The Treatment Of Asthma: Where Are We Evolution Of A Concept
Asthma control medications reduce airway inflammation and help to prevent asthma symptoms among these, inhaled corticosteroids are the mainstay in the treatment of asthma, whereas quick-relief or rescue medicines quickly ease symptoms that may arise acutely. Among these, short-acting beta-agonists rapidly reduce airway bronchoconstriction .
National and international guidelines have recommended SABAs as first-line treatment for patients with mild asthma, since the Global Initiative for Asthma guidelines were first published in 1995, adopting an approach aimed to control the symptoms rather than the underlying condition a SABA has been the recommended rescue medication for rapid symptom relief. This approach stems from the dated idea that asthma symptoms are related to bronchial smooth muscle contraction rather than a condition concomitantly caused by airway inflammation. In 2019, the GINA guidelines review introduced substantial changes overcoming some of the limitations and weaknesses of the previously proposed stepwise approach to adjusting asthma treatment for individual patients. The concept of an anti-inflammatory reliever has been adopted at all degrees of severity as a crucial component in the management of the disease, increasing the efficacy of the treatment while lowering SABA risks associated with patients tendency to rely or over-rely on the as-needed medication.
Fig. 1
Established Therapy And Its Further Development
The established treatment of asthma primarily comprises two classes of drug, bronchodilators and anti-inflammatory/immunosuppressive drugs. By far the most effective bronchodilators in asthma are 2adrenoceptoragonists. Inhaled short-acting 2adrenoceptoragonists or, less frequently, anticholinergic drugs are used either on an as required basis, prophylactically, i.e. prior to exercise, or as rescue medication. Anti-inflammatory glucocorticoids are primarily long-term medications and are aimed at the treatment of airway inflammation and responsiveness 3. In very selected cases, disodium cromoglycate and nedocromil are available as alternatives to treatment with very low doses of inhaled steroids. Because of their significant side-effects, systemic steroids are used exclusively for the treatment of severe asthma or asthma exacerbations against which other therapies exhibit insufficient effects.
Signs That You Need To Use Asthma First Aid
If you are experiencing any of the following signs, follow your asthma action plan. If you do not have an asthma action plan, or you are assisting someone who is experiencing an asthma attack, start asthma first aid. Do not wait until asthma is severe.
Mild to moderate asthma signs :
- able to talk in full sentences
- able to walk or move around
- may have a cough or wheeze.
Severe asthma signs :
- cannot speak a full sentence in one breath
- tugging of the skin between ribs or at base of neck
- may have cough or wheeze
- reliever medication not lasting as long as usual.
Life-threatening asthma signs :
- getting little or no relief from reliever inhaler
- may no longer have wheeze or cough.
In asthma emergencies, follow your asthma action plan.
Don’t Miss: How Can Asthma Cause Death
The Present Treatment Of Asthma
The present treatment of asthma is based on guidelines from theBritish Thoracic Society,1-11 which advise starting patientswith mild asthma on agonists alone , with steroidsgiven only if there is poor control and too much bronchodilator isbeing used . Agonists are therefore widely regarded as thetreatment for asthma, with steroids as an optional extra. The evidenceshows that the reverse is true but it is difficult to convince patients of this in the face of the current guidelines, whichsupport the use of agonists as the drug of first choice. Thus manypatients who should be taking inhaled corticosteroids are receiving agonists only.1-12 Even when steroids are given the dose isoften insufficient to abolish symptoms due to bronchialhyperreactivity, and most patients are taking more agonists than isrealised.1-13
Peak flow rate readings show how initial dose of inhaled or oralcorticosteroids rapidly achieves optimum lung function in asthmaticpatients. Stepped care is less likely to achieve maximum possible peakflow rate
Management Of Patients Admitted To The Hospital: Wards And Icu Care
Careful consideration must be given to the level of care required when a patient with an exacerbation of asthma is admitted to the hospital. In general, guidelines suggest that patients should be admitted for observation and further treatment if the pretreatment FEV1 or PEF is < 25% of predicted or of personal best or if the post-treatment values are < 40% after emergency department treatment. Typically, patients who demonstrate a poor response to therapy , persistent or unresponsive hypercapnia, altered mental status, hypotension, or have significant comorbid conditions should be admitted to the ICU.
