Overview Of Small Airways Disease
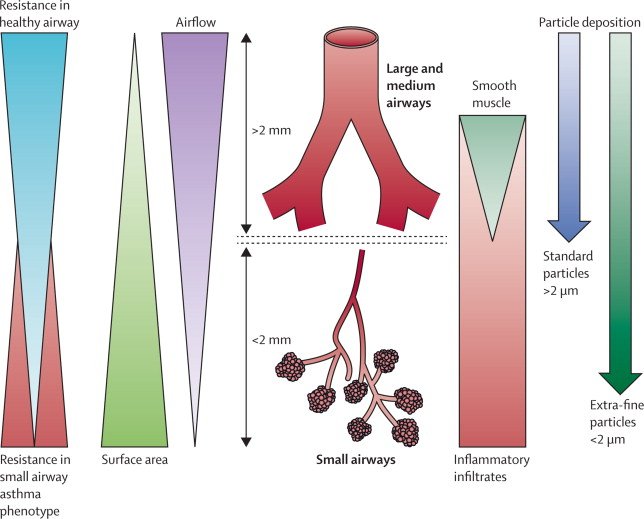
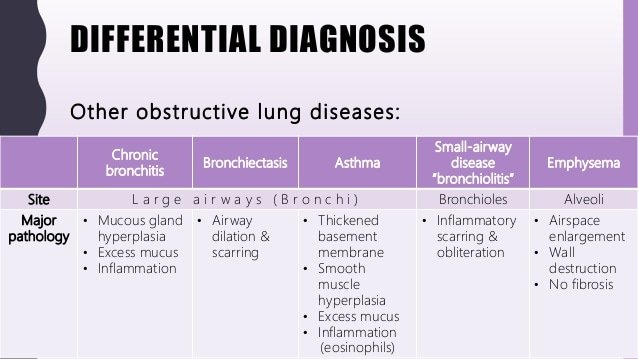
Small airways are usually defined as non-cartilaginous airways with an internal diameter <2 mm . These airways are located from approximately the eighth generation of airways down to the terminal bronchioles and respiratory bronchioles, which open into the gas-exchange apparatus . In normal lungs, small airways contribute only a little to total airway resistance , and it has been estimated that obstruction of 75% of all small airways is required before changes can be detected by routine pulmonary function tests ) . Small airways are not easily visualised by imaging techniques and their histopathological analysis is best analysed in surgical lung biopsies because bronchoscopic transbronchial biopsies usually contain only a few small airways. The difficulties of sampling these airways in human subjects are responsible for the limited recognition of the important pathophysiological roles of small airways, which have been called the silent zone. Small airways appear particularly vulnerable because many particles and infectious agents may be deposited there and because their narrow lumen makes them more susceptible to complete obstruction than larger airways. These considerations explain why: 1) small airways involvement occurs in many diseases either isolated or in association with abnormalities in large airways and alveoli; and 2) small airways represent the major site of airflow limitation in most airways diseases .
Airway Smooth Muscle Mass Was Increased In The Ova + Ozone Group
The ASM mass was increased in lung slices from mice treated with OVA + ozone, compared with control mice by 75.48% . The OVA group showed a slightly, but not significantly thicker ASM than the control group. The ASM mass in lung slices of the OVA + ozone mice was increased by 42.66% more than that of the OVA group . Correlation analysis demonstrated that the -SMA positive area was positively correlated with the FEV50 , but no correlation with other large- or small-airway variables was observed .
|
Figure 6 Airway smooth muscle mass was increased in OVA + ozone mice. Representative photomicrographs of immunohistochemical analysis of alpha-smooth muscle actin in lung tissue slices. Percentage of SMA-positive area around the airways. *P < 0.05, **P < 0.01. Scale bars represent 100 µm. |
Histological And Morphometric Analysis
After the lungs of mice were resected, the left lungs were inflated by injection of 4% paraformaldehyde to provide 20 cm of water pressure. They were then immersed overnight in paraformaldehyde, after which they were embedded in paraffin, and sectioned to expose the maximum surface area of lung tissue in the plane of the bronchial tree, and prepared for subsequent staining. Morphological changes of the lung and airway epithelium were assessed following hematoxylin-eosin , periodic acidSchiff , and Massons trichrome staining.
