Nocturnal Asthma And Children
Asthma is more common in children than in adults and is the most common chronic disease in children worldwide. Accurately diagnosing and treating nocturnal asthma in children is especially important because the effects of nocturnal asthma, like loss of sleep and daytime sleepiness, are associated with behavioral and developmental difficulties.
Unfortunately, nocturnal asthma often goes undiagnosed in children because they tend to underestimate or not report their nighttime symptoms. For this reason, its helpful for parents to monitor and report back to the doctor any concerning symptoms in children. These symptoms may include wheezing, disturbed sleep, daytime sleepiness, and difficulties concentrating at school.
Breathing Disorders Linked Connections Between Sleep Apnea & Asthma
Its an unfortunate reality that most disorders out there have side effects that can put you at risk of developing further problems. This is especially true of Obstructive Sleep Apnea, or OSA. When left untreated, OSA is well known in the medical community for putting sufferers at risk of developing far more serious conditions from heart disease and heart attacks to strokes, Type II Diabetes, and even certain types of cancer.;
But while the cardiovascular and other physiological conditions I listed above are well known, some may be surprised to hear that OSA can actually be caused or exacerbated by the common respiratory problem known as asthma. Studies have shown that adults who already struggle with asthma are prone to an increased risk for developing OSA, especially if they have had asthma for a long period of time;
Asthma And Sleep Apnea: What Does Research Say
A study undertaken in Wisconsin examined the occurrence of sleep apnea in adult participants, over a period of 25 years, from 1988 till 2013. The study concluded that asthma was associated with an increased risk of sleep apnea. The symptoms of asthma, like nasal congestion, inflamed airway, and breathlessness, can aggravate sleep apnea. Another study has also proven that nocturnal symptoms occur in 60 to 74% of asthma patients. Sleep apnea is a common risk factor for asthma.
However, sleep apnea can also worsen symptoms of asthma during the day. A study mentions that the mechanisms which lead to worsening of asthma in patients of sleep apnea, include partial or complete airway obstruction. Also, sleep apnea often results in gastroesophageal acid reflux due to increased abdominal pressure. Sleep apnea is also associated with bronchial inflammation and hyperresponsiveness, which can trigger an asthma attack. Sleep apnea is also linked to cardiac dysfunction, increasing the risk of congestive heart failure which causes airway obstruction, resulting in asthma. There is increasing evidence that obesity may be a major risk factor for asthma, and many obese patients are likely to develop sleep apnea as well.
Recommended Reading: Cough Variant Asthma Mayo
Clinical Outcome Of Asthma
Not only does OSA seem to be associated with development of nocturnal asthma, it is also associated with persistent daytime asthma symptoms, particularly in those with severe and difficult-to-treat asthma. Thus, unrecognized OSA may be the cause of persistent daytime and nocturnal asthma .
There is still little evidence on the impact of OSA on asthmatic patients pulmonary function. Based on a 15-year follow-up study of ventilatory function in asthmatic patients, the unadjusted decline in forced expiratory volume in one second was 38 ml/year . There are several factors identified for the decline of FEV1 in asthma, including age, sex, asthma exacerbation, smoking status, obesity, and hypoxia . In a recent retrospective study, asthmatic patients with OSA were followed for more than 5 years with spirometry and showed a greater decline in FEV1 compared to those without OSA . In this study, the decline of FEV1 among asthmatic patients with severe OSA was 72.4 ml/year compared to 41.9 ml/year in those with mild to moderate OSA and 24.3 ml/year in those without OSA. After adjusting for confounder, OSA severity was the only independent factor affecting pulmonary function decline . However, in another recent meta-analysis, no significant difference of FEV1 was seen between asthmatic patients with and without OSA . Larger prospective studies are needed to verify long-term effects on pulmonary function.