Although many patients maintain good oxygen saturations despite severe airway obstruction, some patients develop small airway mucus plugging even after the PEF/FEV1 normalize. Guidelines suggest that oxygen should be administered via nasal cannula or oronasal mask to maintain an arterial oxygen saturation of 9395% in adults and 9498% in children. In severe exacerbations, low-flow oxygen therapy by titrating the saturation to 9395% was associated with better physiological outcomes than with high-flow 100% oxygen therapy.
You May Like: Arizona Asthma And Allergy Institute Reviews
A Paradigm Shift In The Treatment Of Mild Asthma
Wei Tang1, Lin Sun1, J. Mark FizGerald2
1Department of Pulmonary Critical Care Medicine, Ruijin Hospital, Shanghai Jiaotong University school of Medicine ,
Correspondence to:
Submitted Sep 14, 2018. Accepted for publication Sep 26, 2018.
doi: 10.21037/jtd.2018.09.127
Mild asthma, often termed mild intermittent or mild persistent asthma, is defined by the Global Initiative in Asthma management strategy as patients who meet the criteria for step 1 and step 2 treatment strategies. Although these patients have fewer symptoms, they are the main and largest subgroup of asthma patients. Epidemiological data shows that mild asthma accounts for 70% of the total population of asthma patients, and a large proportion of them are newly diagnosed .
Although patients with mild asthma have fewer symptoms than patients with moderate or severe asthma, they also face ongoing chronic inflammation of the lower respiratory tract and the risk of acute exacerbations. According to epidemiological studies, among GINA grade 1 and grade 2 patients, 52.4% and 42.3% of them were uncontrolled . In addition, up to 25% of patients with mild asthma experienced a severe asthma exacerbation in the previous year . All of these data suggest that there are still a lot of unmet needs in the treatment of mild asthma.
A New Approach To The Treatment Of Asthma
It should be clearly stated that steroids are the proper treatmentfor asthma and that bronchodilators must be held in reserve foremergencies. All newly diagnosed asthmatics should be given a high doseof inhaled corticosteroids,1-11 continued for 3 months,after which the dose should be gradually reduced to a point wheresymptoms are controlled and maximum lung function maintained with theminimum dose. Unless there is an emergency agonists should not begiven initially but kept in reserve as rescue drugs.
A satisfactory response over a few days will show the effectiveness ofsteroids, gain the patient’s confidence, and ensure compliance. Thisalso acts as a reversibility test to find the maximum possible peakflow rate , which can be used as the target forfuture control. This procedure allows better lung function to beachieved than when gradual increments in drugs are used, as in steppedcare starting with agonists .
The difficulty in assessing the severity of symptoms, in order todecide on treatment, is avoided as all patients receive inhaledcorticosteroids as soon as the diagnosis of asthma isconfirmed.George Strube
Read Also: What Changes Inside The Airways Leads To An Asthma Attack
Increasing Your Treatment Dose
Your GP will probably try you on an add-on treatment before increasing the dose in your usual preventer medicine. This is so you can continue on a low dose of steroid medicine and avoid side effects.
They may consider trying a different inhaler device that may be easier for you to use, before increasing the dose.
If youre still having symptoms, even though youre taking add-on treatments or have tried a new inhaler device, your GP may consider increasing the dose of your preventer. They would start with an increase from a low to a medium dose.
Whenever your medicines change you should have another appointment with your GP or asthma nurse within four to eight weeks, either in the surgery or over the phone, to see if the change is working well for you.
Ask your GP or asthma nurse to update your asthma action plan with any changes to your medicines.
