Rare Gene Mutation In Some Black Americans May Allow Earlier Screening Of Heart Failure
by NIH/National Heart, Lung and Blood Institute
Researchers have linked a rare genetic mutation found mostly in Black Americans and other people of African descent to an earlier onset of heart failure and a higher risk of hospitalization. The findings suggest that earlier screening for the mutation could lead to faster treatment and improved outcomes for heart failure in this vulnerable group, the researchers said. The results of the study, which was largely supported by the National Heart, Lung, and Blood Institute , part of the National Institutes of Health, appear in the Journal of the American College of Cardiology: Heart Failure.
“This is the most comprehensive evaluation of the association between this mutation and measures of cardiac structure, heart function, and heart failure risk in an exclusively Black population,” said lead study author Ambarish Pandey, M.D., assistant professor of internal medicine in the Division of Cardiology at University of Texas Southwestern Medical Center in Dallas. “The results also highlight the importance of early genetic screening in patients at higher risk for carrying the mutation.”
“What that means is that the gene is causing heart damage slowly over time,” said Amanda C. Coniglio, M.D., the lead author of the study and a physician with Duke University School of Medicine in Durham, North Carolina. “The changes are subtle but significant.”
Explore further
Contribution Of Inherited Factors
The central tenet of research in asthma genetics is that clinical disease only occurs in a subject with a genetic susceptibility, which becomes expressed after exposure to an environmental trigger. Several environmental factors have been proposed, including house dust mites, cigarette smoke, viral respiratory tract infections, and atmospheric pollution. Unfortunately, the elements of the genetic susceptibility have proved to be more elusive. Although the prevalence of asthma in a population is approximately 4â8% , this increases to 20â25% in those with affected first degree relatives. This measure can be expressed as the risk ratio , which is defined as the prevalence of a disease in first degree relatives of an affected subject divided by the prevalence in the general population. In asthma, λS is approximately 5â6, compared with 15 in type I diabetes mellitus, 8 in schizophrenia, and 3.5 in type II diabetes mellitus.
Monozygotic and dizygotic twin studies have examined the concordance of a number of traits, such as asthma symptoms, total IgE, and skin test hypersensitivity, and have shown variable, but significant, inherited contributions . As with other multifactorial diseases, the contribution of genetic factors is influenced by the population being studied and the propensity to sharing a common environment.
Can Dupilumab Calm Inflammation In Asthma
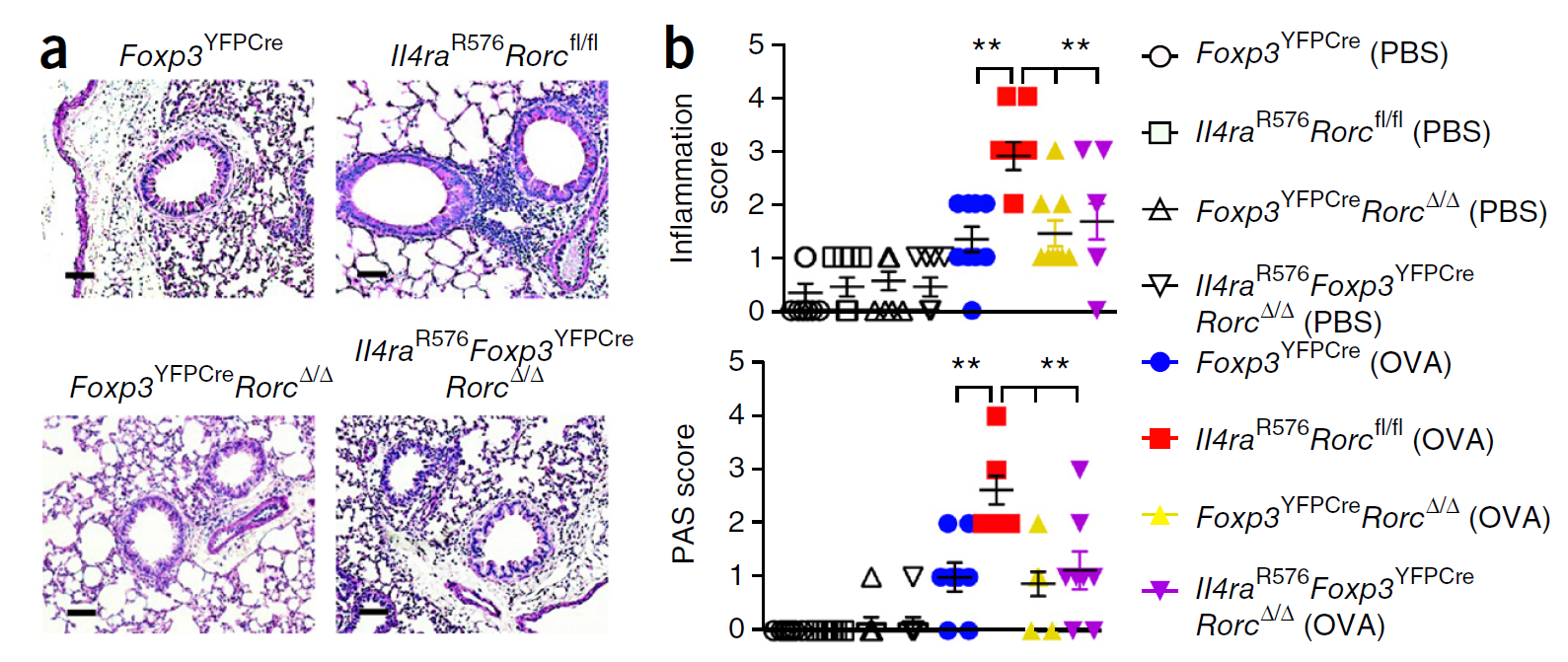
Called IDEA , the trial will test dupilumab in 150 people age 12 and older, with and without the ILR4 mutation. Participants will enroll at Boston Childrens, Brigham and Womens Hospital, the Henry Ford Health System in Detroit, and the Atlantic Health System in New Jersey.
