We Asked Allergists And Pulmonologists What Patients Need To Know About The Two Chronic Respiratory Diseases
Q: What are similarities and differences between asthma and chronic obstructive pulmonary disease ?
Asthma and COPD share similar symptoms persistent cough, wheezing, labored breathing during exercise, chest tightness and shortness of breath.
COPD involves several progressive lung diseases that develop over time, including emphysema and chronic bronchitis. Factors that point to a COPD diagnosis include:
- increased mucus or phlegm
- a greater frequency of respiratory tract infections
- history of smoking cigarettes
- exposure to secondhand smoke or environmental pollutants.
Most people with COPD develop symptoms after the age of 40 following years of exposure to lung irritation, particularly smoking. Other signs that could suggest COPD include fatigue, weight loss and morning headaches.
Q: Is one more common than the other?
Approximately 24 million people in the United States have asthma, including 6.2 million children, according to the Centers for Disease Control and Prevention .
More than 11 million Americans have COPD, but some 12-14 million more people may have the disease and not know it. COPD is sometimes misdiagnosed as asthma.
Q: Which is more serious?
Asthma and COPD are both serious, potentially life-threatening conditions. Both are treated with quick-relief inhalers for respiratory emergencies and daily controller medications that help keep airways open, reduce mucus and improve breathing.
Asthma
COPD
Q: Can asthma progress to COPD?
Reviewed by Purvi Parikh, MD
What Is The Difference Between Asthma And Copd
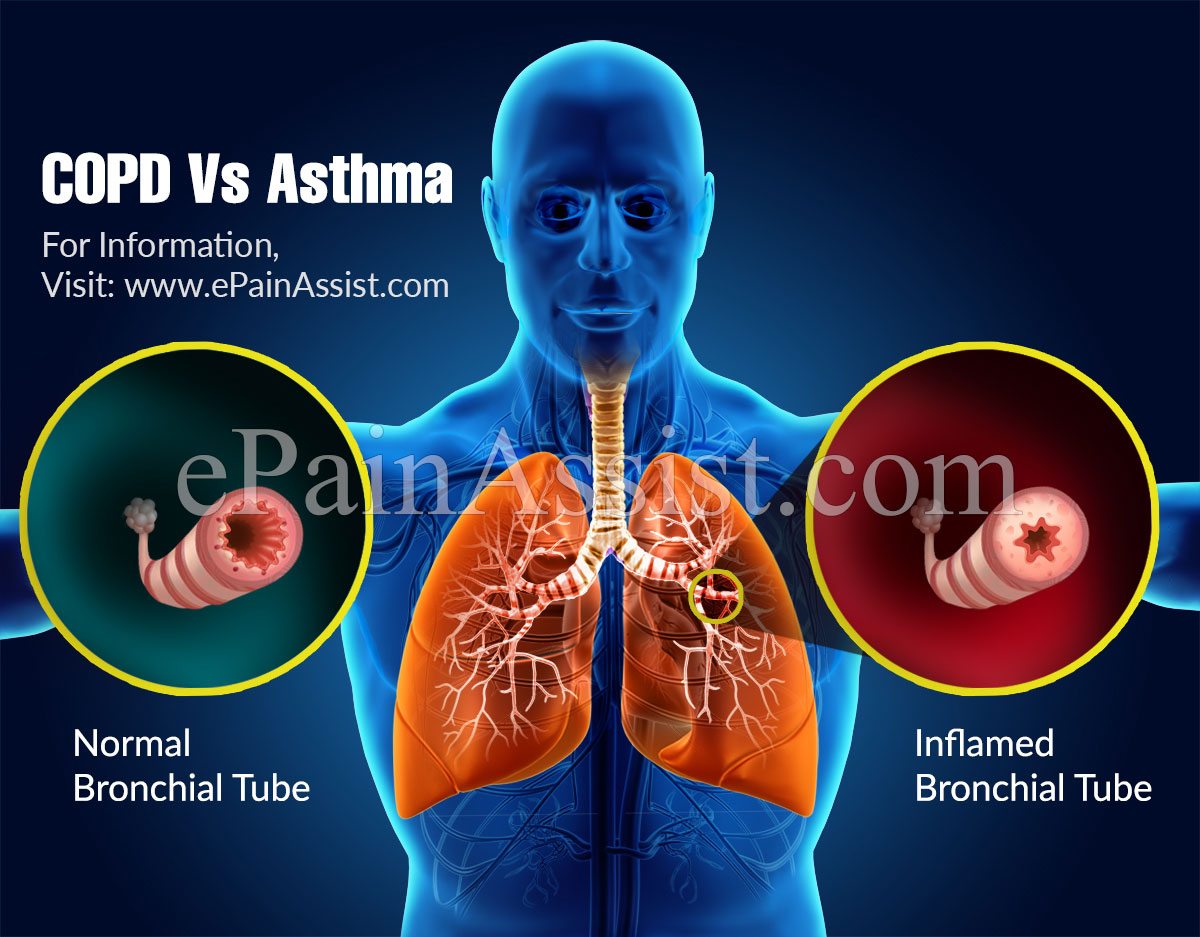
Asthma is a respiratory disease affecting the bronchial tubes, or airways, making them sensitive to allergens or irritants, both of which can bring on an asthma attack. During an asthma attack, it is hard to breathe, and wheezing, coughing, and chest tightness may occur. While COPD can also cause these symptoms, its more likely to experience a consistent cough with phlegm.
