Evaluating Asthma And Copd Symptoms And Causes
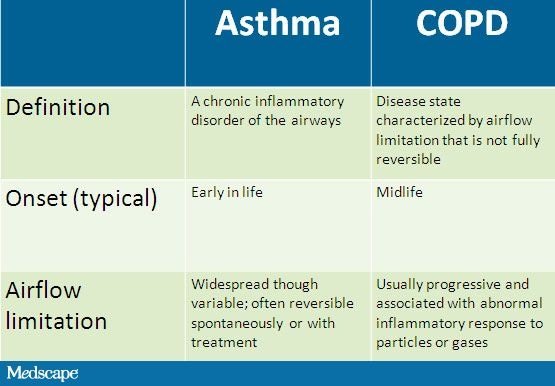
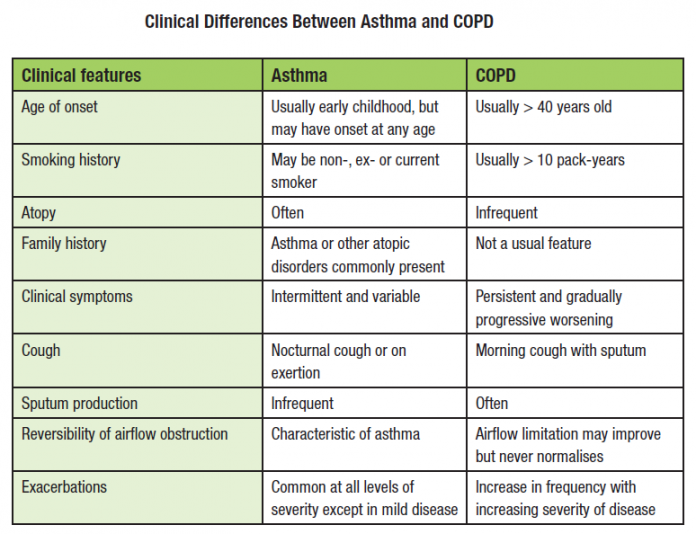
Because they are both lung diseases that inhibit regular breathing, asthma and COPD share many similarities in both symptoms and causes. The inflammatory immune reactions that cause an asthma attack are often triggered by airborne substances like smoke, dust, pollen, pet dander, mites and mold spores. COPD is caused by long-term exposure to lung irritants, such as cigarette smoke, toxic fumes and chemicals, which results in damaged lung cells.
While there are many external factors like tobacco smoke and secondhand smoke that can cause COPD or asthma, inherited genetic factors can also play a role in susceptibility to either of the diseases. For instance, alpha-1 antitrypsin deficiency is also referred to as inherited emphysema. Because of their similar causes and the way they affect the lungs, COPD symptoms can oftentimes look like an asthma attack and vice versa.
Here are the symptoms that may be found in both those with asthma and those with COPD:
Although the symptoms of COPD and asthma have a great amount of overlap and similarities, there are some subtle differences among them. For example, the chronic cough often experienced by those with COPD tends to produce far more phlegm and mucus than the amount produced by asthma. For this reason, a chronic cough is much more common in those with COPD than with asthma.
Staging And Treatment Of Chronic Obstructive Pulmonary Disease
The stages of COPD are defined primarily by lung function . This emphasises the important clinical message that the diagnosis of COPD requires the measurement of lung function. The stages of COPD suggested in the GOLD Guidelines are as follows. Stage 0: At risk, cough or sputum present but lung function normal. Stage 1: Mild COPD, FEV1/forced vital capacity < 70%, with an FEV1 â¥80% predicted, with or without chronic symptoms. Stage 2: Moderate COPD, FEV1/FVC < 70% and FEV1 % pred> 30% and < 80%. Stage 2 is split at an FEV1 of 50% pred since the existing data support the value of inhaled corticosteroids below an FEV1 of 50% pred but not above. Stage 3: Severe COPD, FEV1< 30% pred and FEV1/FVC < 70%.
In the GOLD guidelines, Stage 0 is a newly defined stage that was included to give a strong public health message that symptoms of chronic cough and sputum production should alert the clinician to the presence ofan ongoing pathophysiological process even when lung function is normal. This may progress to clinically significant COPD in a proportion of those exposed . The analogy that is perhaps most relevant is that mild hypertension in some but not all , with mild elevation of blood pressure will progress to clinically significant hypertension.