Treatment Of Acute Asthma Exacerbations
, DO, Wake Forest Baptist Health
The goal of asthma exacerbation treatment is to relieve symptoms and return patients to their best lung function. Treatment includes
Corticosteroids Leukotriene modifiers Mast cell… read more .)
Patients having an asthma exacerbation are instructed to self-administer 2 to 4 puffs of inhaled albuterol or a similar short-acting beta agonist up to 3 times spaced 20 minutes apart for an acute exacerbation and to measure peak expiratory flow if possible. When these short-acting rescue drugs are effective , the acute exacerbation may be managed in the outpatient setting. Patients who do not respond, have severe symptoms, or have a PEF persistently & lt 80% should follow a treatment management program outlined by the physician or should go to the emergency department .
Also Check: What Does Asthma Do To The Body
Therapy In The Emergency Department
Patients with mild-to-moderate asthma exacerbations may present to the emergency department to seek medical care. These patients should be treated as an out-patient when following the recommendation detailed above. Patients with severe or life-threatening asthma should always be managed in the emergency department. A focused, expedited history and physical examination should be carried out in all patients. It is critical to rule out other conditions that may mimic a severe asthma exacerbation, such as pneumonia, congestive heart failure, pneumothorax, and myocardial infarction. In patients with a severe exacerbation, careful attention should be placed on the level of consciousness, oxygen saturation, breathing frequency, resting pulse, and blood pressure, and on the use of accessory respiratory muscles. Patients with severe asthma may have a fast deterioration of their clinical presentation, so continuous monitoring of these patients is warranted. In the advanced stages of an asthma exacerbation, the pulmonary physical examination may reveal a silent chest, which may herald impending respiratory failure. Patients with severe asthma should also be monitored for potential complications of asthma, such as pneumothorax, pneumomediastinum, and anaphylaxis.
Unproved Alternate Therapy In Status Asthmaticus
Although the application of noninvasive ventilation has proved to be safe and effective in COPD, the use of NIV in severe asthma is not clearly defined. A systematic review found 5 studies with > 200 subjects with severe asthma randomized to NIV or placebo. Two of the studies found no difference in the number of subjects who required intubation and mechanical ventilation , whereas one study demonstrated fewer admissions in the NIV group. NIV should not be attempted in patients who are agitated or uncooperative, and patients should be monitored closely if NIV is attempted. Although retrospective studies are encouraging about the potential benefits of NIV, in our experience, many patients with acute, severe asthma are unable to tolerate NIV.,
Although intravenous aminophylline is not likely to result in any additional bronchodilation when compared with standard care with inhaled bronchodilators and corticosteroids, some patients with near-fatal asthma may gain benefit with intravenous aminophylline. The usual loading dose of 5 mg/kg is given intravenously over 20 min and then infused at a rate of 0.50.7 mg/kg/h. Such patients are rare, and the potential adverse effects are not uncommon . Blood levels should be checked daily for all patients receiving aminophylline infusions.
Recommended Reading: Is Asthma Restrictive Or Obstructive
What Causes A Drug To Change First
Or what causes first-line medicines to become the second-line? What causes second-line drugs to become first-line? Once again, Im going to make an educated guess here.
- Studies show its not as beneficial as once thought. Muscarinics are a good example here. Atrovent was once-upon-a-time considered a first-line asthma medicine. It fit all the qualifications of one. But, subsequent studies did not show it benefited most asthmatics. Studies do show, however, that it does help most COPDers. So, it remains a first-line treatment for COPD. Likewise, because it may help some asthmatics, it remains a second-line option here.
- Researchers learn more. Back in the 1970s, doctors were leary that inhaled corticosteroids may cause the same side effects as systemic corticosteroids. After studying this hard, researchers learned ICS are safe and effective for controlling asthma. This moved ICS out of second-line into the first-line status.
