Asthma And Copd Treatment In Dearborn Michigan
Dr. Sham Juratli is a family medicine physician that specializes in caring for adults with chronic respiratory diseases, including asthma and COPD. We help our patients achieve peak physical health and wellness through our various programs and services.
Find out how we can help you live a normal and healthy life. To request an appointment, call Dr. Juratlis clinic at 451-8253 or submit a request now. We look forward to serving you.
Know About Asthmatic Bronchitis
Asthma and bronchitis are defined as two inflammatory airway diseases. While they have distinct differences, as outlined above, asthma and acute bronchitis can occur together. This is known as asthmatic bronchitis.
A number of factors can contribute to asthmatic bronchitis. What triggers the symptoms in one person may be different than what causes a flare-up in another however, the following are the most common factors:
- Pollution
- Viral or bacterial infections
- Emotions
As you may have guessed, the symptoms of asthmatic bronchitis are a combination of asthma and bronchitis. They include shortness of breath, coughing, wheezing, tightness in chest and the production of phlegm.
Due to a virus or bacteria bronchitis can be contagious, however chronic asthmatic bronchitis is not contagious.
Respiratory diseases affect people of all ages- children, teens, adults and seniors. Most of these diseases, such as asthma, bronchitis and COPD, are chronic and all have a significant impact on the individual with the disease, as well as on family, the community and the health care system. Its in everyones interest to gain a better understanding of respiratory ailments, not only so current patients can breathe easier, but so that we can prevent future generations from suffering.
Related Reading:
Read Also: How To Prevent Asthma Attacks
Inflammatory Cells In Copd
Neutrophils are present in sputum of smokers but increased in COPD and related to disease severity. They may be important in mucus hypersecretion and through release of proteases. Macrophages: big numbers are in airway lumen, lung parenchyma, and bronchoalveolar lavage fluid. They produce increased inflammatory mediators and proteases and may show defective phagocytosis. T lymphocytes: both CD4+ and CD8+ cells are increased in the airway wall and lung parenchyma, with big CD8+/CD4+ ratio. Increased is the number of CD8+ T cells and Th1 cells which secrete interferon- and express the chemokine receptor CXCR3. CD8+ cells may be cytotoxic to alveolar cells. B lymphocytes: are increased in peripheral airways and within lymphoid follicles, possibly as a response to colonization and infection. Eosinophils: increased eosinophil proteins in sputum and eosinophils in airway wall during exacerbations. Epithelial cells: May be activated by cigarette smoke to produce inflammatory mediators .
Also Check: Do Chihuahuas Take Away Asthma
Is Asthma Or Copd Worse
Asthma and COPD are both dangerous in their own way.
A severe asthma attack can cause your airways to narrow so much that you are no longer able to breathe on your own. This happens when your short-acting inhaler is not effective enough. Youll need immediate treatment at the hospital. Without prompt treatment, a severe asthma attack can cause death.
COPD has more long-term consequences and is always progressive and is the leading cause of death in the U.S. But you can reduce exacerbations with treatment. Even though you can’t reverse the damage, you can slow the effects of damage and reduce the risk of death by quitting smoking and using oxygen therapy .
Very rarely, you may need lung transplantation, but this is a long process and a huge commitment for you and your family, so it is important that you discuss it with a pulmonologist at an appropriate transplant center.
Its important to know the early warning signs of COPD, so you can help slow the progression of the disease:
- Chronic cough
- Shortness of breath while doing everyday activities
- Frequent respiratory infections
- Fatigue
Result Of Physical Exam And Tests
The treatments for asthma and COPD are different. COPD treatment requires bronchodilators, and these should not be given to people with asthma. Asthma is often treated primarily with corticosteroids and the use of an inhaler. Asthma users also actively avoid triggers that induce asthmatic attacks. As such, an accurate diagnosis is critical in order to successfully manage your symptoms.
Diagnostic tests used to determine which of the two conditions you have include but are not limited to lung function tests, peak expiratory flow, spirometry, and pulse oximetry. Once you have an accurate diagnosis, you will work with a doctor to manage your condition. Asthma and COPD are lifelong conditions, so you will need to continuously work with medical professionals to help maintain a normal lifestyle.
