other therapy:
-
oxygen therapy ;
-
non -invasive mechanical ventilation .
Knowing The Differences Between Copd And Asthma Is Vital To Good Practice
This content was published in 2011. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
The Outcomes strategy for people with chronic obstructive pulmonary disease and asthma was launched in July 2011 by the Department of Health, with the overall aim to drive improvements in outcomes for patients.1 Once implemented, it is expected to help people to avoid lung disease and lead longer and healthier lives. The strategy recognises the role of community pharmacy in supporting the management of people with respiratory disease through medicines use reviews and new pharmacy services.
In addition, the introduction of national target groups for MURs in England, under amendments to the NHS Community Pharmacy Contractual Framework, aims to ensure the service is provided to those who will benefit most. One of the target groups is patients with asthma or COPD.2 Both diseases have a major impact in the UK in terms of mortality and morbidity3 and the aim of MURs with these patients is to support them to take their medicines as intended, increase their engagement with their condition and medicines, and promote healthy lifestyles, in particular stopping smoking.
Is It Asthma Copd Or Both
Both asthma and chronic obstructive pulmonary disease , including emphysema and chronic bronchitis, make breathing difficult. In fact, they share many similarities. However, they are different lung diseases. Asthma-COPD overlap syndrome is diagnosed when you have symptoms of both asthma and COPD. ACOS is not a separate disease, but rather a way for doctors to recognize the mix of symptoms and select a treatment plan that is most appropriate for you.
Study Examined Relationship Between Thunderstorms And Copd Asthma Symptoms
![[Full text] The asthma](https://img.knowyourasthma.com/wp-content/uploads/full-text-the-asthma-copd-overlap-syndrome-do-we-really.jpeg)
In a recent article published in JAMA Internal Medicine, researchers analyzed Medicare claims from 1999 to 2012 to study whether storms led to an increase in respiratory illness-related emergency room visits in patients with obstructive lung disease. The study included 46,581,214 patients over 65 years old who had 22,118,934 emergency room visits due to respiratory complaints. Obstructive lung disease was a diagnosis in 43.6% of the patients, and included asthma , COPD , and combined asthma and COPD .
The researchers used meteorological data from the US National Oceanic and Atmospheric Administration to identify the dates when thunderstorms occurred. The NOAA database covers the continental US and includes data relating specifically to storms: windspeed, lightning, precipitation, and temperature. It also includes information on pollen and common air pollutants including small particulate matter , nitrogen dioxide, sulfur dioxide, ozone, and carbon monoxide.
Inflammatory Mediators Involved In Asthma
Chemokines are important in the recruitment of inflammatory cells into the airways and are mainly expressed in airway epithelial cells . Eotaxin is selective for eosinophils, whereas thymus and activationregulated chemokines and macrophage-derived chemokines recruit Th2 cells . Cysteinyl leukotrienes are potent bronchoconstrictors and proinflammatory mediators mainly derived from mast cells and eosinophils . Cytokines orchestrate the inflammatory response in asthma. Key cytokines include IL-1 and TNF, and GM-CSF. Th2-derived cytokines include IL-5, which is required for eosinophil differentiation and survival; IL-4, which is important for Th2 cell differentiation; and IL-13, needed for IgE formation . Histamine is released from mast cells and contributes to bronchoconstriction and inflammation . Nitric oxide , a potent vasodilator, is produced from syntheses in airway epithelial cells . Exhaled NO is increasingly being used to monitor the effectiveness of asthma treatment . Prostaglandin D2 is a bronchoconstrictor derived predominantly from mast cells and is involved in Th2 cell recruitment to the airways .
Airway structural cells involved in the pathogenesis of asthma are: airway epithelial cells, airway smooth muscle cells, endothelial cells, fibroblasts and myofibroblasts and airway nerves .
Diagnosing Asthma And Copd With Pft
I explained how a PFT can help diagnose asthma in my post at Asthma.net: What Are PFTs? I explained how a PFT can hep diagnose COPD in my post on this site, What Are PFTs?
So, if you read those, you know what an FEV1 is. You know how this can be used to determine if you have COPD. Still, heres a quick review. You do a PFT. You do a pre and post FVC. A computer determines your FEV1. This is the best indicator of airflow limitation.