Relationship Between Asthma And Obesity
Obesity represents a major risk factor and a disease modifier of asthma both in children and adults . It was found that obese subjects have increased risk of asthma and obese asthmatics have more symptoms, more frequent and severe exacerbations, a reduced response to medications and an overall decreased quality of life highlighting a bidirectional correlation between these two entities. There are likely different phenotypes within the obese asthma syndrome: those seen in lean individuals complicated by obesity, disease newly arising in obese individuals and phenotypes worsens by increased environmental pollutants response . Different factors contributing to the syndrome of obesity-related asthma have been hypothesized such as diet, the microbiome, genetic factors, metabolic and immune function , environmental exposures and mechanical effects: reduction in functional residual capacity and expiratory reserve volume . As obese asthma syndrome is a complex and multifactorial entity which is just beginning to be understood further studies should better characterize this disease to understand, in particular, mechanisms conducting to the phenotype of severe and uncontrolled asthma.
Read Also: Edibles And Asthma
Recognizing The Impact Of Obstructive Sleep Apnea In Patients With Asthma
Abstract: The coexistence of asthma and obstructive sleep apnea in a given patient presents a number of diagnostic and treatment challenges. Although the relationship between these 2 diseases is complex, it is clear that risk factors such as obesity, rhinosinusitis, and gastroesophageal reflux disease can complicate both asthma and OSA. In the evaluation of a patient with poorly controlled asthma, it is important to consider the possibility of OSA. The most obvious clues are daytime sleepiness and snoring, but the definitive diagnosis is made by polysomnography. Management of OSA may include weight loss and continuous positive airway pressure . Surgical intervention, such as uvulopalatopharyngoplasty, may be an option for patients who cannot tolerate CPAP. Management may include specific therapies directed at GERD or upper airway disease as well as modification of the patient’s asthma regimen. :423-435)
Obstructive sleep apnea and asthma are both common medical problems.1,2 It is estimated that up to 40 million persons in the United States have OSA, while 17 million have asthma.1-4 Moreover, OSA and asthma may coexist,5 further complicating airway inflammatory pathology and the management of airway disease.
In this article, we will discuss the association between OSA and asthma and the role of certain comorbidities, such as obesity, gastroesophageal reflux disease , nasal obstruction, and rhinosinusitis, that may complicate either or both diseases.
Obesity
Preventing Sleep Apnea And Asthma
In order to do your part towards claiming your life back from sleep apnea and asthma, it is very important to actively manage these conditions. Take your medicine as directed and use your CPAP machine every single night. You should get a minimum of six to eight hours of sleep per night.
Engage in just a few lifestyle changes to improve your overall health.
For example, watch what you eat. Reduce your intake of sugar, carbs, and junk food and instead opt for healthier options like fruit, veggies, nuts , seeds, and whole grains to reduce your weight.
Also, engage in moderate exercise at least three times a week by taking a brisk walk, going for a swim, cycling, or using an elliptical to burn fat, build muscle and strong bones, and reduce stress.
You May Like: Does Asthma Inhalers Cause Weight Gain
How Asthma Contributes To Sleep Apnea
While asthma is normally viewed as a condition that takes place during the day time, symptoms can certainly worsen during the night. When nocturnal asthma occurs, the airways struggle to pull enough oxygen into the lungs and this may cause attacks of coughing, chest tightness, shortness of breath, and wheezing during sleep. As a result, over time the airways may become inflamed and restricted.
You may or may not wake up completely from nocturnal asthma, but as your body fights to restore normal airflow, these interruptions disrupt your normal sleep and prevent your body from getting necessary oxygen and proper rest, very similar to how sleep apnea disrupts restful sleep.; They both can lead to fatigue and poor concentration.
Because severe asthma can cause periods of apnea, or moments during sleep when you stop breathing, it can contribute to low oxygen levels, sleep deprivation, high blood pressure, diabetes, stroke, heart attacks, weight gain, depression, and much more.
Are Gerd And Sleep Apnea Related Or Not
This question appears to have fallen out of fashion in the medical research community. We suspect that this isnt because that line of research was deemed unimportant but rather that a more promising problem to investigate emerged.