Peribronchiolar and perivascular inflammation was observed in the HE- stained lung slices and scored on a scale from 0 to 3, as previously described. The total number of leukocytes, neutrophils, eosinophils, and lymphocytes along the lobar bronchi and segmental bronchi were determined in 10 randomly selected, nonoverlapping fields under a magnification of 400× from two separate lung sections per animal. Average width of observed area was 100m. The airway inflammatory cells infiltration density was calculated as the ratio of cells to the whole length of bronchial wall counted.
Infiltration of inflammatory cells, and evaluation of airway mucus hypersecretion and collagen deposition were performed double-blind by two investigators independently.
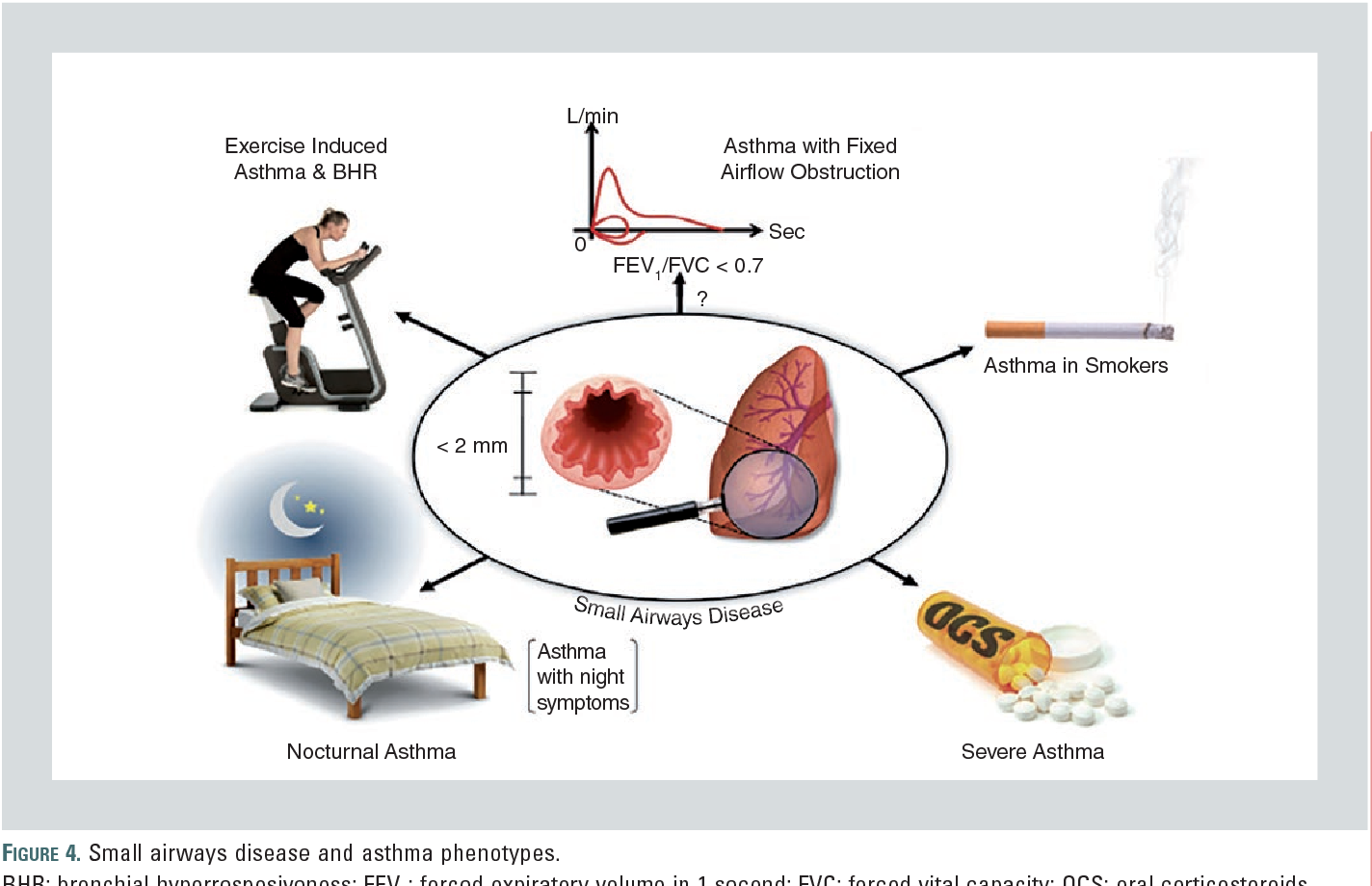
Sad And Asthma Control
A growing body of literature correlates IOS with asthma features, and overall, it emerges that asthma control appears to be linked with SAD.