You May Like: How To Get Rid Of Asthma Without Inhaler
Primary Outcome And Measurements
The primary outcome for this study was the proportion of patients with either asthma or COPD who had the other disease in the validated asthma and COPD populations. The presence of a diagnostic asthma Read code and positive reversibility tests supported an asthma diagnosis in the COPD population. The presence of a diagnostic COPD Read code, smoking history, and fixed airflow obstruction supported a current COPD diagnosis in the population with validated asthma. Spirometry measurements with at least one airflow measurement with forced expiratory volume in 1 second to forced vital capacity ratio â¤70% were considered as evidence for an obstructive airflow limitation. The quality of the spirometry procedure undertaken in UK primary care to diagnose COPD is high, as determined in a previous validation study.
Conversely, if the last COPD code was given > 2 years before the validation of an asthma diagnosis , the COPD might be misdiagnosed as the code was not repeated afterwards.
Asthma And Copd In The Elderly
The Global Initiative for Chronic Obstructive Lung Disease has defined COPD as a partially reversible or nonreversible airway limitation that is progressive and cannot be reversed by current therapies asthma, by contrast, is defined as a syndrome characterized by reversible airflow limitation .6,7 While there are prominent differences between COPD and asthma in older adults , they may become indistinct clinically in some elderly individuals.2
COPD is considered a systemic disease associated with extrapulmonary manifestations, including muscle wasting and systemic inflammatory response.2 It is important in the management of both disorders, however, to recognize the role of inflammation in the pathogenesis of asthma and COPD.2
Of note, although the incidence of upper airway obstruction in the elderly is unknown, it can mimic asthma and COPD therefore, special vigilance is necessary to diagnose upper airway obstruction in this patient population.2 Typical causes of upper airway obstruction include infection, malignancy, trauma, extrinsic compression and benign strictures secondary to airway interventions, which are becoming more prevalent.2
Don’t Miss: Ways To Help Asthma Without Inhaler
Who Can Get Asthma Or Copd
The most common risk factors for developing asthma is if you have a parent with asthma, or have had a severe respiratory infection as a child, or have an allergic condition, or have been exposed to certain chemical irritants or industrial dust in the workplace.
Risk factors for COPD include:
- Exposure to cigarette smoke
- Smokers with asthma
- Exposure to dust and chemicals at work
- COPD develops slowly over the years, so most people are at least 40 years old when symptoms begin
- A rare genetic disorder alpha-1-antitrypsin deficiency is the cause of some cases of COPD
What To Do To Overcome These Problems In Future
Our opinion is that asthma and COPD are obsolete terms that do not fully recognize the molecular and clinical heterogeneity of these pathological conditions. This heterogeneity indicates a wide range of disease mechanisms. Furthermore, as elegantly highlighted by Hizawa, asthma and COPD are not only heterogeneous diseases but also associated with complex medical conditions therefore, different molecular characteristics associated with different endotypes may occur in varying proportions in any given patient. For this reason, it would be useful to abandon both the Dutch and the British hypotheses in favor of the paradigm that diseases of airway obstruction are a collection of endotypes, driven by unique biological/genetic mechanisms.
Hizawa has also proposed that endotypes of asthma or COPD may be primarily characterized by increased susceptibility to type 2 inflammation, increased susceptibility to viral infections, bacterial colonization, or impaired lung development. This proposal could be an oversimplification, but at least it has the merit of inducing thought about asthma and COPD in a different way from the classic one.
Don’t Miss: Can Allergies Turn Into Asthma
Asthma Treatment Options& copd Treatment Options
In many cases, both lung diseases treatments are the same, such as Bronchodilators and inhalable steroids, but there are also a few treatment options that are specific to each condition.People with asthma may be encouraged to stay away from triggers or avoid going outdoors when pollen levels are high. In cases of people with severe asthma, a bronchial thermoplasty may be recommended. The procedure burns off some of the muscles in the airway, reducing their ability to constrict.