Discovering a possible CPAP connection with both OSA and GERD might have been a chance, but at least this technology seems to help some people living with both conditions.
Also Check: How To Prevent Asthma Attacks
Tips To Manage Sleep Apnea
Sleep apnea, sometimes, can be managed by making small lifestyle changes and improving sleeping habits. Here are some ways to manage sleep apnea:
- Avoid stimulants like coffee or tea four to six hours before going to sleep
- Avoid large meals in the evenings
- Avoid alcohol
- Find a good place to sleep peacefully
- Include exercise in your daily routine to lower abdominal fat
Sleep Apnea Is A Comorbidity Of Asthma
People with asthma often suffer from nighttime coughing, wheezing and breathlessness that disturbs their sleep. People with asthma and/or COPD who have a frequent problem waking up at night often have worse respiratory disease. They are also at risk for complications from their asthma or COPD.
Sleep apnea can worsen asthma symptoms throughout the day, increase the need for rescue inhalers, and worsen one’s quality of life. Sleep apnea can be a serious condition by itself. In those with moderate to severe sleep apnea who do not get treatment, their risk for hypertension, heart disease and stroke is increased.
Read Also: Can A Person Get Asthma Later In Life
Asthma And Obstructive Sleep Apnea
Obstructive sleep apnea is a disorder in which the airways narrow or collapse during sleep. Asthma and OSA share similar symptoms and appear to have a bidirectional relationship. This means that having one of these respiratory conditions increases the likelihood of being diagnosed with the other. OSA is particularly common in people with asthma who also snore and those with poorly-controlled asthma symptoms.
People with asthma may find it helpful to talk to their doctors about obstructive sleep apnea. Because asthma puts a person at an increased risk of developing OSA, research suggests that periodic evaluations for OSA may help patients with asthma. Fortunately, treating OSA can often reduce asthma symptoms.
Secondary Service Connection For Sleep Apnea

A secondary service-connected disability is one that results from a condition that is already service-connected.; In claims for secondary service connection, proving a medical nexus is especially important.; With regard to the conditions discussed herein, veterans may be eligible for service connection on a secondary basis for sleep apnea.; That is, if a veteran is service-connected for asthma and later develops sleep apnea, they should subsequently be service-connected for the sleep apnea if they can provide the appropriate medical evidence.
To apply for secondary service connection for sleep apnea, veterans can file a claim the same way they would file an initial claim for service-connected compensation.; They will need to demonstrate the following to VA to be granted secondary service connection for sleep apnea:
