Factors That Influence The Accuracy Of Pulse Oximetry Readings
Overestimation of SaO2 is possible with bright sunlight on the probe, fluorescent lights, operating room lights, infrared heat lamps, elevated CoHb, elevated metHb, anemia, and motion artifact if the actual SaO2 is less than 85%.
Underestimation of SaO2 is possible because intravascular dyes, such as methylene blue and indocyanine green, produce transient reductions in SpO2. Fingernail polish, increased venous pressures, and motion artifact if the actual SaO2 is greater than 85% also can cause underestimation of the SaO2.
Mecholyl challenge, bronchial provocation test
An Approach To Interpreting Spirometry
TIMOTHY J. BARREIRO, D.O., and IRENE PERILLO, M.D., University of Rochester School of Medicine and Dentistry, Rochester, New York
Am Fam Physician. 2004 Mar 1 69:1107-1115.
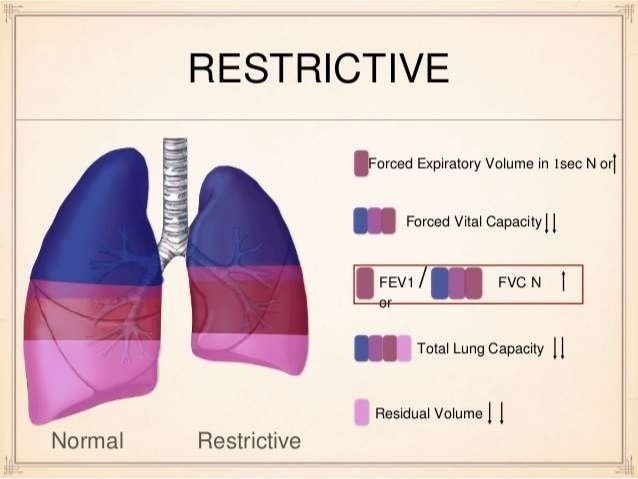
Spirometry is a powerful tool that can be used to detect, follow, and manage patients with lung disorders. Technology advancements have made spirometry much more reliable and relatively simple to incorporate into a routine office visit. However, interpreting spirometry results can be challenging because the quality of the test is largely dependent on patient effort and cooperation, and the interpreter’s knowledge of appropriate reference values. A simplified and stepwise method is key to interpreting spirometry. The first step is determining the validity of the test. Next, the determination of an obstructive or restrictive ventilatory patten is made. If a ventilatory pattern is identified, its severity is graded. In some patients, additional tests such as static lung volumes, diffusing capacity of the lung for carbon monoxide, and bronchodilator challenge testing are needed. These tests can further define lung processes but require more sophisticated equipment and expertise available only in a pulmonary function laboratory.
What Would A Larger Vital Capacity Indicate
Vital capacity is the maximum amount of air a person can expel from the lungs after a maximum inhalation. A persons vital capacity can be measured by a wet or regular spirometer. In combination with other physiological measurements, the vital capacity can help make a diagnosis of underlying lung disease.
You May Like: Propanolol Asthma
Is It Possible To Increase Vital Capacity
Another way to increase lung capacity is to improve exercise tolerance. Exercise causes your heart and breathing rates to increase, so your body has enough oxygen and strengthens your heart and lungs. The average persons lung capacity can be improved around 5 percent to 15 percent even with frequent workouts.
Airflow Lung Volumes And Flow
, MD, Grant Medical Center, Ohio Health
Airflow and lung volume measurements can be used to differentiate obstructive from restrictive pulmonary disorders, to characterize severity, and to measure responses to therapy. Measurements are typically reported as absolute flows and volumes and as percentages of predicted values using data derived from large populations of people presumed to have normal lung function. Variables used to predict normal values include age, sex, ethnicity, and height.
Read Also: What Is The Blood Test For Eosinophilic Asthma
Peak Expiratory Flow Rate
PEFR monitoring is a simple and costeffective means of determining the degree of airways obstruction. PEFR is a tool for monitoring patients with asthma, but it should not be used for the diagnosis of asthma. Patients with moderate or severe asthma should be instructed in the use of PEFR and have a peak flow meter accessible for selfmonitoring.