The trial is a natural outcome of earlier scientific work by Dr. Phipatanakul and Dr. Talal Chatila, also in the Division of Immunology. They showed that mutations in IL4R alter the cell receptor for the chemical messenger IL-4. This leads to increased airway inflammation via two types of T cells, Th2 and Th17. In fact, the mutation converts normally benign regulatory T cells, which help calm immune responses, into cells much like inflammatory Th17 cells.
Having two mutated copies of IL4R further increases asthma severity. Severity is even worse, Dr. Phipatanakul has found, if children are also exposed to toxins in the air .
Dupilumab, a monoclonal antibody, blocks the mutated IL-4 receptor, and the researchers hope it will also curb asthma inflammation. The study will compare responses to the drug in people with one, two, or no copies of the IL4R mutation.
We specifically want to help the patients who are most in need, says Dr. Phipatanakul. Based on our earlier work, we expect that people with two copies of the genetic variant will respond the most. Were excited to take the science to the next logical step.
You May Like: Can You Join The Air Force With Asthma
Single Genetic Glitch May Explain Most Allergies And Asthma
Follow
Allergies are certainly the result of both genetic and environmental factors, but there is fresh evidence to suggest that at least one major genetic aberration could be behind everything from hay fever to food allergies to asthma.
Allergies to dust, pet hair or peanuts are essentially the product of misdirected immune systems, which start to see innocuous objects as potential threats and launch an intensive assault that can translate into sneezing, wheezing, and even potentially fatal seizures. For decades now, rates of allergies and other immune-related diseases such as asthma and eczema have been rising in the U.S., and the rapid increase suggests that its more than just genes, or just changes in lifestyle that made us too clean that are at work.
Now researchers studying the genetics behind the rare tissue disorders Marfan and Loeys-Dietz syndromes have discovered that there may be a common genetic driver behind almost all allergic diseases. Reporting in the journal Science Translational Medicine, scientists from Johns Hopkins Childrens Center and the Johns Hopkins Institute of Genetic Medicine say that they were surprised to find that the same mutation they found in the Marfan and Loeys-Dietz patients may also trigger the immune changes responsible for allergies most of the patients with the two rare disorders also have higher than normal rates of allergies.
Characterisation Of Asthma By Eosinophilic Inflammation
Histopathological studies of the airway inflammation in asthma have found an increase of eosinophils, lymphocytes, plasma cells, and mast cells in patients with asthma. The resultant phenomena of mucosal oedema, vascular congestion, bronchoconstriction, increased mucus production, and impaired ciliary function are thought to be a consequence of the interaction and activation of these inflammatory cells. In addition, several in vivo studies have shown the presence of allergic inflammation in those affected by persistent asthma as well as asthma induced in susceptible subjects by exogenous antigens. In patients with mild, stable asthma with persistent symptoms and an increased airway responsiveness, bronchial biopsy samples and broncheoavleolar lavage cell studies have shown an increased number of eosinophils, lymphocytes, and mast cells. In addition, the eosinophils showed evidence of activation with increased concentrations of major basic protein, eosinophilic cationic protein, and other granular proteins. Such findings in patients with mild, stable asthma not only provide clues to the pathogenesis, but should also raise considerable concern in doctors as they indicate chronic inflammation in those otherwise considered to have trivial asthma.