In a study in 65 well-characterized patients, IOS-defined SAD correlated better with clinical symptoms and asthma control than spirometry-defined SAD; furthermore, greater small-airways reactance was associated with loss of asthma control . Pisi et al. showed that IOS-defined SAD was associated with poor disease control, assessed by the Asthma Control Test in 33 adult asthmatic patients with normal FEV1 . Manoharan et al. evaluated adult asthmatics with a preserved FEV1 , and showed that SAD assessed by FEF2575%, and R5R20 was associated with a significantly increased likelihood of having worse long-term asthma control . These results were confirmed by other studies with a similar design .
Notably, the risk of having poorer asthma control was greater when measurements of FEF2575%, and R5R20 were combined . R5R20 and AX were closely related to asthma control assessed by asthma control questionnaire , while spirometry did not . In ATLANTIS study , a SAD score has been calculated by use of impulse oscillometry and spirometry and associated significantly with asthma control, history of exacerbation and disease severity. The highest correlations were seen for airway resistance and reactance , peripheral conducting airway heterogeneity , and hyperinflation .
Integrative Medicine For Small Airways Disease In Copd
Airways <2 mm in diameter, which represent <10% of total airway resistance in normal individuals, contribute to the majority of the increase in total resistance in patients with COPD . This increase in total resistance may be related to a reduction of small airways numbers and/or to the narrowing of small airways. Because the total resistance of small airways is determined by the sum of the inverse resistance of each individual small airway, a removal of 50% of small airways is predicted to double small airways resistance. Narrowing of all small airways is predicted to result in an even greater increase in total small airways resistance because resistance varies inversely with the fourth power of the airway radius. From these calculations, it appears to be critical to determine whether the numbers of small airways are reduced in numbers in those with COPD.
From these studies, Hogget al. concluded that it is possible to measure a reduction in small airways numbers in Global Initiative of Obstructive Lung Disease stage IV COPD subjects. Terminal and pre-terminal bronchioles narrow and may disappear early in the course of the disease. These changes can be linked to regional differences in histology and gene expression in different pathological phenotypes of COPD. Changes in histology and gene expression are associated with the inflammatory immune cell infiltration and tissue remodelling process observed during repetitive tissue damage.
Increased Maximal Shortening Or Velocity Of Shortening
Besides alterations in contraction force, other properties of the ASM in asthma might play a role in excessive airway narrowing. It was suggested that increased maximal shortening of ASM might be such a feature. Mitchellet al. observed that in passively sensitised bronchial rings of peripheral airways, maximal ASM shortening was significantly greater in patients with asthma compared with individuals without asthma. In ASM obtained through endobronchial biopsies of patients with asthma and an asthma model using sheep trachea it was observed that there was increased maximal shortening of the ASM. However, in another study in large airways in patients with asthma no difference in maximal shortening was observed .
Allergic Airway Inflammation Induction And Ozone Exposure
C57BL/6 mice were randomly divided into three groups with eight mice in each group . The OVA sensitization was administered on days 0 and 7, with an intraperitoneal injection of 20 µg OVA dissolved in 0.2 mL of Dulbeccos phosphate buffered saline , emulsified in 2 mg aluminum hydroxide as an adjuvant. Challenge of OVA was induced on days 14, 16, 18, 20, and 22, with exposure to 5% aerosolized OVA in a plastic box that was linked to an ultrasonic nebulizer for 30 min. Mice in the control group were sensitized and challenged with the same volume of PBS as vehicle.