Patients should establish a baseline personal best PEFR. At a time when asthma symptoms are wellcontrolled, readings should be obtained at least twice daily over a 2 to 3week period, with one reading when the patient wakes up and another between noon and 2:00 pm. Readings should also be obtained pre and postbeta2 agonist use.
PEFR zones are defined by the EPR2 as follows:
-
Green Zone: > 80% of personal best peak flow. These readings represent good asthma control, and patients should continue taking their medications without change.
-
Yellow Zone: > 50%, but < 80% of personal best peak flow. Patients with readings in this range should exercise caution. A short-acting inhaled beta2 agonist should be taken immediately, and the patient should contact the physician regarding any potential changes to the asthma regimen.
-
Red Zone: < 50% of personal best peak flow. Patients should be on the alert, take their short-acting inhaled beta2 agonist, and contact their physician or the emergency department immediately. Patients may also go to their nearest emergency room.
Lung Volumes And Lung Capacities In Health And Respiratory Diseases
The changes in the volumes of the lungs occur in a predictable manner during quiet breathing and deep breathing. Four such measurable volumes have been described and based on the four volumes four capacities have been defined.
Tidal volume volume inhaled or exhaled during quiet breathing
Inspiratory Reserve Volume volume inhaled in excess of the TV in a deep inspiration
Expiratory Reserve Volume volume exhaled in excess of the TV and IRV in a deep expiration
Residual Volume volume that remains in the respiratory tract following a deep expiration
Inspiratory Capacity = TV + IRV
Vital Capacity = IRV + TV + ERV
Functional Residual Capacity = ERV + RV
Total Lung Capacity = IRV + TV + ERV + RV
Don’t Miss: Asthma Propranolol
Do Lung Volumes Tell Us Anything Meaningful About Obstruction
Residual volume upper limit of normal plotted as a percentage of the predicted value. Height and age of white subjects enrolled in the National Health and Nutrition Examination Survey III study were used to calculate the predicted RV and its upper limit of normal, using the European Community for Coal and Steel equations. All values fall above 120% of predicted, a value frequently used as the upper limit of normal when assessing air-trapping.
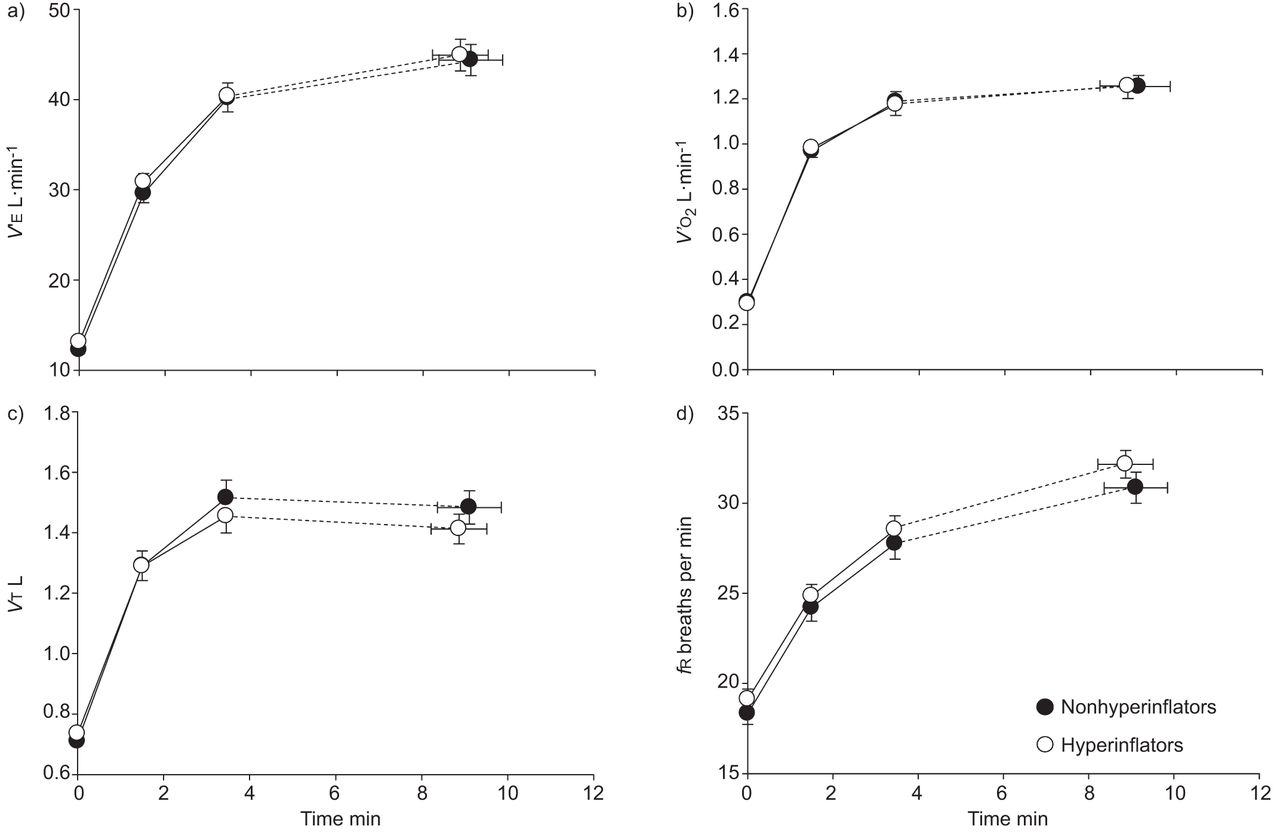