On the other hand, people with COPD may be encouraged to alter lifestyle habits, such as quitting smoking, to help prevent any further damage. They may also be prescribed oxygen or pulmonary rehabilitation. In severe cases of COPD, procedures like lung volume reduction surgeries and lung transplants may be suggested.
Both Asthma and COPD are treatable diseases that will require some lifestyle changes. Staying informed on your options and taking care of your health is very important in managing lung diseases. For any further questions about these conditions and their treatments, click the link below!
Copd Is Caused By Chronic Exposure To Noxious Chemicals
Day after day after day after day exposure to these noxious chemicals irritate airways. This initiates a response from the immune system. Mediators are released to get these chemicals out of the lungs. These “mediators” cause inflammation of airways and other lung tissue. This is what causes chronic bronchitis and emphysema. Unlike asthma, both of these diseases are progressive, meaning they may slowly get worse over time.
You May Like: How To Make A Homemade Inhaler For Asthma
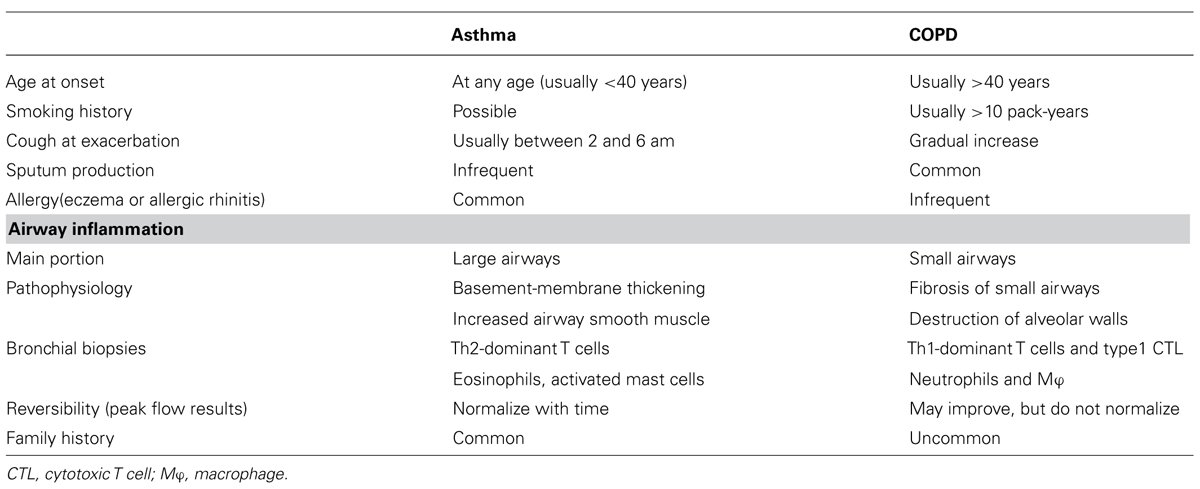
Patterns Of Airway Inflammation
The patterns of airway inflammation in asthma and COPD are markedly different. Asthma is characterized by mast-cell activation and infiltration of eosinophils, driven by activation of T-helper type 2 cells and type 2 innate lymphoid cells. In COPD, there is infiltration of neutrophils and macrophages driven by Th1, Th17, and CD8+ T cells, and typically no mast-cell activation, which accounts for the lack of reversibility. Nevertheless, eosinophil might play an important role in 10%40% of patients with COPD. Furthermore, patients with severe asthma may have prominent neutrophilia in biopsy specimens, although these patients are steroid-dependent and demonstrate more severe disease when compared to patients in whom bronchoalveolar lavage eosinophilia is evident.
There is no doubt that evaluation of bronchial biopsy specimens adds value to help differentiate asthma from COPD, but bronchial biopsy specimens are not a routine approach in everyday practice, and their use is limited. In any case, peripheral blood eosinophil count is a surrogate marker for airway eosinophilia in stable COPD, with a reasonable degree of accuracy.