Mice were exposed to ozone at a concentration of 3 ppm, or air in a Perspex container 30 min after each OVA/PBS challenge on days 14, 16, 18, 20, and 22. Ozone was produced by an ozone generator . Every exposure lasted 2 h. Ozone concentration was continuously controlled and adjusted by an OS-4 ozone switch . The control mice were exposed to air during this time.
Drug Delivery In Severe Asthma With Small Airways Disease
Anti-inflammatory therapy with inhaled corticosteroids , with or without long acting B2-agonists , is the cornerstone of management of persistent asthma. Nonetheless, a significant number of patients do not gain optimal asthma control in spite of being treated with a high dose ICS/LABA combination , calling into question the ability of commonly used devices to deliver medication to the small airways. For individuals with small airways disease, and certainly for those with severe asthma, anti-inflammatory therapy needs to reach and address inflammation of the entire affected airway, and therefore efficacy of delivery becomes very important when selecting treatment .
Unmet Needs In Severe Asthma And Small Airways Disease
Unmet needs:
A reliable index of noninvasive, widely available testing would allow easier diagnosis and monitoring of small airways disease in the primary care and specialty setting.
Additional studies need to assess the long term benefit of extra-fine particle inhaler therapy on remodeling, lung function, and other outcomes for individuals with small airways disease.
Despite an ever-increasing utilization of biologic medications for individuals with moderate to severe asthma, the benefit of these therapies for small airways disease has not been well established.
The impact of small airways disease in children with severe asthma is not well described. Further studies assessing the prevalence, clinical features, assessment, and effect of treatments on small airways disease in asthma should focus on the pediatric population.
Whos Likely To Have Asthma Copd Or Aco
People who smoke or breathe in pollution or chemicals at work for many years have higher chances of having COPD. That’s why the condition often starts in middle age or later in life.
Asthma is sometimes caused by gene changes that are passed down through families. If one of your parents has the disease, you’re more likely to have it.
Symptoms of asthma often start in childhood, and the condition is one of the most widespread long-term illnesses in kids. It affects about 1 in 10 children.
Besides a family history of the condition, a few things can raise your chances of asthma:
- Being around chemicals or other irritants in the air
People who get ACO tend to be over 40 but younger than people with just COPD, and they have .
Spirometry In Mice Using The Forced Manoeuvres System
Mice were anesthetized with Zoletil 50 and xylazine hydrochloride via IP injection, 24 h after the last challenge. Following tracheostomy, mice were fitted with a tracheal cannula, and attached to a plethysmograph with a pneumotachograph using the eSpira Forced Manoeuvres System for mice . The animals lungs were inflated to a set tracheal pressure, and then exposed to a large negative pressure reservoir, forcing the mouse to exhale as quickly as possible, to mimic classical clinical spirometry. Variables, including the FVC, FEV25, FEV50, FEV75, FEF25 , FEF50, FEF75, and MMEF, were calculated. Among them, the FEV25, FEV50, FEV75, and FEF25 represented large-airway function; whereas the FEF50, FEF75, and MMEF indicated small-airway function.
Common Variable Immunodeficiency Disorders
CVID represent a heterogeneous group of conditions characterised by a low level of circulating IgG, IgA and/or IgM, and leading to increased susceptibility to infections . Although the pathophysiology of CVID is not fully understood, it seems that B-lymphocytes fail to undergo normal maturation into plasma cells . Abnormalities in T-lymphocytes are also frequently observed in patients with CVID . The prevalence of CVID is estimated as approximately one in 30 000 individuals. Clinical manifestations in patients with CVID are related to three mechanisms: 1) recurring infections related to the failure to produce sufficient antibody levels; 2) autoimmune diseases that are observed in up to 20% of patients and are probably related to immune dysregulation or to a defect in antigen clearance ; and 3) lymphoid hyperplasia with increased incidence of B-cell lymphoma, thymoma and solid cancer .