Read Also: Does Weight Gain Make Asthma Worse
Molecular Genetics Of Asthma
Over a hundred different genes have been associated with asthma and the list is still growing. Asthma susceptibility genes fall mainly into three categories relating to 1) functioning of the immune system, 2) mucosal biology and function, and 3) lung function and disease expression . However, just because a gene has been associated with asthma in a single study does not necessarily establish a connection between that gene and the disease. A major problem in many genetic studies of asthma is the lack of replication of results from previous studies. Notably, only a subset of identified genes has been found to be associated with asthma in more than one study and many regard replication as one of the most important features of a gene’s candidacy . However, some genes may be important only in a subset of asthmatics, for example, in childhood-onset asthma, atopic asthma, house dust mite sensitive asthma, or occupational asthma, and therefore replication across these different populations cannot always be expected. Moreover, some genes are expressed only in certain environmental contexts, for instance, in children growing up with a cat or in those exposed to passive smoking in the first years of life . The importance of gene-environment interaction in asthma causation should not be underestimated every gene’s role should be viewed within the context of a permissive environment.
Gene Mutation Causes Asthma
A team of researchers at Weill Cornell Medical College, Columbia University Medical Center and SUNY Downstate Medical Center have found the cause of a common type of childhood asthma, and its not rooted in allergens.
The way in which asthma develops is a subject of much scientific interest, considering that the way it develops and affects people varies considerably.
The team identified that an over-active gene ORMDL3 was linked to around 30 percent of childhood asthma cases. The gene is responsible for disrupting the synthesis of lipid molecules . They arent fully sure how a reduced production of sphingolipids can cause asthma, yet the results of their study clearly indicate there is a link.
The study, published in Science Translational Medicine, revealed a completely unique pathway for asthma which does not have anything to do with allergens or inflammation.
The senior author of the study, Dr. Stefan Worgall, said:
Usually asthma is thought to be an inflammatory disease or a reaction to an allergen. Our model shows that asthma can result from having too little of a type of sphingolipids. This is a completely new pathway for asthma pathogenesis. Our findings are not only valuable in understanding the pathogenesis of this complex disease, but provide a basis to develop novel therapies, especially asthma agents based on a patients genotype.
Also Check: Does Chihuahua Help Asthma
Personalised Medicine And Pharmacogenetics
Personalised medicine is becoming increasingly important in the post-genomic era. The idea behind personalised medicine is to predict, based mostly on genetic information, which patients will experience the best response to treatment. As this field advances, it will be possible to individualise pharmacotherapy based on genetic polymorphisms so that certain drugs are administered only to those patients who are most likely to respond, while harmful effects are avoided in patients who are most likely to experience toxicity and adverse reactions . Candidate genes for such studies are those encoding receptor proteins and enzymes involved in drug transportation, processing, degradation and excretion. The continuing elucidation of the biological pathways underlying asthma and allergy will help identify new possible targets for intervention. For example, in a randomised study of an experimental drug blocking the IL-4/IL-13 pathway, certain amino acid variations in the IL4 receptor seemed to predict which patients would have the best therapeutic treatment response in terms of increased lung function .
Rare Mutations Do Not Explain ‘missing Heritability’ In Asthma
by University of Chicago Medical Center
Despite a strong suspected link between genetics and asthma, commonly found genetic mutations account for only a small part of the risk for developing the disease – a problem known as missing heritability.
Rare and low frequency genetic mutations have been thought to explain missing heritability, but it appears they are unlikely to play a major role, according to a new study led by scientists from the University of Chicago. Analyzing the coding regions of genomes of more than 11,000 individuals, they identified mutations in just three genes that were associated with asthma risk. Each was associated with risk in specific ethnicities. Their findings, published in Nature Communications on Jan. 16, suggest gaps in the current understanding of asthma genetics.
“Previous studies have likely overestimated the heritability of asthma,” said study senior author Carole Ober, PhD, Blum-Riese Professor and chair of the Department of Human Genetics at the University of Chicago. “This could be because those estimates are based on correlations between family members that share environment as well as genes, which could inflate the heritability. Gene-environment interactions are not considered in these large scale association studies, and we know that these are particularly important in establishing individual risks for asthma.”
Explore further
Don’t Miss: What Is The Blood Test For Eosinophilic Asthma
Other Omic Studies And Integration Of Multiomics
Other omics technologies, apart from genomics, are powerful tools to increase the current knowledge about asthma pathophysiology . These are focused on data from a wide variety of biological sources: genomic modifications , gene transcription , protein levels and chemical modifications , endogenous and exogenous metabolites , and the microbiome , among others . The application of omics approximations in asthma is still incipient compared to other diseases . Still, several studies have been performed in asthma in the last years as it was reviewed elsewhere .