- A diagnosis of sleep apnea
- Medical evidence showing the relationship between their service-connected asthma and their sleep apnea
You May Like: Qvar And Weight Gain
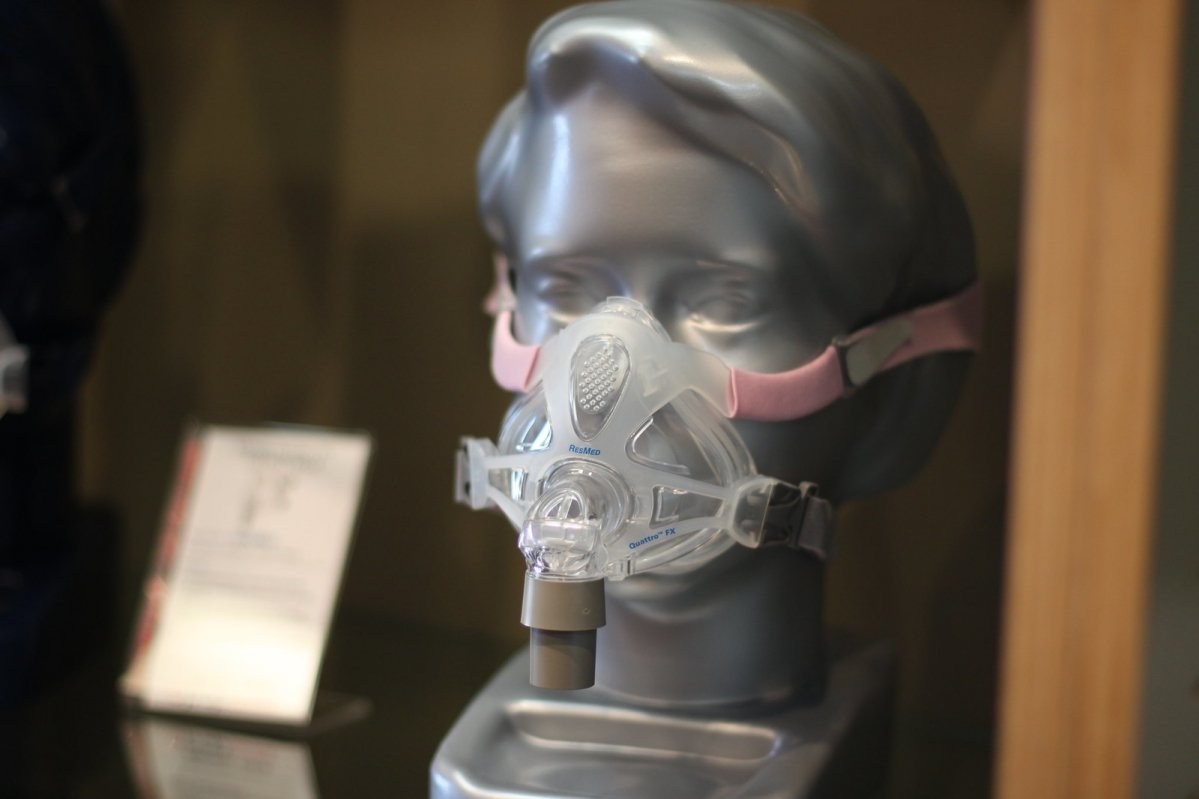
Continuous Positive Airway Pressure
Continuous positive airway pressure is the preferred therapy for obstructive sleep apnea. CPAP involves wearing a mask while sleeping. The mask provides a continuous stream of pressurized air to keep the airways open.
When used with a doctor’s supervision, CPAP seems to reverse many of the harmful effects of sleep apnea. CPAP therapy stabilizes the airway, which means more oxygen to the lungs and decreased contraction of the smooth muscles around the airway.
CPAP therapy also improves acid reflux and lowers inflammatory chemicals in the bloodstream, which may, in turn, reduce inflammation in the body, including the lungs.
Be sure to follow your prescribing physician’s instructions closely, as using CPAP incorrectly can actually cause symptoms to worsen.
What Is The Relationship Between Gerd And Sleep Apnea
A good nights sleep can be a precious commodityespecially for people with untreated sleep apnea, acid reflux, or both. When health conditions such as these routinely interrupt our sleep cycles , a downward spiral can result.
GERD and sleep apnea would seem to be completely unrelated conditions, except that they both disrupt sleep. But is there other information to consider in connecting the two?
The question, are GERD and sleep apnea related? is what were about to discuss here. First, though, lets consider the two conditions independently.
Also Check: What To Do When Someone Has An Asthma Attack
Nocturnal Asthma And Sleep Apnea
Research shows that people with asthma are more likely to develop obstructive sleep apnea .
OSA is a serious sleep-breathing disorder in which mechanical obstruction of the airways during sleep causes repeated pauses in breathing.;These pauses can greatly disrupt blood oxygen levels and lead to sleep fragmentation.
OSA and asthma have overlapping symptoms that can make each condition to differentiate from the other.;
Some clinicians think the similarities are so strong between the two that nocturnal asthma should be considered a sleep-breathing disorder, as it has as serious an impact on sleep as sleep apnea.;
Getting a differential diagnosis is critical; some asthma therapies may, in fact, aggravate an underlying and undetected OSA condition.;
People with either sleep apnea or asthma, who suspect they might have both, may request a referral to a sleep specialist;for testing to rule the other condition in or out. This is useful for finding;appropriate treatments for both conditions.;
How Can We Help
If you are asthmatic and you suspect that you may have developed sleep apnea, we recommend that you come in and see us. We take a holistic approach to treatment and provide solutions that help to restore and improve overall wellness.