At the pulmonary level, recurring infections may be responsible for bronchiectasis . Lymphoid hyperplasia and granulomatous lesions may infiltrate alveoli and bronchioles; this non-infectious complication of CVID is being called granulomatous-lymphocytic interstitial lung disease .
Asthma And Copd: What’s The Difference And Is There A Link
and chronic obstructive pulmonary disease are lung diseases. Both cause swelling in your airways that makes it hard to .
With , the swelling is often triggered by something youâre allergic to, like or , or by physical activity. is the name given to a group of lung diseases that include emphysema and chronic bronchitis.
happens when the tiny sacs in your are damaged. Chronic bronchitis is when the tubes that carry air to your get inflamed. is the most common cause of those conditions .
gets better. Symptoms can come and go, and you may be symptom-free for a long time. With , symptoms are constant and get worse over time, even with treatment.
Imaging Of Small Airways Disease
Potential interest and limitations of the various imaging techniques that can be used for the diagnosis of small airways disease have been described previously . Volumetric CT scans with thin sections allow multiplanar coronal or sagittal reconstructions with maximum intensity projection and minimum intensity projection images, and is the preferred imaging technique in subjects suspected of small airways disease . Inspiratory and expiratory acquisitions are routinely obtained for assessing small airways using qualitative analysis. To date, quantitative analysis based on measurements of voxel attenuation values has only been used for research purposes. Novel voxel-wise image analysis techniques are currently being developed and may provide improved assessment of small airways disease in the near future .
Representative images of computed tomography scans in patients with small airways disease. a) An inspiratory CT scan in a patient with hypersensitivity pneumonitis showing mosaic pattern of attenuation. b) Expiratory CT scan in the same patient showing air trapping that is characteristic of small airways disease. c) Ill-defined centrilobular nodules in a patient with farmer’s lung . d) Localised micronodules branching with bronchovascular structures related to tuberculosis in a patient with rheumatoid arthritis receiving treatment with anti-tumour necrosis factor-. Reproduced from with permission from the publisher.
Bronchoalveolar Lavage Collection And Measurements
After airway function tests were performed, mice were sacrificed. The trachea of each mouse was lavaged with three aliquots of 0.6 mL cold PBS through a polyethylene tube . Bronchoalveolar lavage fluid was retrieved and the return volume was consistently 70% of the instilled volume. The BALF was then centrifuged at 3000 r/min for 10 min at 4 °C. Total cell counts were calculated by a hemocytometer under optical microscope. And the supernatant was used for the enzyme-linked immunosorbent assay using commercial kits , according to the manufacturers protocol.
Analysis Of Muc5ac Gene Expression
Muc5ac is a representative component of airway mucus. Total RNA was isolated from lung tissue using the TRIzol Reagent . After the determination of concentration and purity, RNA was translated into cDNA using a cDNA reverse transcription kit in a PTC-200 Peltier Thermal Cycler . Real-time quantitative PCR was performed using a ViiA 7 Real-Time PCR System . The RT-PCR thermal cycling program was as follows: one cycle of pre-denaturation at 95 °C for 5 min; followed by 40 cycles of denaturation at 95 °C for 15 s; annealing at 60 °C for 30 s; and elongation at 72 °C for 30 s. Fluorescence intensity of the internal reference gene and target gene expression were detected. The relative expression of target genes was calculated by the 2Ct method.
The following primer sequences were used in the PCR:
-actin: Forward-5 CCT CTA TGC CAA CAC AGT 3,
Reverse-5 AGC CAC CAA TCC ACA CAG 3;
Muc5ac: Forward-5 TCA CAT TTG ATG GCA CCT ACT 3,
Reverse-5 CAC ACG GAA GTA TCC AAA CAC 3
Small Airways As A Therapeutic Target In Asthma
On the basis of the physiological and pathological evidence presented in the present review, small or peripheral airways and lung parenchyma are clearly implicated in the pathogenesis of asthma. Because this is the ‘quiet’ zone, however, damage in the small airways often goes undetected. What is unclear at present is whether inhaled corticosteroids effectively treat this compartment of the lung. Although inhaled corticosteroids reduce airway inflammation in patients with mild-to-moderate asthma , prolonged courses of inhaled steroids do not normalize hyper-responsiveness . Furthermore, it was demonstrated in deposition studies that most of the currently used inhaled corticosteroids are predominantly deposited in the central airways and not in the lung periphery .