To our knowledge, a total of 26 asthma studies using other omics approaches have been published in the last 2 years . Just like recent GWAS of asthma, these studies have been equally focused on childhood and adulthood asthma since 2016. Moreover, most of them have been carried out in patients of European descent. A total of 18 studies focused on asthma susceptibility or severity three focused on the ICS response two explored the interactions with environmental factors and three inspected the overlap with other pulmonary diseases . Nonetheless, other experts have discussed the recent omics advances in asthma in this issue except for those of transcriptomics. Therefore, we focused on summarizing the main findings of studies made using this approach.
Does Asthma Run In The Family
Asthma, a chronic lung condition that affects the airways, can occur in people of all ages. In some cases, asthma symptoms can be mild and are well controlled with asthma medications. For others, symptoms are more severe and can have a debilitating effect on daily life and work. Asthma and other atopic conditions can run in the family, meaning if you have a family history of the condition, you are more at risk to developing it.
Theres no cure for this bronchial condition, but it can be effectively managed with modern treatments, and research continues to reveal more about asthma causes.
Read on to discover if asthma is genetic or environmental and if theres any truth in the idea that asthma can run in families.
You May Like: What To Do During Asthma Attack Without Inhaler
Asthma Gene Mutation Discovered On Island
Find your bookmarks in your Independent Premium section, under my profile
Researchers have identified a mutated gene that makes people susceptible to asthma, having discovered it on one of the world’s most isolated islands.
Sequana Therapeutics analysed DNA from about 300 people on Tristan da Cunha, an island in the south Atlantic, about 1,500 miles from South Africa. About 30 per cent of the island’s residents have asthma, apparently passed on from an original settler.
The pinpointing of the mutated genes eventually could help identify people at risk of getting sick, and also could suggest new drugs for treatment.
“We found a difference – a change in that DNA that is different in people who have asthma than those that don’t have the disease,” said Bob Giargiari, of San Diego-based Sequana.
The researchers said that, of the estimated 15 million Americans with asthma, up to 10 per cent seemed to have a genetic predisposition to the disease.
Overlap Among Asthma And Allergic Diseases
Given the firm links in the pathogenesis of asthma and other allergic diseases , a few studies used this rationale to explore the overlapping genetic architecture among these diseases , including two large-scale GWAS published between 2016 and 2018 .
Table 4. Novel loci of asthma and allergic diseases revealed by meta-analyses published between 2016 and 2018.
Besides these findings, 29 of the genes identified by Ferreira et al. encode for proteins that are drug targets for several diseases, including allergic and auto-immune diseases. Interestingly, the protective effect of these genes was found to be correlated with the effect of drugs targeting them, attenuating allergy symptoms. These findings suggest that these could be effective targets to treat allergic diseases or asthma and thus, the proteins encoded by these should be prioritized for pre-clinical evaluation .
Also Check: Does Weight Gain Make Asthma Worse
Studying Dna Marks In Asthma
The study looked at nose tissue samples from nearly 500 children and teens living in Puerto Rico, including 169 children with allergic asthma. This is the most common type of asthma, in which allergens, such as pollen, dust, and pet dander, cause tightening of the airway, leading to wheezing and shortness of breath. The research team identified all the DNA marks across each childâs entire DNA code and compared them with the marks in children who do not have asthma.
The principal investigator of this research effort, Juan C. Celedón, M.D., Dr.P.H., has seen many children with asthma as a physician and now as the chief of service in the Division of Pediatric Pulmonary Medicine at UPMC Childrenâs Hospital of Pittsburgh. He also shares a connection with the study population, saying, âI am quite passionate about health disparities research because of my Latino background.â
Genetic Epidemiology Of Asthma
Looking at the population gives clues about asthma being a heritable trait. First, there are large geographic and racial differences in disease occurrence. For example, the prevalence of asthma in many Western populations is high, up to 20%, whereas populations from the developing world exhibit much smaller prevalence rates, some as low as 1% or even lower . This is only indicative of a genetic causation in asthma, as different populations also have very different environmental circumstances. Second, offspring of asthmatic parents are at increased risk of asthma . The recurrence risk of asthma in children with one affected parent is around 25%, whereas the risk if both parents are affected is around 50%. Twin studies also support asthma being much more likely to occur in an individual if that individual has a genetically close relative with the disease. For instance, the recurrence risk of asthma in monozygotic twins is much higher than in dizygotic twins, highlighting the role of genetic risk factors in asthma . Nevertheless, the fact that the concordance for asthma in monozygotic twins is not 100% but around 75% points to environmental risk factors also playing an important role.
Read Also: How To Get Rid Of Asthma Without Inhaler