Unlike asthma, COPD is a chronic condition caused by damage to the lungs over time, most often from smoking, and it is irreversible. With asthma, breathing returns to normal after an attack, but COPD symptoms are more regular. Usually, COPD develops in people after age 40 and becomes a chronic disease of lung function while asthma may develop in people of almost any age.
Why Do Some Asthmatics Develop Copd
Researchers are still investigating this area. They are still not sure. But, one theory is the type of inflammation involved. Most asthmatics have inflammation caused by white blood cells called eosinophils. So, they have eosinophilic inflammation. This type of inflammation responds well to traditional asthma medicines.
Their asthma responds well to beta 2 adrenergics and corticosteroids. A daily dose of medicines like Advair or Symbicort help them obtain good asthma control.
When these medicines dont work, they may be diagnosed with Severe Asthma. The cause may be a different type of inflammation, such as neutrophilic inflammation. This is similar to the type of inflammation seen in COPD airways.
Plus, Severe Asthmatics may have airway scarring. Inflammation can cause damage to airway tissues. Tissues then become scarred. This scar tissue makes airway walls thicker. This also is similar to what happens with COPD.
Thicker walls make airways abnormally narrow. There is no medicine for treating this. And this may cause persistent airflow limitation. When this happens, a diagnosis of COPD can be made. It may result in a diagnosis of Asthma/ COPD Overlap Syndrome.
Recommended Reading: Does Weight Gain Make Asthma Worse
Whos Likely To Have Asthma Copd Or Aco
People who smoke or breathe in pollution or chemicals at work for many years have higher chances of having COPD. That’s why the condition often starts in middle age or later in life.
Asthma is sometimes caused by gene changes that are passed down through families. If one of your parents has the disease, you’re more likely to have it.
Symptoms of asthma often start in childhood, and the condition is one of the most widespread long-term illnesses in kids. It affects about 1 in 10 children.
Besides a family history of the condition, a few things can raise your chances of asthma:
- Smoking
- Being around chemicals or other irritants in the air
People who get ACO tend to be over 40 but younger than people with just COPD, and they have allergies .
Can Asthma Turn Into Copd
Allergies and breathing disorders can be some of the toughest conditions to navigate, especially since there is so much at stake. If you are suffering from asthma, emphysema, or COPD, you may be wondering if there are any links between these diseases.
Recent studies have compared links between asthma and COPD. If you are interested in a consultation or assessment to diagnose your own breathing conditions, please make an appointment for asthma treatment in Manhattan.
Read Also: How To Get Rid Of Asthma Without Inhaler
Exacerbation/infection: Changes In Inflammatory Features And Cytokine Profiles
Exacerbations of asthma and COPD are clinically significant events. They are frequently triggered by viral infections of the airways and are associated with a decline in lung function and symptomatic aggravation. During exacerbation, airway inflammation becomes more exaggerated than in the mild and stable disease states, and the inflammation pattern changes. Neutrophil recruitment is a prominent feature of acute exacerbation of chronic asthma, probably owing to respiratory tract infection by viruses., Furthermore, neutrophilic inflammation in the absence of eosinophils is largely present in sudden-onset fatal asthma, and neutrophil numbers are highly elevated in status asthmaticus., Thus, severe and fatal asthma may be mediated by neutrophils, which is quite different from the classical Th2-driven eosinophilic form of the disease. In COPD patients, an allergic profile of inflammation can occur, particularly during exacerbation. Airway eosinophilia is observed in chronic bronchitic patients with exacerbation and is associated with the upregulation of RANTES in the airway epithelium., Recently, Siva et al. demonstrated that the minimization of eosinophilic airway inflammation was associated with a reduction in severe COPD exacerbation. Taken together, these studies indicate that the inflammatory characteristics of asthma and COPD are interchangeable during exacerbation and infection.