Metered-dose inhalers , pressurized inhalers, or dry powder inhalers are not very efficient at depositing medication in the more peripheral airways of the lung. These delivery systems typically deliver no more than 15% of the inhaled dose to the lungs . The challenge for the pharmaceutical companies is to improve the technology of aerosol delivery systems. This will ultimately allow delivery of anti-inflammatory drugs to the peripheral and to the central inflammatory sites with minimal oropharyngeal deposition. Such technologies will thus enable us to treat inflammation uniformly throughout the airways.
Pathology Of Small Airways In Asthma And Copd
In healthy subjects, small conducting airways have a thin wall and offer little resistance to airflow that is laminar . Importantly, resistance to airflow varies inversely with the fourth power of the airway radius. A decrease in airway radius may be the result of increased amount of mucus and inflammatory cells obstructing the airway lumen, increased thickness of the submucosa related to inflammation, fibrosis or increase in smooth muscle mass, and distortion and narrowing of the lumen by the loss of alveolar attachments.
The pathological changes found in patients with COPD are probably related to innate and adaptive immune responses, but are also determined by the microenvironment that modulates the type of immune response to produce destructive responses in parenchyma and fibrosis in small airways. Several questions remain to be answered. The pathology of small airways during COPD exacerbations is unknown because such tissue is difficult to obtain, except from autopsy specimens. An important limitation is that these specimens may show many changes related to post mortem alterations rather than exacerbation-related changes. Furthermore, pathological data on small airways in COPD were obtained in cross-sectional studies, and no longitudinal data are available. As a result, the relationship between pathological changes in small airways and subsequent development of airflow limitation remains unknown.
Evaluating An Asthma Attack
Because people who are having a severe asthma attack commonly have low blood oxygen levels, doctors may check the level of oxygen by using a sensing monitor on a finger or ear . In severe attacks, doctors also need to measure levels of carbon dioxide in the blood, and this test typically requires obtaining a sample of blood from an artery or, occasionally, a vein. However, carbon dioxide levels can sometimes be monitored in the person’s breath using a sensor placed in front of the nose or mouth.
Doctors may also check lung function, usually with a spirometer or with a peak flow meter. Usually, a chest x-ray is needed only when asthma attacks are severe, in order to rule out other serious conditions .
Ova Caused Peribronchial Collagen Deposition
OVA sensitization/challenge induced peribronchial collagen deposition . Compared with the control group, collagen deposition was increased in both the OVA and OVA + ozone groups , indicating airway remodeling in the asthma models. The T2-high model seemed to have shown more severe collagen deposition than the T2-low model; however, no significant differences were observed between the two models.
|
Figure 5 Collagen deposition in the lungs of mouse models of asthma. Representative photomicrographs of Massons trichrome stained lung tissue. Percentage of subepithelial Masson stained area . ***P < 0.001. Scale bars represent 100 µm. |
Asthma Uk Community Forum
Hi, I have been a chronic asthmatic for years and escaped hospital after 22 days last week, this was my 4th admission this winter. Upon discharge I was told that I also have Small Airways Disease and that I was been referred to a Professor Sabro in Sheffield as my consultant feels that she has tried everything available without much joy.
Does anybody on here know much about Small Airways Disease or have any dealings with Prof. Sabro?
Thanks in advance.
Sounds like you have had a tough winter with hospital. 22 days is a long time. Hope you are better now. Im in Scotland so have no dealings or heard of the guy you have been referred to at Sheffield but the wonders of the internet now you will be able to find out their background and special interests etc.