Copd Vs Asthma: Which Is Worse
| | | | | | | | |
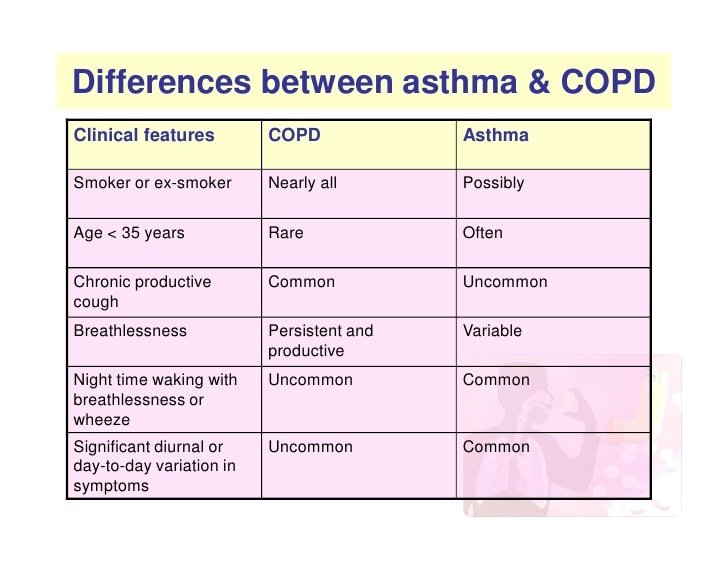
Asthma and chronic obstructive pulmonary disease are diseases of the lung that have a lot in common, but they also have key differences. Both conditions have similar symptoms caused by swelling of the airways or airway obstruction. Airflow limitation commonly results in breathing difficulties, coughing, wheezing, chest tightness, and shortness of breath.
Symptoms from asthma, triggered by allergens or exercise, come and go. COPD symptoms that can be caused by long-term smoking or prolonged exposure to chemical irritants are persistent. With COPD, chronic inflammation results in irreversible damage to the tissues lining the airways as well as pathological changes to the lung.
Though both diseases are chronic, COPD is a progressive condition, meaning symptoms are constant and the condition gets worse over time. With asthma, measures can be taken to control the disorder and when managed properly, its possible not to experience any symptoms for extended periods of time. Its important to distinguish COPD from asthma to determine the best course of treatment. Lets investigate the similarities and differences between asthma and COPD.
You May Like: Does Weight Gain Make Asthma Worse
Airway Hyperresponsiveness And Bronchial Reversibility
High degree of airway hyperresponsiveness in response to such stimuli as methacholine is usually associated with asthma, and remains a useful measure in distinguishing asthma from COPD. In COPD, airway hyperresponsiveness is typically limited to direct stimuli, such as histamine, suggesting that the airway response in this illness is largely determined by airway caliber, rather than an inflammatory bronchoconstriction. However, we have known for a long time that the presence of airway hyperresponsiveness, which is influenced by baseline lung function, is more common in smokers, with an association that becomes stronger with increasing age.
In any case, using reversibility as a key diagnostic criterion to distinguish between asthma and COPD is neither specific nor sensitive, also because in COPD the administration of high doses of bronchodilators has been associated with an unpredictable variability in airflow obstruction. While reversible airflow obstruction is the hallmark of asthma and mainly irreversible airflow obstruction the hallmark of COPD, many patients with asthma have persistent obstruction, while many with COPD have a reversible component. A 15% improvement in FEV1 used as the threshold to distinguish between asthma and COPD affords only 44% sensitivity for detecting asthma, and a quite modest 72% specificity in distinguishing asthma from COPD.
Airway Inflammation In Asthma
The airway inflammation in asthma is persistent even though symptoms are episodic, and the relationship between the severity of asthma and the intensity of inflammation is not clearly established .The inflammation affects all airways including in most patients the upper respiratory tract and nose but its physiological effects are most pronounced in medium sized bronchi . The pattern of inflammation in the airways appears to be similar in all clinical form of asthma, whether allergic, non-allergic, or aspirin-induced and at all ages .