What Is The Prognosis And Life Expectancy For A Person Copd Vs Asthma
The prognosis for COPD ranges from fair to poor and depends on how rapidly COPD advances over time. In general, individuals with COPD have a decrease in their lifespan according to research.
If you have asthma, the prognosis for most people ranges from fair to excellent, depending upon how well you can identify what triggers your attacks, and your response to medication.
Don’t Miss: Chihuahuas And Asthma
Does Asthma Worsen With Age
With age, the immune system’s response to inflammation becomes blunted, making it harder to fight off infections that can trigger asthma exacerbations. Other biological changes, notably shifts in patterns of inflammation, may reduce older patients’ response to inhaled corticosteroids that need to be taken daily.
Is Chronic Asthma The Same As Copd
Chronic asthma and COPD can have similar symptoms, but they are considered distinct conditions. COPD refers specifically to chronic bronchitis, emphysema or both.
Other differences include the fact that asthma tends to start during childhood, while COPD is more likely to appear among adults who smoke.
Recommended Reading: Asthma Attack With No Inhaler
Asthma May Raise Risk Of Copd Emphysema
Asthma Patients May Be Up to 17 Times More Likely to Develop Incurable Lung Diseases
July 12, 2004 — Adults with asthma may face dramatically higher risks of developing potentially deadly lung diseases later in life, according to a new study.
Researchers found asthmatic people were 12 times more likely to be diagnosed with chronic obstructive pulmonary disease than people without asthma.
COPD is a group of lung diseases for which there is no cure. COPD causes permanent damage to the lungs, making it difficult to breathe. It includes emphysema and chronic bronchitis.
According to the National Heart, Lung, and Blood Institute, it is the fourth leading cause of death in the U.S. and the world.
“Our study shows a strong link between asthma diagnosis and the development of COPD, which suggests they may share a common background,” says researcher Graciela E. Silva, MPH, of the University of Arizona’s College of Medicine in Tucson, in a news release. “It is possible that factors such as smoking and repeated episodes of acute bronchitis may facilitate the evolution of asthma into COPD, but the process by which asthma and COPD become comorbid conditions is not clear.”
More Than 40 Percent Of Women With Asthma May Develop Copd But Risk May Be Reduced
- Date:
- American Thoracic Society
- Summary:
- More than four in 10 women with asthma may go on to develop chronic obstructive pulmonary disease , according to a study conducted in Ontario, Canada.
More than 4 in 10 women with asthma may go on to develop chronic obstructive pulmonary disease , according to a study conducted in Ontario, Canada, and published online in the Annals of the American Thoracic Society.
In “Asthma and COPD Overlap in Women: Incidence and Risk Factors,” Teresa To, PhD, and coauthors report that of the 4,051 women with asthma included in their study, 1,701, or 42 percent, developed COPD. On average, the women were followed for about 14 years after being diagnosed with asthma.
The researchers examined risk factors for developing asthma and COPD overlap syndrome, known as ACOS. Those who develop ACOS experience increased exacerbations and hospitalizations and have a lower quality of life, compared to those who have asthma or COPD alone.
“Previous studies have found an alarming rise in ACOS in women in recent years and that the mortality rate from ACOS was higher in women than men,” said Dr. To, a professor in the Graduate School of Public Health at the University of Toronto in Canada. “We urgently need to identify and quantify risk factors associated with ACOS in women to improve their health and save lives.”
However, ACOS did not affect only those who smoke: 38 percent of the women who developed ACOS in the study had never smoked.
Story Source:
Read Also: Atopy And Asthma
Airflow Restriction: Reversible Or Permanent
- Asthma treatment generally returns lung function to normal or near-normal and you should not have many asthma symptoms between asthma exacerbations. Airflow restriction in asthma is generally considered reversible, though some people who have severe asthma develop irreversible damage.