- Better, stronger, safer medicinal options become available. A good example here is theophylline. It was a first-line asthma medicine during the 1970s and 80s. It opened airways and kept them open. But, it also had some unwanted side effects, such as it kept you awake, like coffee does. The advent of combination inhalers like Advair made it so most asthmatics could be weaned off theophylline. This helped to relegate Advair to first-line status. But, it moved theophylline from first-line to second-line drug status.
Can Medicine Alone Help My Asthma
Not usually. Although medicines help a lot, they may not be able to do the job alone. You have to avoid the things that cause or trigger your asthma symptoms as much as you can. Asthma triggers can be found outside or inside your home, school, or workplace.
Improving the indoor air quality in your home is an important part of asthma control. Your indoor air can be more polluted than outside air. Our interactive Healthy Home can show you ways to improve the indoor air quality of your home. A healthier home can reduce your exposure to allergens and irritants.
Read Also: Can Change In Weather Trigger Asthma
Asthma Symptoms In A Severe Allergic Reaction
People having a severe allergic reaction can also have asthma-like symptoms. If the person has an anaphylaxis action plan, follow the instructions.
Always give adrenaline injector first, then asthma reliever if someone with known asthma and allergy to food, insects or medication has sudden breathing difficulty even if there are no skin symptoms. In case of an emergency, call triple zero and ask for an ambulance.
Leukotriene Receptor Antagonists And Synthase Inhibitors
Leukotrienes and histamine are the most important mediators in allergic asthma 32, and are released after contact with allergen from mast cells, eosinophils and basophils. Although antihistamines have no proven and documented effect in asthma, antileukotrienes have been developed that inhibit either the synthesis of leukotrienes or the interaction of leukotrienes with their receptors. To date, three drugs from this class of anti-leukotrienes that have been approved for the combination with inhaled steroids in different parts of the world, the leukotriene receptor antagonists, montelukast, zafirlukast and pranlukast 33. In clinical studies, montelukast was shown to reduce allergen- and exercise-induced bronchoconstriction. Other studies demonstrated that inhibition of the leukotriene pathway might decrease asthma symptoms, increase lung function and reduce the use of rescue medication 34. However, only a certain subgroup of patients, including some patients with severe asthma, appear to respond to treatment with antileukotrienes. Although it has been indicated that patients with aspirin-induced asthma might benefit from this treatment 35, it is, unfortunately, not possible to identify the subgroup in advance.
Don’t Miss: Can You Be In The Fbi With Asthma
The 2019 Gina Guidelines For Asthma Treatment In Adults
Emily L. Fedor, BS Pharmacy Studies, PharmD Candidate 2021Western New England University College of Pharmacy & Health SciencesWestern New England University College of Pharmacy & Health SciencesVictoria L. Freniere, BS Pharmacy Studies, PharmD Candidate 2021Western New England University College of Pharmacy & Health SciencesJared Ostroff, PharmD, BCACP, BCGPAmbulatory Pharmacy Anticoagulation CoordinatorClinical Associate ProfessorWestern New England University College of Pharmacy & Health SciencesSpringfield, Massachusetts
US Pharm. 2020 45:18-24.
ABSTRACT: Establishing asthma symptom control using pharmacologic and nonpharmacologic interventions improves quality of life and prevents exacerbations in patients with asthma. The Global Initiative for Asthma 2019 guidelines provide recommendations for asthma treatment organized into five steps that correlate with disease severity. Medication options include inhaled corticosteroids , long-acting beta2 agonists, short-acting beta2 agonists , leukotriene receptor antagonists, and oral corticosteroids. Recent data show unfavorable outcomes for SABAs used alone for as-needed treatment of symptoms of mild asthma. Guideline changes include the use of a low-dose ICS with formoterol for as-needed treatment in adults with mild asthma, or for use whenever a SABA would be used. Appropriate, effective medication regimens combined with counseling on proper inhaler technique will help patients achieve asthma-management goals.