Dykstra and colleagues evaluated TLC, RV, and the RV/TLC ratio in a large group of patients with airway obstruction to see whether lung volumes could discriminate between asthma and COPD. They found that RV and RV/TLC were more sensitive than TLC to the degree of airway obstruction. As airway obstruction falls from mild to moderate , RV increases while TLC tends to remain the same. In general, lung volumes are not able to distinguish whether the increases are caused by COPD versus asthma, particularly when the diseases have progressed to moderate or severe airway obstruction. However, as shown in , there is a great deal of variability in RV/TLC, particularly around the LLN for FEV1. Although RV or RV/TLC may not help make a diagnosis as to whether the patient has asthma or COPD, it may be important to know how much hyperinflation is present if reducing it is a therapeutic goal.,
Is A Low Tlc A Useful Measurement
Aaron and colleagues demonstrated what might be considered intuitive regarding the relationship between FVC, RV, and TLC. They evaluated 470 patients who had restriction to assess whether a low FVC could be used to predict that restriction. When the FVC was within the normal range, the probability of a restrictive pattern was very low . If the FVC was reduced, the probability of a reduced RV was in the range of 5060%. In effect, a validly performed FVC excludes restriction if it is normal, but requires an additional evaluation if it is low. They also found that a low FVC accompanied by evidence of obstruction reduced the likelihood of restriction even further .
Probability of restrictive lung disease plotted against FVC for a large population of subjects referred for pulmonary function tests. As FVC falls the likelihood of restriction increases, but only to about 50%, and it differs depending on the degree of obstruction present.
Lung volume changes in obesity. Functional residual capacity and expiratory reserve volume % predicted plotted versus body mass index in 373 patients. Changes in each parameter are exponential , with the greatest change in the transition between overweight and obese .
Read Also: How To Get Rid Of Asthma Without Inhaler
Lung Volumes Depend On The Age Sex Ethnicity And Built
The lung capacities and volumes tend to increase as the size of the body increases and are higher in males compared to females. As the age increases after the third decade, the residual volume and the functional residual capacity increases due to the stiffening of the lungs as the elastic recoil forces tend to decrease with ageing. The tidal volume and the expiratory reserve volume decreases but the total lung capacity remains relatively constant.