Don’t Miss: How To Make A Homemade Inhaler For Asthma
Concerns Regarding Pharmacologic Therapy
Medication Delivery: In the elderly, it should be recognized that poor inhaler technique is common.2 One small study conducted by Allen et al assessed the metered-dose inhaler technique of 30 elderly patients .10 The researchers found that while 60% of participants were classified as competent, a mere 10% had an ideal technique 40% of participants were classified as incompetent. The most frequent error made was inadequate timing of actuation and inhalation.10 The study indicated competence was significantly related to mental status competence was not related to age, underlying diagnosis, or duration of MDI therapy.10 The researchers recommend that elderly patients requiring MDI therapy should be carefully selected and properly instructed by the prescribing physician. Patients were significantly more likely to be competent if they were first prescribed an MDI in a hospital, rather than prescribed an MDI by a general practitioner.10
Medication Effectiveness: Pharmacodynamic and pharmacokinetic differences, as compared with younger patients, may cause a diminished response to b2-agonists, while comorbidities, such as cardiovascular disease, may increase the risk for medication adverse effects.2
Medication Adherence: Factors leading to poor adherence to recommendations and inadequate response include: 1) complex medication regimens, 2) prohibitive cost, 3) cognitive impairment, and 4) poor medication delivery technique.2
Are Genetic Studies Helpful In Copd Phenotype Definitions
Genetic studies are a promising area of investigation in obstructive lung disease, both in COPD and asthma. But as Weiss writes, quoting Winston Churchill, It is not the beginning of the end, but it might be the end of the beginning. Both from a mechanism and clinical standpoint, other than the long-established information we have about alpha-1 antitrypsin deficiency and emphysema, this rapidly growing area is still in its early stage.
Don’t Miss: Can A Chihuahua Take Away Asthma
Airway Obstruction In Bronchitis
Asthma and chronic bronchitis are both obstructive lung diseases. Having an obstructive lung disease means that air has a hard time getting out of your lungs. An important difference between asthma and chronic bronchitis is whether medications can open up the airways .
In people with asthma, the airway obstruction is reversible. Their lung function improves after taking a bronchodilator medication, such as albuterol. People with COPD have irreversible airway obstruction. Their lung function does not improve after taking albuterol. Lung function is measured with spirometry.5
Is Air Flow Obstruction A Risk Factor For Lung Cancer
Cigarette smoking is the main risk factor for lung cancer, accounting for roughly 85% of cases. Multiple studies have suggested that air flow obstruction is a risk factor for lung cancer independent of smoking, but the role of radiographic evidence for emphysema is less clear. A recent study from the Mayo Clinic enrolled 1,520 patients who were followed for 4 years for the development of lung cancer . When analyzed as a continuous variable, reduced FEV1 and FEV1/FVC were associated with a subsequent diagnosis of lung cancer, with an odds ratio of 1.15 and 1.29 , respectively. When analyzed as a categorical variable, more severe air flow obstruction was associated with greater likelihood of lung cancer . There was no statistical association between percent volume of emphysema on chest CT scan and prevalent or incident lung cancer . Total lung volume measured on chest CT was significantly higher in patients with lung cancer than control subjects .
Presence of Air Flow Obstruction and Its Severity Predict Development of Lung Cancer Independent of Age, Smoking History, and Sex on Conditional Logistic Regression*
Read Also: What Do You Do When You Have An Asthma Attack
Recommended Reading: What Happens If You Smoke Weed With Asthma
How Doctors Differentiate The Two
Doctors can usually differentiate the two by asking you questions. Do you have a family history of asthma? COPD? Do you smoke? Did you have a job that exposed you to dust, fumes, or chemicals. When do you have symptoms? How often? They may also perform tests. The best test is a breathing test called a PFT. This is a test that measures your lung function. If lung function improves after using a bronchodilator, this usually indicates asthma.
What to make of this? There are certainly other differences, other than those listed here There are also asthmatics diagnosed with severe asthma. They may present similarly to COPD. There are also those who have a combination of both, Asthma-COPD Overlap Syndrome. There is also a lot more to learn about both.