Will Medicine Help Me Breathe Better When I Exercise
Yes. Exercising, particularly in cold air, may cause airway swelling or exercise-induced bronchoconstriction . Quick-relief asthma medicines, taken before exercise, usually control this. If you need repeated doses of quick-relief medicine during and after exercise talk with your doctor. Your medicines may need to be adjusted. Thanks to these medicines, many Olympic and professional athletes have successful sports careers even with their asthma.
It is important for everyone, including people with asthma, to be as active as possible for good health. Talk with your doctor about how you can be physically active while keeping your asthma well-controlled.
Also Check: How To Get Rid Of Asthma Completely
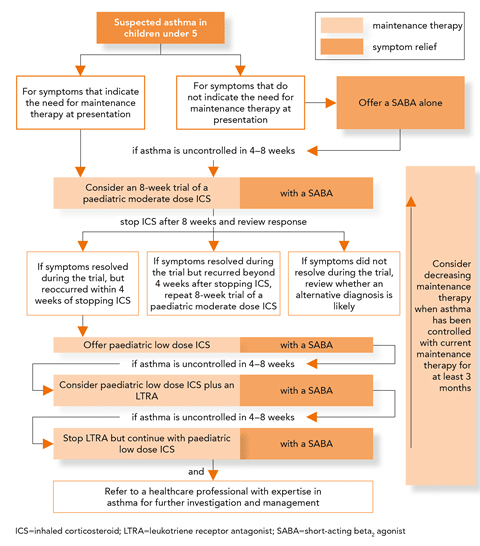
Figure : Stepwise Approach To Asthma Management For Children Ages 5
ICS=inhaled corticosteroids, LABA=long-acting beta agonists, LTRA=Leukotriene receptor antagonists, SABA=short-acting beta agonistsAdditional Figure 2 notes
- Every step: Reduce exposure to triggers, exercise, eat healthy, and manage stress
- Steps 2, 3, and 4: Consider immunotherapy for allergies
- Steps 5 and 6: Consider adding asthma biologics
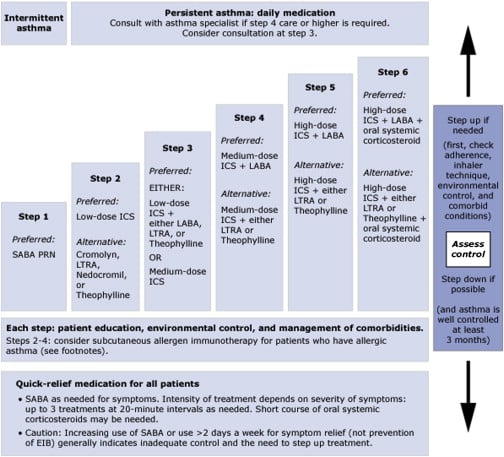
Figure : Stepwise Approach To Asthma Management For Adults And Children 12 Years And Up1
ICS=inhaled corticosteroids, LABA=long-acting beta agonists, LAMA=Long-acting muscarinic antagonists, LTRA=Leukotriene receptor antagonists, SABA=short-acting beta agonistsAdditional Figure 1 notes
- Every step: Reduce exposure to triggers, exercise, eat healthy, and manage stress
- Steps 2, 3, and 4: Consider immunotherapy for allergies
- Steps 5 and 6: Consider adding asthma biologics
Also Check: Can You Develop Asthma Later In Life
Can An Asthmatic Person Be Cured Of The Disease
Although asthma cannot be cured, proper management can control the disease and allow people to enjoy a good quality of life. Short-term medications are used to relieve symptoms.
What are the mechanisms and management of asthma exacerbations?
Mechanisms and management of asthma exacerbations Acute asthma remains a major medical emergency, the most common cause of acute hospitalizations in children and a major source of morbidity in adults with asthma. At all ages with asthma, the presence of exacerbations is an important determinant of asthma severity.