Airflow Restriction: Reversible Or Permanent
- Asthma treatment generally returns lung function to normal or near-normal and you should not have many asthma symptoms between asthma exacerbations. Airflow restriction in asthma is generally considered reversible, though some people who have severe asthma develop irreversible damage.
- Even with COPD treatment, airflow restriction and lung function will likely not return to normal or may only partially improveeven with smoking cessation and bronchodilator usage.
Recommended Reading: What Triggers And Asthma Attack
Chronic Bronchitis & Asthma
Chronic bronchitis is one of the lung diseases comprising chronic obstructive pulmonary disease , and theres also a link between this condition and asthma. Called asthma-COPD overlap syndrome , it is commonly described as persistent airflow limitation. While researchers are still learning about the cause and risk factors for ACOS, most agree that people with asthma who also smoke cigarettes are at greater risk of getting this condition. ACOS can lead to greater reduced lung function compared to those with only COPD as well as more frequent hospitalizations.
How Different Lung Diseases Affect The Lung
An analysis of how different lung diseases affect the lungs functionsThe lungs are essential respiratory organs in humans which enable us to breathe. Our lungs are specialised structures that allow us to exchange gases. We require oxygen from the air to enter our blood, as all cells need it to function. We also need to get rid of carbon dioxide which is a product of many metabolic reactions within our cells. Our lungs allow this gas exchange so we can get rid of carbon dioxide and acquire oxygen
Recommended Reading: Asthma Recurrence In Adults
Prevalence Of Asthma And Copd In The General Population Aged 2085 Years
There is a paucity of knowledge on the prevalence of asthma in the elderly, probably because asthma and COPD tend to overlap, making the diagnosis complex. , On the contrary, the large majority of epidemiological studies on COPD, which is usually assumed to be an aging disease, has been focused on elderly population and only few studies have been performed on young adult populations .
Our study is one of the few that reports the prevalence of both diseases in people aged from 20 to 84 years. It documents that asthma and COPD are major health problems, affecting about 13% of adults and 20% of the elderly. As people got older, the prevalence of asthma decreased , while the prevalence COPD increased . However, the prevalence of asthma and COPD remained non negligible even at the extremes of the age range. It is likely that this age-related pattern of asthma and COPD reflects both the true pattern of disease prevalence and the differential doctors diagnostic propensity according to the age of their patients . Indeed, distinguishing between asthma and COPD can be quite challenging, even for the most expert medical professional, and COPD is often misdiagnosed as asthma in young people, while the opposite happens in the elderly. This could explain in part our finding showing that the prevalence of asthma and/or COPD is invariant in the 2065 age range.
Airway Remodelling And The Overlap Syndrome
There is also increased airway wall remodelling in the overlap syndrome, with increased bronchial wall thickening on high resolution CT . Increased thickness of the airway wall is an important feature leading to airway obstruction in most airway diseases. In asthma, this is due to inflammation, subepithelial fibrosis and increased thickness of the smooth muscle. There is also increased thickness of the airway wall in COPD, which is not as prominent as in asthma, but involves the same structures of the epithelium, reticular basement membrane, airway smooth muscle and mucous glands. There is also evidence of remodelling, fibrosis and inflammation in these structures. The increased smooth muscle reported in COPD is seen in some but not all studies. Increased thickness of the airway epithelium and goblet cell hyperplasia are features of the remodelled airway in both asthma and COPD. Similarly, increased airway wall fibrosis is reported in both asthma and COPD. Thus when considering the pathological changes within the airways that are associated with asthma and COPD, there is similarity in terms of structures that are remodelled, but differences in the degree of changes in specific structures.
Recommended Reading: How To Cure Wheezing Permanently
What Is The Overlap Between Asthma And Copd
A patient who has features of more than one condition exhibits an overlap syndrome. The pathogenesis of overlapping asthma and COPD may be mediated by inflammatory/immune mechanisms and/or structural alterations. The clinical recognition of overlapping asthma and COPD requires an assessment of increased variability of airflow and incompletely reversible airflow obstruction. Numerous studies have documented the presence of partial reversibility after short-term and long-term bronchodilator administration in patients with COPD., Current guidelines emphasize a fixed or irreversible component to airway obstruction in some patients with asthma., Thus, the use of phenotypic characteristics may be useful in differentiating disease characteristics and in understanding similarities in the development and progression of both obstructive airway diseases. A recent study found that 17% to 19% of patients with obstructive airway diseases had more than one condition, or overlap. The overlap of asthma and COPD has been confirmed in older patients by objective testing and is becoming an important clinical consideration.