I was replying mainly about your question about small airways disease. I was told many years ago I had Brittle Asthma and small airways disease but never told much more about it. They have not treated anything differently. I think what they mean by small airways disease is that your lower airways are effected. Asthma falls under the small airways disease but it is never clear with asthma which bits of your lungs are effected so to speak. It is generally your bronchi that are effected which are the larger or the airways but infection tends to effect the smaller airways which is where I think they get the small airways disease from.
Hope this has helped a bit.
justTUX
Thanks in advance.
Small Airways In Severe Asthma
A definitive assessment of the impact of small airways disease on severe asthma is limited by the lack of a practical gold-standard determinant of the small airways. However, using the aforementioned surrogate markers of small airways disease, including physiologic assessments and imaging techniques, many published studies implicate small airways dysfunction in increased symptoms, risk of exacerbations, and asthma severity. Measures of small airways disease can change with asthma treatment and correlate with asthma control . Further, small airways dysfunction is implicated in asthma severity of both adults and children.
Usmani and colleagues performed a systematic review to determine the prevalence of small airways disease in adult asthma. Fifteen studies were identified, which utilized a variety of techniques including spirometry, plethysmography, nitrogen washout, impulse oscillometry, and high-resolution computed tomography to assess the small airways. Overall estimates determined small airways disease affects 50-60% of individuals across the range of persistent asthma severity . In children with asthma, a majority suffer from small airways disease, determined using FeNO and nitrogen washout .
What Is The Difference Between Reactive Airway Disease And Asthma
With increasing pollution and environmental issues, airway diseases are highly prevalent in the world today.
If you are suffering from respiratory conditions, it is highly possible that you have come across the terms of reactive airway disease and asthma.
Although both these terms are many times used interchangeably, these are not the same.
In many cases, the symptoms and signs might be similar to each other. It is therefore highly possible that you might get confused between these two diseases.
But as there is a huge difference between these two terms, which must be clear to you, lets discuss the difference between reactive airway disease and asthma in detail along with its possible treatment options.
In This Article …
Environmental Or Occupational Exposure
Hypersensitivity pneumonitis
Hypersensitivity pneumonitis is one of the most frequent causes of small airways diseases. It is usually due to the inhalation of organic dust but can also occur with the inhalation of chemical compounds . Pathologically, hypersensitivity pneumonitis is characterised by an inflammatory process with granulomatous infiltration of the lung interstitium and small airways. Although hypersensitivity pneumonitis is often considered an interstitial lung disease, small airways disease is constant and sometimes predominates .
Farmer’s lung and pigeon breeder’s disease are among the most frequent forms of hypersensitivity pneumonitis, but novel environmental exposures can also be involved. For example, exposure to household moulds has been associated with hypersensitivity pneumonitis . Exposure to Mycobacterium avium intracellulare in hot tubs or to Mycobacterium immunogenum in metalworking fluids used in the industrial sector have also been associated with hypersensitivity pneumonitis.
Clinical manifestations of hypersensitivity pneumonitis include chronic cough and sputum production in up to 50% of patients . Nonspecific bronchial hyperresponsiveness and wheezing may also be prevalent in subjects with recent hypersensitivity pneumonitis, especially in dairy farmers .
Bronchiolitis related to other environmental exposures
Radiographic Identification Of Small Airways Inhomogeneity
High-resolution computed tomography methodology has permitted a non-invasive direct radiographic assessment of the luminal caliber and wall thickness of medium and large airways of >2mm in diameter that is reproducible and related to clinical disease severity . However, while the limits of resolution of HRCT imaging do not currently allow direct assessment of the small airways, one can indirectly evaluate changes in airways of<2mm in diameter through measures of changes in regional air trapping, indicated by areas of low lung attenuation of 900 Hounsfield units. With the asthma subject performing a suspended breath hold at RV, areas of low attenuation can be visualized intermixed with areas of higher attenuation, creating a black and white mosaic pattern. Low lung attenuation regions, in black, represent air trapped behind functionally closed peripheral airways and are easily differentiated from high attenuation lung regions, which appear white, from which air has been normally expelled through patent airways. Changes in air trapping can also be assessed within regions of the lung under different physiologic conditions such as after bronchodilator or after allergen or methacholine challenge . Radiation exposure remains a limitation of HRCT.