Alcohol Effects On Lungs
Heavy alcohol use can cause damage to the lungs in a few different ways. It can interfere with the immune system that keeps the lungs healthy and able to fight off infections. It can also harm the surface cells that line the insides of the lungs.
Every day, a person inhales things in the air from which the lungs and immune system try to protect them. Parts of the lungs are even lined with moving, hair-like cells called cilia whose job it is to sweep things inhaled out of the lungs. Heavy alcohol> use harms this whole process.
Alcohols damage to lung cells and the immune system is so well known that it is a syndrome termed alcoholic lung. One study showed that chronic alcohol use can start to harm the lungs in as little as six weeks.
Alcohol abuse can also cause inflammation and harm cells in both the upper and lower parts of the airway. Its not the alcohol in its liquid form that does this, it is actually the vapor. Alcohol, after all, is an irritating chemical.
After a person drinks alcohol, besides going into the bloodstream, some of it will diffuse out into the lungs and end up in the breath. Breathalyzer tests work because the alcohol is partly breathed out in vapor form. But when it is in vapor form, then it is free to cause damage to the airway. This damage happens not only in the lungs but also in the nasal passages and sinuses, causing inflammation and making them less able to fight off infection.
Also Check: Can You Enter The Military With Asthma
Don’t Miss: Can I Join The Marines With Asthma
Global Alliance Against Chronic Respiratory Diseases
The Global Alliance against Chronic Respiratory Diseases contributes to WHOs work to prevent and control chronic respiratory diseases. GARD is a voluntary alliance of national and international organizations and agencies from many countries committed to the vision of a world where all people breathe freely.
What Is An Asthma Action Plan
Your healthcare provider will work with you to develop an asthma action plan. This plan tells you how and when to use your medicines. It also tells you what to do if your asthma gets worse and when to seek emergency care. Understand the plan and ask your healthcare provider about anything you dont understand.
Also Check: What Is Exercise Induced Asthma
Also Check: Does Weight Gain Make Asthma Worse
How Do I Get Ready For Pulmonary Function Tests
Your healthcare provider will explain the procedure to you. Ask him or herany questions you have. You may be asked to sign a consent form that givespermission to do the procedure. Read the form carefully. Ask questions ifanything is not clear.
Tell your healthcare provider if you take any medicines. This includesprescriptions, over-the-counter medicines, vitamins, and herbalsupplements.
Make sure to:
-
Stop taking certain medicines before the procedure, if instructed by your healthcare provider
-
Stop smoking before the test, if instructed by your healthcare provider. Ask your provider how many hours before the test you should stop smoking.
-
Not eat a heavy meal before the test, if instructed by your healthcare provider
-
Follow any other instructions your healthcare provider gives you
Your height and weight will be recorded before the test. This is done sothat your results can be accurately calculated.
Reducing The Burden Of Asthma
Asthma cannot be cured, but good management with inhaled medications can control the disease and enable people with asthma to enjoy a normal, active life.
There are two main types of inhaler:
- bronchodilators , that open the air passages and relieve symptoms and
- steroids , that reduce inflammation in the air passages. This improves asthma symptoms and reduces the risk of severe asthma attacks and death.
People with asthma may need to use their inhaler every day. Their treatment will depend on the frequency of symptoms and the different types of inhalers available.
It can be difficult to coordinate breathing using an inhaler especially for children and during emergency situations. Using a spacer device makes it easier to use an aerosol inhaler and helps the medicine to reach the lungs more effectively. A spacer is a plastic container with a mouthpiece or mask at one end, and a hole for the inhaler in the other. A homemade spacer, made from a 500-ml plastic bottle, can be as effective as a commercially-manufactured inhaler.
Access to inhalers is a problem in many countries. In 2019, only half of people with asthma had access to a bronchodilator and less than one in five had access to a steroid inhaler in public primary health-care facilities in low-income countries .
Read Also: Ibuprofen And Asthma Warning
Signs You Actually Have Severe Asthma
Breathing is just one of those things you take for granted until it feels like every inhale or exhale is a struggle. Unfortunately, people with severe asthma have to deal with breathing issues way more often than anyone should, and it can be completely terrifying.