How Is Asthma Related To Chronic Obstructive Pulmonary Disease
- Date:
- University of Nottingham
- Summary:
- Two new studies exploring the causes and treatment of asthma and chronic obstructive pulmonary disease could lead to the development of drugs to battle these debilitating conditions.
Two University of Nottingham studies exploring the causes and treatment of asthma and Chronic Obstructive Pulmonary Disease could lead to the development of drugs to battle these debilitating conditions.
Though they are different diseases, asthma and COPD affect the human body in a similar way. In asthma, allergens irritate the lungs, in COPD, this is done by cigarette smoke. This irritation inflames the sufferers airways, which the muscles then close, creating a narrowing effect.
Research done at the University over the past 15 years has found that the muscle layer in the airway is more complex than has traditionally been thought. As well as going into spasm during asthma and COPD attacks the muscle layer produces a wide range of mediators and cytokines proteins that act as chemical signallers when it comes into contact with allergens or cigarette smoke. In asthma and COPD sufferers, these proteins are produced by stimulation of airway muscle cell walls in the lungs, releasing intracellular signalling proteins called transcription factors which alter the DNA of the cell and activate messenger RNA. It is these transcription factors which activate the inflammation by causing release of mediators and cytokines.
Story Source:
Also Check: Can Weed Affect Asthma
What Are Symptoms Of Emphysema
Symptoms of emphysema may include coughing, wheezing, shortness of breath, chest tightness, and an increased production of mucus. Often times, symptoms may not be noticed until 50 percent or more of the lung tissue has been destroyed. Until then, the only symptoms may be a gradual development of shortness of breath and tiredness , which can be mistaken for other illnesses. People who develop emphysema have an increased risk of pneumonia, bronchitis, and other lung infections. See your doctor if any of these symptoms arise:
- Shortness of breath, especially during light exercise or climbing steps
- Ongoing feeling of not being able to get enough air
- Long-term cough or smokers cough
- Wheezing
Q: How Can I Improve My Lung Health On My Own
No matter which lung condition you have, working closely with your healthcare team can control its effects on your everyday life. But there are other steps you can take as well. For instance, if you smoke, its never too late to quit. Make sure that youre current with all vaccinations, especially the pneumococcal and annual flu vaccine. These viruses can be very harmful to people with a lung disease. In addition, consider asking your provider about pulmonary rehabilitation if you have consistent breathing problems. This type of rehabilitation focuses on managing symptoms, exercising, and eating a nutritious diet.
Read Also: Can You Join The Marines If You Have Asthma
Asthma And Copd May Require Multiple Treatments
Dear Mayo Clinic:
I am an active 84-year-old man and was diagnosed with asthma and COPD a few years ago. My pulmonologist prescribed two medications Advair and Spiriva that seem to do the same thing. Why would I need both medications and are there other options?
Answer:
The medications you mention include three drugs because Advair contains two different medications. Spiriva is approved for treating chronic obstructive pulmonary disease . Advair is approved for both asthma and COPD. For people with moderate to severe COPD, research has shown a number of benefits with triple therapy like yours.
COPD is a lung disease that blocks airflow and makes breathing difficult. In most cases, the lung damage that leads to COPD is caused by cigarette smoking. But other irritants can cause COPD, too, including cigar or pipe smoke, air pollution and certain occupational exposures. In some cases, COPD results from a genetic disorder that causes low levels of a protective protein called alpha-1-antitrypsin.
Asthma occurs when the airways in the lungs become inflamed and constricted. This may be triggered by allergies or viral infections. During an asthma attack, the airways thicken due to inflammation, the muscles of the bronchial walls tighten, and the airways produce extra mucus that increases obstruction.
Paul D. Scanlon, M.D., Pulmonary and Critical Care Medicine, Mayo Clinic, Rochester, Minn.
Basis And Quality Of Data
Irritant-induced obstructive airways diseases cannot usually be diagnosed in one clinical visit and, instead, follow-up and/or detailed clinical investigations are necessary. The diagnostic gold standard for OA is SIC using a specific occupational agent in an exposure chamber. SIC is particularly indicated in the clinical setting where new causative substances with still unknown adverse respiratory sensitization potential are suspected. This gold standard is not applicable for large studies so, it was used mainly in case series or reports.The evidence levels to confirm irritant-induced work-relaated asthma or occupational COPD for the listed irritant agents, professions or worksites are frequently low with the major reasons being that high quality studies were missing and the quality of the available studies was low. Nevertheless, this knowledge is the best available and may help physicians to identify a suspected irritant agent as causative in irritant-induced work-related asthma and / or occupational COPD. As also recently stressed by Quint et al., implementing an evidence-based identification and regulatory process for OA will help to ensure primary prevention of OA. In cases of low evidence level of an agent that does not exclude a causative role, caution should be exercised and a more detailed diagnostic testing of relevant exposure should be performed.