- Even with COPD treatment, airflow restriction and lung function will likely not return to normal or may only partially improveeven with smoking cessation and bronchodilator usage.
Diagnosing Asthma And Copd With Pft
I explained how a PFT can help diagnose asthma in my post at Asthma.net: What Are PFTs? I explained how a PFT can hep diagnose COPD in my post on this site, What Are PFTs?
So, if you read those, you know what an FEV1 is. You know how this can be used to determine if you have COPD. Still, heres a quick review. You do a PFT. You do a pre and post FVC. A computer determines your FEV1. This is the best indicator of airflow limitation.
You then use a bronchodilator. This can be either an inhaler or breathing treatment. Then you do a second FVC. Heres how you determine if its asthma or COPD.
- COPD. By its basic definition, its persistent respiratory symptoms and airflow limitation. Your pre and post bronchodilator FEV1 is less than 80%. Your post bronchodilator FEV1 is not much different than your pre bronchodilator FEV1. This shows that airflow limitation is persistent. It is not reversed with time or treatment. This confirms a diagnosis of COPD.1
- Asthma. By its basic definition, respiratory symptoms and airflow limitation are intermittent and vary in intensity. Asthma attacks are reversible with time or treatment. Your post bronchodilator FEV1 improves by 12% or more. This shows airflow limitation is reversible. This can help make a diagnosis of asthma. 2
- Asthma and COPD. This is when you have both. Your airflow limitation is reversible. But, your FEV1 remains under 80% despite treatment.
You May Like: Natural Albuterol Substitute
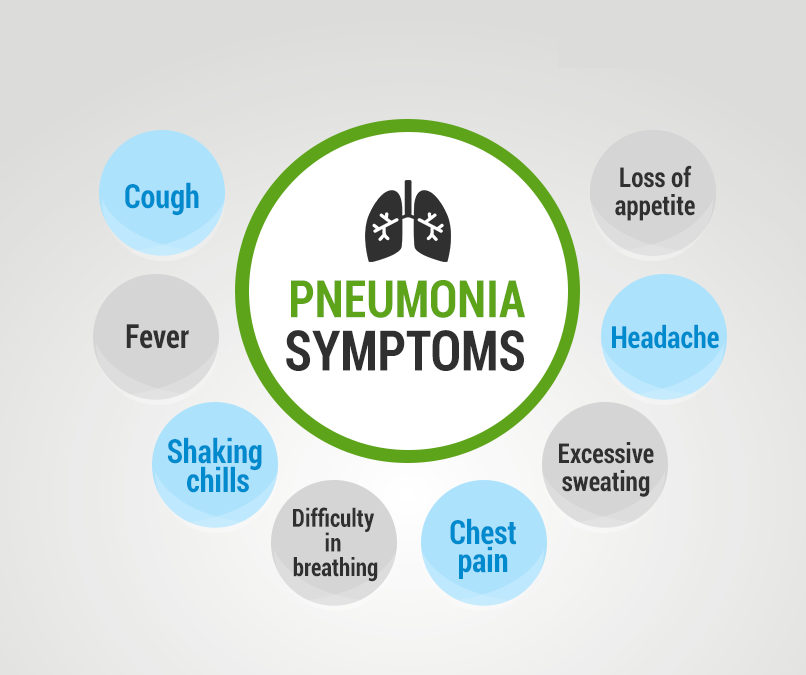
Q: How Can I Improve My Lung Health On My Own
No matter which lung condition you have, working closely with your healthcare team can control its effects on your everyday life. But there are other steps you can take as well. For instance, if you smoke, its never too late to quit. Make sure that youre current with all vaccinations, especially the pneumococcal and annual flu vaccine. These viruses can be very harmful to people with a lung disease. In addition, consider asking your provider about pulmonary rehabilitation if you have consistent breathing problems. This type of rehabilitation focuses on managing symptoms, exercising, and eating a nutritious diet.
Airway Inflammation In Asthma
The airway inflammation in asthma is persistent even though symptoms are episodic, and the relationship between the severity of asthma and the intensity of inflammation is not clearly established .The inflammation affects all airways including in most patients the upper respiratory tract and nose but its physiological effects are most pronounced in medium sized bronchi . The pattern of inflammation in the airways appears to be similar in all clinical form of asthma, whether allergic, non-allergic, or aspirin-induced and at all ages .