You then use a bronchodilator. This can be either an inhaler or breathing treatment. Then you do a second FVC. Heres how you determine if its asthma or COPD.
- COPD. By its basic definition, its persistent respiratory symptoms and airflow limitation. Your pre and post bronchodilator FEV1 is less than 80%. Your post bronchodilator FEV1 is not much different than your pre bronchodilator FEV1. This shows that airflow limitation is persistent. It is not reversed with time or treatment. This confirms a diagnosis of COPD.1
- Asthma. By its basic definition, respiratory symptoms and airflow limitation are intermittent and vary in intensity. Asthma attacks are reversible with time or treatment. Your post bronchodilator FEV1 improves by 12% or more. This shows airflow limitation is reversible. This can help make a diagnosis of asthma. 2
- Asthma and COPD. This is when you have both. Your airflow limitation is reversible. But, your FEV1 remains under 80% despite treatment.
What Are The Different Types Of Copd
The two most common conditions of COPD are chronic bronchitis and emphysema. Some physicians agree that asthma should be classified as a chronic obstructive pulmonary disease, while others do not. A brief description of asthma, is included below:
| 1
What is chronic bronchitis?Chronic bronchitis is a long-term inflammation of the bronchi , which results in increased production of mucus, as well as other changes. These changes may result in breathing problems, frequent infections, cough, and disability. |
1
What is pulmonary emphysema?Emphysema is a chronic lung condition in which alveoli may be:
This can cause a decrease in respiratory function and breathlessness. Damage to the air sacs is irreversible and results in permanent “holes” in the lung tissue. |
1
What is asthma?Asthma is a chronic, inflammatory lung disease involving recurrent breathing problems. The characteristics of asthma include the following:
|
Who Is At Risk For Copd
The risk factors for COPD include
- Smoking. This the main risk factor. Up to 75% of people who have COPD smoke or used to smoke.
- Long-term exposure to other lung irritants, such as secondhand smoke, air pollution, and chemical fumes and dusts from the environment or workplace
- Age. Most people who have COPD are at least 40 years old when their symptoms begin.
- Genetics. This includes alpha-1 antitrypsin deficiency, which is a genetic condition. Also, smokers who get COPD are more likely to get it if they have a family history of COPD.
- Asthma. People who have have more risk of developing COPD than people who dont have asthma. But most people with asthma will not get COPD.
When To Talk With A Doctor
There is no set age for a COPD screening. Therefore, you should discuss symptoms with your doctor if you suspect COPD. Your doctor may be aware of your breathing difficulties and diagnose the condition without your prompting, but dont back if you suspect you have this lung condition. Early treatment will prevent the condition from getting worse.
Keep in regular contact with your doctor following a diagnosis of COPD. Reach out if you experience side effects to medications, worsening symptoms, or new symptoms.
Asthma In The Canadian Population
CCDSS Case Definitions
Prevalent Asthma Case Definition
The case definition of diagnosed asthma is: an individual aged one year and older having at least two visits to a physician with a diagnosis of asthma in the first diagnostic field in a two-year period, or at least one hospital separation with a diagnosis of asthma ever in any diagnostic field, coded by the International Classification of Diseases , ninth revision or ICD-9-CM 493 or ICD-10-CA J45-46. This case definition for asthma was validated by two independent studies in Ontario.Footnote 17Footnote 18
Only the first diagnostic field was used in physician billing claims data as not all provinces and territories had more than one diagnostic field. All fields were included from the hospital separation file as this database allows for the recording of up to 25 diagnoses.
Based on this definition, once a case is detected, it is a prevalent case for life regardless of future contact with health services. Consequently, once someone is identified as a case, they are always included in the database as a case. All jurisdictions identified cases occurring as of 1995, with the exception of Quebec which began in 1996 and Nunavut which began in 2005.
Active Asthma Case Definition
Incident Asthma Case Definition
Denominator Definition
Prevalence
Asthma
Figure 1.1 Prevalence of diagnosed asthma among Canadians aged one year and older, by age group and sex, Canada, 2011-2012
Active Asthma
Incidence
All-cause Mortality