If you are diagnosed with a sleep breathing disorder, treatment may include sleep position training, as well as lifestyle guidance like weight reduction and smoking cessation. In some cases, oral appliance therapy may be effective, while continuous positive air pressure is also a common treatment for breathing disorders. The treatment that suits you will depend on your particular case, which is why it is important to begin with a consultation this gives you the opportunity to discuss your concerns in detail and for Dr Acker and his team to address any questions you might have.
To make an appointment, please dont hesitate to get in touch. We are also currently offering free Zoom sessions simply fill out our sleep questionnaire to be eligible for a consult.
To find out more about the services that we offer at Elite Dental of Staten Island, please have a look here. Our team is dedicated to providing world-class care and patient information. We look forward to helping you improve your overall health.
Also Check: Best Painkiller For Asthmatic Patients
What Is The Va Rating For Asthma
Bronchial asthma is rated under VA Diagnostic Code 6602. The ratings under this code vary depending on the asthma disability associated with your condition.;
There is one metric that is used to help classify these ratings. Its known as your;FEV value, which stands for Forced Expiratory volume. In short, FEV-1 measures how much air a person can exhale with a forced breath. Most of the time, physicians will measure the force of the exhale on three different occasions. Do your best on these tests and dont try to fake your breathing problem. They can detect a lot of conditions with these tests and youll need them to be as accurate as possible.
Thus, your FEV-1 value is the amount of air you can exhale in one second. Likewise, your FEV-2 and FEV-3 values specify how much air you exhaled;during the second and third seconds. Your physician may also measure your Forced Vital Capacity, or FVC, to determine the total amount of air that you exhale during your FEV test.
This Firm is So Good at what they do! They are very knowledgeable. They keep you informed. HIRE THEM!
Referencing these values, the VA disability rating;breakdown for asthma is as follows: 10%, 30%, 60% or 100%. Lets take a look at each rating in greater detail.
Increasing Your Va Rating For Asthma With Common Secondary Conditions Like Sleep Apnea
The Centers for Disease Control and Prevention estimates that around;one in three people, or 25 million Americans, have;asthma. Many of those that are veterans have other conditions as well. These are called secondary-connected conditions. ;
Of these adult patients, roughly 50% also suffer from obstructive sleep apnea, or OSA. At the same time, nearly 28% of asthma sufferers are at risk of developing OSA and 20% have some form of sleep-disordered breathing .
If youre a veteran who has both asthma;and;sleep apnea, you could be eligible to receive compensation from the U.S. Department of Veterans Affairs . Take a closer look at the VA rating for asthma, as well as how these two conditions are linked in this article. Well also explain how the presence of a secondary condition can help you earn a higher;VA disability rating, which means more money in your pocket.
You May Like: Does A Chihuahua Take Away Asthma
How Sleep Apnea Contributes To Asthma
When sleep apnea causes you to stop breathing during the night, your body reacts by raising your heart rate and blood pressure, which can result in tossing and turning.; There may also be the backward flow of stomach acid into the esophagus , which can then irritate the lungs if it gets sucked into the throat and airways. This is one reason why it is important to not eat within two to three hours of going to bed, since reflux is less likely to happen on an empty stomach.
As acid reflux burns your throat and airways the lungs may become inflamed, making it more difficult to draw in oxygen. This may also lead to your lungs being overly sensitive and reactive to allergens, fumes, and weather changes, and could result in worsening asthmatic symptoms. It may even lead to uncontrolled asthma that requires more doses of daily and rescue medicines, and that can result in scarring and damage of the lungs.
Sleep deprivation contributes to hypersensitivity to common triggers and can weaken the immune system, creating a cycle of inadequate sleep and poor health.; Sleep apnea can also cause people to wake up with dry mouth, headache, irritability, and feelings of fatigue.