Read Also: Can Smoking Weed Cause Asthma
Asthma And Copd: What’s The Difference And Is There A Link
Asthma and chronic obstructive pulmonary disease are lung diseases. Both cause swelling in your airways that makes it hard to breathe.
With asthma, the swelling is often triggered by something youâre allergic to, like pollen or mold, or by physical activity. COPD is the name given to a group of lung diseases that include emphysema and chronic bronchitis.
Emphysema happens when the tiny sacs in your lungs are damaged. Chronic bronchitis is when the tubes that carry air to your lungs get inflamed. Smoking is the most common cause of those conditions .
Asthma gets better. Symptoms can come and go, and you may be symptom-free for a long time. With COPD, symptoms are constant and get worse over time, even with treatment.
Staging And Treatment Of Chronic Obstructive Pulmonary Disease
The stages of COPD are defined primarily by lung function . This emphasises the important clinical message that the diagnosis of COPD requires the measurement of lung function. The stages of COPD suggested in the GOLD Guidelines are as follows. Stage 0: At risk, cough or sputum present but lung function normal. Stage 1: Mild COPD, FEV1/forced vital capacity < 70%, with an FEV1 â¥80% predicted, with or without chronic symptoms. Stage 2: Moderate COPD, FEV1/FVC < 70% and FEV1 % pred> 30% and < 80%. Stage 2 is split at an FEV1 of 50% pred since the existing data support the value of inhaled corticosteroids below an FEV1 of 50% pred but not above. Stage 3: Severe COPD, FEV1< 30% pred and FEV1/FVC < 70%.
In the GOLD guidelines, Stage 0 is a newly defined stage that was included to give a strong public health message that symptoms of chronic cough and sputum production should alert the clinician to the presence ofan ongoing pathophysiological process even when lung function is normal. This may progress to clinically significant COPD in a proportion of those exposed . The analogy that is perhaps most relevant is that mild hypertension in some but not all , with mild elevation of blood pressure will progress to clinically significant hypertension.
You May Like: How To Make A Homemade Inhaler For Asthma
Differences Between Copd And Asthma
There are a number of other differences between COPD and asthma as well.
-
Often diagnosed during childhood or adolescence
-
Symptoms more likely to occur episodically and/or at night
-
Commonly triggered by allergens, cold air, exercise
-
People who have asthma are more commonly nonsmokers
-
Comorbid conditions include eczema and allergic rhinitis
-
Treatment usually involves inhaled steroids
-
Airflow restriction mostly reversible
-
Likely to cause morning cough, increased sputum, and persistent symptoms
-
Exacerbations commonly triggered by pneumonia and flu or pollutants
-
Most people who have COPD have smoked or had significant secondhand smoke exposure
-
Comorbid conditions include coronary heart disease or osteoporosis
-
Treatment usually involves pulmonary rehabilitation
-
Airflow restriction is permanent or only partially reversible
Once you develop COPD, your symptoms will generally be chronic. Over time, with COPD, you are likely to experience symptoms that are not typical for asthmalosing weight, decreased strength, and diminished endurance, functional capacity, and quality of life.
Why Is It Important
There are several reasons why the overlap syndrome is important. First, patients with overlapping asthma and COPD are excluded from clinical trials of treatment. This means that for an increasing proportion of older patients with obstructive lung disease, the data on efficacy of treatment may not be relevant. The clearest example of this comes from the studies on the efficacy of inhaled corticosteroids in asthma. These studies typically exclude smokers with asthma because of the difficulty in separating asthma from COPD in smokers with obstructive lung disease. However, up to 30% of people with asthma are smokers, and this means a substantial proportion of the population are excluded from randomised controlled trials. Extrapolation of the efficacy results for corticosteroids in non-smokers to smokers with asthma is flawed. Smokers with asthma have a relative corticosteroid resistance such that corticosteroids are much less efficacious in smokers with asthma than in non-smokers with asthma. This emphasises the need to study drug efficacy in relevant clinical populations, and the necessity to include overlap syndrome in drug evaluation programmes.
You May Like: How To Get Rid Of Asthma Without Inhaler
Can You Have Both Copd And Asthma
Yes, people can have symptoms of both COPD and asthma. Its called the asthma-COPD overlap syndrome. People with the overlap syndrome tend to be younger than those with COPD and older than those with asthma, and they have symptoms more often than people with COPD or asthma alone. When you have asthma for many years, it can also start to behave more like COPD than asthma. Sometimes the distinction can be hard to make.