Asthma is a respiratory condition that affects the airways that extend from your nose and mouth to your lungs, according to the National Heart, Lung, and Blood Institute . When youre exposed to triggers like animal fur, pollen, mold, exercise, and respiratory infections, these airways can narrow, restricting your airflow. This can then make the muscles surrounding your airways constrict, making it even harder to breathe, and cause your airways to produce more mucus than normal, further compounding the problem. All together, this can lead to asthma symptoms like shortness of breath, coughing, wheezing , and chest tightness or pain, according to the NHLBI.
Like most health conditions, asthma severity runs along a spectrum, Emily Pennington, M.D., a pulmonologist at the Cleveland Clinic, tells SELF. Some people have cases where they experience minor symptoms here and there . Others can have asthma that is basically an ever-present problem and might result in scary asthma attacks, which is when symptoms ramp up in severity and can even become life-threatening.
Related:
Also Check: What Kind Of Specialist Treats Asthma
Measurement Of Peripheral Lung Function
A number of studies have directly demonstrated the involvement of the lung periphery in asthma. In 1989, Wagner and coworkers published an investigation that employed the wedged bronchoscope technique to assess peripheral airflow resistance in normal subjects and in subjects with asthma, and reported two important findings. First, the magnitude of Rp in subjects with asthma was about an order of magnitude larger than in normal subjects, despite the fact that FEV1 in the subjects with asthma was within normal limits saliently illustrating the insensitivity of the FEV1 to peripheral lung dysfunction. Second, Rp was significantly correlated to AHR as measured by the PC20. We have subsequently extended this line of investigation , and found Rp to be increased by installation of cold dry air. We also found Rp to be highly variable, very unstable, and correlated to AHR. Even traditional measures of overall lung function implicate the critical role of the lung periphery in asthma. For example, dry gas hypernea increases residual volume and alters the quasi-static pressurevolume behavior of the lung, only during inspiration .
Recommended Reading: What Is The Blood Test For Eosinophilic Asthma
Bronchial Asthma: A Complex Disease
Bronchial asthma is a chronic disease characterized by airway hyperresponsiveness to a series of allergens or irritants. Coexistence of airway inflammation and remodelling has led to the hypothesis that the disease is inflammatory in nature, although the relationship between the inflammatory process and AHR has not been consistently shown. For example, studies examined by Brusasco etâal. revealed that markers of inflammation correlated with AHR in no more than 50% of the cases. In addition, pharmacological interventions have shown that inflammation can be modified independently of AHR and vice versa. It is significant that, despite a multitude of studies on cellular and molecular lung biology and immunology, the precise pathogenesis of asthma still remains unknown. In this review, we examine the disease from a different perspective. Specifically, we suggest that the pathogenesis of asthma can be better understood if we start from the principle that the lung is a complex organ and any chronic disease affecting it will also become complex.
What Happens During Pulmonary Function Tests
You may have your procedure as an outpatient. This means you go home thesame day. Or it may be done as part of a longer stay in the hospital. Theway the procedure is done may vary. It depends on your condition and yourhealthcare provider’s methods. In most cases, the procedure will followthis process:
Youll be asked to loosen tight clothing, jewelry, or other things that may cause a problem with the procedure.
If you wear dentures, you will need to wear them during the procedure.
Youll need to empty your bladder before the procedure.
Youll sit in a chair. A soft clip will be put on your nose. This is so all of your breathing is done through your mouth, not your nose.
Youll be given a sterile mouthpiece that is attached to a spirometer.
Youll form a tight seal over the mouthpiece with your mouth. Youll be instructed to inhale and exhale in different ways.
You will be watched carefully during the procedure for dizziness, trouble breathing, or other problems.
You may be given a bronchodilator after certain tests. The tests will then be repeated several minutes later, after the bronchodilator has taken effect.
Recommended Reading: Asthma Nebulizer Medication Names