You May Like: How To Get Rid Of Asthma Without Inhaler
Don’t Miss: Can You Join The Army If You Have Asthma
Accelerated Decline In Lung Function
Since COPD represents incomplete reversibility of airflow obstruction, then any risk factor that leads to accelerated loss of lung function will contribute to the development of COPD. Several risk factors for accelerated decline in include age, smoking, BHR, asthma and exacerbations or lower respiratory infections. Increasing age is associated with decline in lung function, both in asthma and in those without asthma.
Smoking
Loss of lung function is accelerated by smoking by up to 50 ml per year, and there is an established doseâresponse relationship. The loss of lung function with smoking may even be greater in those with asthma, such that smokers with asthma can develop COPD. Importantly, quitting smoking slows the decline in lung function. In the Lung Health Study, the annual decline in FEV1 in people who quit smoking at the beginning of the 11 year study was 30 ml/year for men and 22 ml/year for women. Continued smoking led to a decline in FEV1 of 66 ml/year in men and 52 ml/year in women.
Bronchial hyper-responsiveness
Asthma
The deficits in lung function in asthma seem to arise early in the course of the disease, and may be an effect of incomplete lung growth. In one study, abnormal lung function at age 26 in patients with asthma was related to male sex, BHR at age 9 years, early onset of asthma and reduced lung function by age 9 years.
Exacerbations
Knowing When To See A Professional
Clearly, there are numerous ways to effectively manage asthma and COPD, which means the prognosis for both diseases can be hopeful as long as each condition is caught early. While neither asthma nor COPD are considered curable, asthma is typically easier to control on a daily basis by avoiding triggers and taking the proper medication. As a progressive disease, COPD may get worse over time, but sticking with a physician-prescribed treatment plan can slow the disease’s progression and lessen symptoms.
The first step in successfully managing both conditions is to see a medical professional. Whether you suffer from difficulty breathing, coughing, wheezing or chest tightness or simply have a family history of the disease, you should consider seeking professional help. After consulting with a medical specialist, you will have a better idea of your condition and available treatment options.
It is especially important to receive medical attention specifically intended for your individual condition. Look for a rehabilitation center like Post Acute Medical that offers cardiopulmonary health services explicitly created to benefit asthma and COPD patients. At Post Acute Medical, there are precise treatment plans and therapies for a wide range of cardiopulmonary conditions, including COPD and asthma.
- Methods to maximize oxygen intake.
- Disease pathology.
- Infection control.
- Respiratory care.
Recommended Reading: Can You Join The Army If You Have Asthma
Distribution Of Symptoms Physical Limitation And Hospitalization According To The Diagnoses Of Asthma And Copd
Respiratory symptoms, physical limitation and hospitalization were statistically significantly increased in subjects with either doctor diagnosed asthma or COPD or both The risk of having respiratory symptoms or using medicines ranged from a minimum of 5-fold to a maximum of 200-fold with respect to subjects without a doctor diagnosis . Subjects reporting the diagnosis of the asthma-COPD overlap syndrome had the highest prevalence of all the respiratory symptoms/conditions considered, with the exception of allergic rhinitis and they differed significantly from the subjects with the diagnosis of asthma or COPD alone for the majority of symptoms investigated.
Lifestyle Factors For Copd
If you have COPD it can help to make a number of important lifestyle changes, including:
- quitting smoking techniques can include cold turkey, counselling, nicotine replacement therapy and medications that work on brain receptors. Evidence shows that counselling, together with medical therapy, is most effective
- being as physically active as possible. If possible, attend pulmonary rehabilitation
Also Check: Acetaminophen And Asthma
What Is The Prognosis And Life Expectancy For A Person Copd Vs Asthma
The prognosis for COPD ranges from fair to poor and depends on how rapidly COPD advances over time. In general, individuals with COPD have a decrease in their lifespan according to research.
If you have asthma, the prognosis for most people ranges from fair to excellent, depending upon how well you can identify what triggers your attacks, and your response to medication.
Dont Miss: Asthmatic Bronchitis Definition
